|
 |
- Search
| Arch Craniofac Surg > Volume 17(2); 2016 > Article |
Abstract
Background
The subciliary approach is commonly used for reconstruction of orbital wall or zygomaticomaxillary fractures. However, this approach is associated with postoperative complications, especially lower eyelid malposition. We report the experience of managing postoperative lower eyelid malposition with triamcinolone acetonide.
Methods
A retrospective review was performed for all traumatic facial fractures requiring surgery via the subciliary approach at Chosun University Hospital in 2014. For each patient meeting inclusion criteria, the medical chart was reviewed for demographic information and postoperative course, including the presence of postoperative eyelid malposition or scleral show.
Results
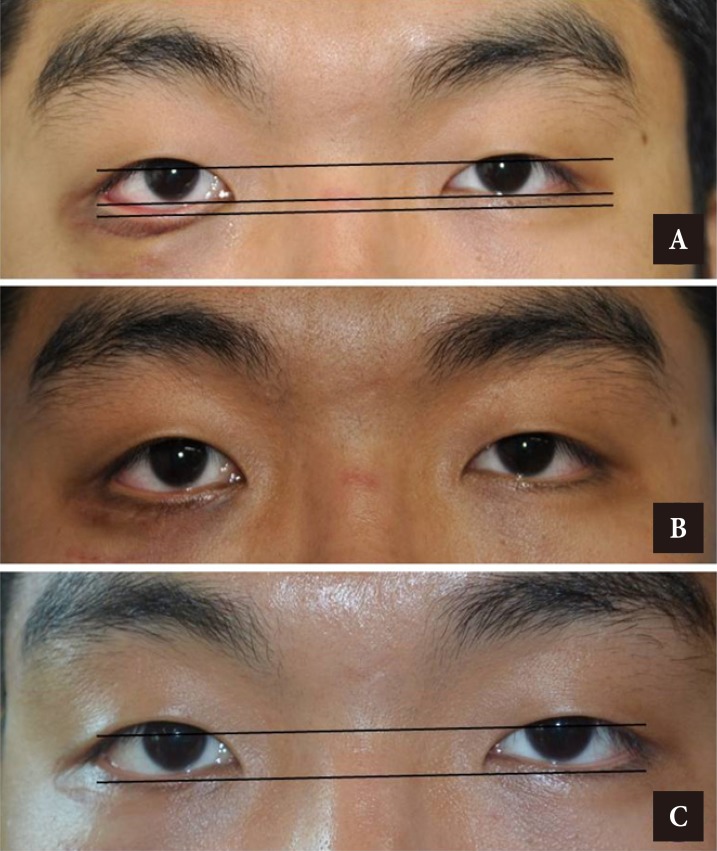
The review identified 189 cases in which the subciliary approach was used, and postoperative lower eyelid malposition was found in 7 cases (3.7%). For these 7 patients, the mean therapeutic period (interval to correction of the malposition) was 10.5 weeks (range, 8 to 14 weeks). On average, patients received 3 injections of triamcinolone. In all cases, degrees of the malposition were improved, and none of the patients required an operative intervention to correct the malposition.
Conclusion
Triamcinolone injection is an appropriate treatment modality for lower eyelid malposition after subciliary approach. Treatment duration is relatively short, requiring fewer than 4 outpatient clinic visits, with relatively earlier recovery compared to conservative "wait-and-see" management.
The surgical approach used to access theorbital wall or zygomaticomaxillary fractures should be short and provide an adequate operative view and easy access to the site of the fracture. Subciliary incision for orbital trauma was first described by Converse [1] in 1944. This approach remains popular because it enables accurate reduction by providing a wide operative view with less scarring [2,3]. However, it is associated with more postoperative complications than transtarsal and transconjunctival approaches [2,4,5,6]. The incidence of postoperative lower eyelid malposition was reported to range from 6.3% to 25% [2,4,6]. The complication causes cosmetic issues as well as multiple ocular symptoms including ocular irritation, photophobia, dry eye, and nocturnal lagophthalmos. Several surgical corrective methods are available for lower eyelid malposition following the subciliary approach [7,8,9], but few studies have examined noninvasive treatment modalities. Considering that ectropion is caused by excessive scar contracture as in the case of trapdoor deformities, we decided to treat patients with lower eyelid malposition after the subciliary approach with triamcinolone acetonide.
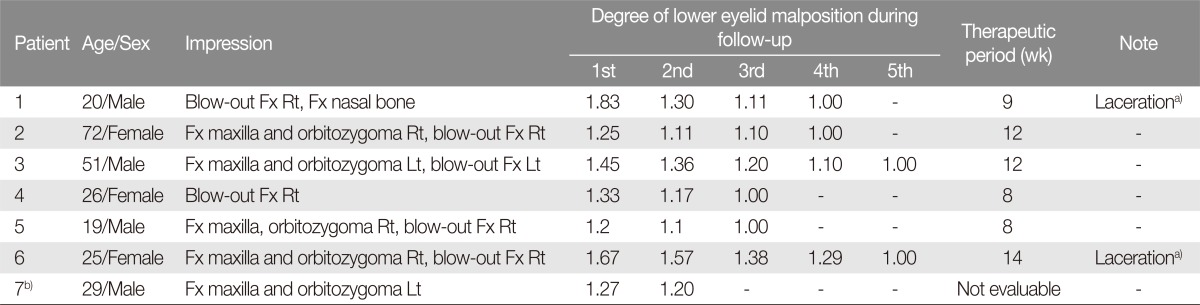
A retrospective review was performed for all traumatic facial fractures requiring surgery via the subciliary approach at Chosun University Hospital in 2014. For each patient meeting inclusion criteria, the medical chart was reviewed for demographic information and postoperative course, including the presence of postoperative eyelid malposition or scleral show. A patient was considered to have lower eyelid malposition if the more of the sclera was visible below the lower margin of the iris when compared to the contralateral side. If the ciliary margin was pulled downwards and had no contact with the bulbar conjunctiva, this was classified as ectropion. The degree of malposition was measured as the ratio of the distance from the corneal light reflex point to the border of the lower eyelid (Fig. 1).
A skin crease several millimeters below the lash line was infiltrated with 1% lidocaine hydrochloride and 1:100,000 epinephrine solution. The incision began at the punctum medially and continued laterally for about 15 mm beyond the lateral canthus. The incision was carried down through the orbicularis muscle and to the orbital septum. The dissection was carried in the preseptal plane to the infraorbital rim, where the periosteum was incised and elevated from the orbital floor. After the orbit was explored and repaired, the periosteum was closed with 5–0 Monosyn sutures. The skin-muscle flap was redraped, and the skin was closed with interrupted 6-0 Ethilon sutures.
Lower eyelid malposition were treated with 4–12 mg of triamcinolone acetonide diluted with 2% lidocaine to a concentration of 20 mg/mL. The steroid was injected only along the postoperative scar, which provided resistance. The injection was strictly limited to the preseptal depth to avoid fat or muscle atrophy. The interval between injections was 3 weeks or longer, and the number of injections depended on clinical status of the ectropion. The degree of malposition was recorded at every follow-up.
We identified 189 cases in which the subciliary approach was used, and postoperative lower eyelid malposition was found in 7 cases (3.7%). The mean age of patients with lower eyelid malposition was 34.5 years, and 4 patients were male. Among the 7 eyelid malposition cases, the subciliary approach was needed for orbital wall fractures in 2 patients and for complex zygomaticomaxillary fractures in 5 patients. As the 2 patients had lacerated wounds in the lower eyelids at the time of injury, the wounds had been closed primarily and incision on /near the closed wounds was followed. One patient stopped treatment during follow-up for personal reasons. The mean therapeutic period (interval to correction of the malposition) was 10.5 weeks (range, 8–14 weeks). The mean frequency of triamcinolone injection was 3 times (Table 1). In all cases, the degree of malposition improved, and none of the patients required operative intervention to correct the malposition (Figs. 2, 3).
Regardless of the approach used to gain access to the orbital floor and zygomaticomaxilla, malposition of the lower eyelid is the most common long-term complication of orbital fracture treatment [4,7,10]. The causes of retraction of the lower eyelid after reconstruction of the orbital floor are multifactorial and may include inadequate skin management with scar retraction (anterior lamellar insufficiency), laxity of the lower eyelid (laxity of the lateral canthal tendon or disinsertion), and middle lamellar inflammation and subsequent scarring. The lower eyelid is supported and suspended by the lateral and medial canthal tendons, capsulopalpebral fascia, tarsus, and orbicularis oculi muscles. It is subdivided into the anterior (skin and orbicularis oculi muscle), middle (orbital septum and orbital fat), and posterior (capsulopalpebral fascia and conjunctiva) lamellae. The orbital septum in the lower eyelid has its origin at the arcus marginalis along the infraorbital rim and inserts into the capsulopalpebral fascia or lower eyelid retractors about 5 mm below the inferior tarsal border [8]. Any event, either iatrogenic or traumatic, that contributes to contracture of the orbital septum will cause the lower eyelid to be pull down from its normal position [7,8].
Various methods are available to correct postoperative lower eyelid malposition. Salgarelli et al. [7] used the tarsal strip technique, while Patipa [8] reported the use of methods such as lateral canthal tendon tightening, spacer graft, and midface lifting. These procedures involved excessive removal of soft tissues such as skin, muscle, or fat during the primary operation, or the patients had inappropriate anatomical repositioning. For the subciliary approach to reconstruction of facial bone fracture; however, the authors believed that non-operative scar managementwould be adequate to correct malposition of the lower eyelid, because subciliary approach does not cause soft tissue defects and avoids inappropriate anatomical reposition through the fine surgical techniques used during operation.
The efficacy of corticosteroid injections in the treatment of scars has been well established, and the most commonly used corticosteroid is triamcinolone [11]. This corticosteroid inhibits alpha 2-macroglobulin, which in turn inhibits collagenase. Once this pathway is blocked, collagenases are activated, which facilitates collagen degeneration [12]. Furthermore, injecting triamcinolone along with lidocaine greatly reduces the pain of injection, enabling patients to tolerate multiple needle pricks. Local complications of triamcinolone injections include atrophy of normal adjacent skin, depigmentation, hyperpigmentation, and telangiectasia. Systemic complications include weight gain, diabetes, and Cushing's syndrome. In our study, no triamcinolone-related complications had occurred because of the long injection interval and small doses of triamcinolone used.
Several studies have reported malposition of the lower eyelid after the subciliary approach. Ridgway et al. [6] reported 7 cases (12.5%) of ectropion after the subciliary approach, among whom 1 patient (1.8%) required operative management. Furthermore, Rohrich et al. [2] found that the incidences of ectropion and scleral show were 6.3% and 18.8%, respectively, while Appling et al. [5] reported 3 cases (12%) of ectropion and 7 (28%) of scleral show after the subciliary approach. All these patients responded to massage with, or injection of, triamcinolone. Burm et al. [13] found 3 cases (1.4%) of ectropion and 3 (1.4%) of scleral show after the subciliary approach, and all these patients recovered with massage with and injection of triamcinolone within 3–15 months. In the present study, 2 patients (1.1%) with ectropion and 5 patients (2.6%) with scleral show recovered without surgical correction.
The incidence of postoperative malposition of the lower eyelid in the present study was 3.7%, which is remarkably lower than the rates reported in previous studies [2,4]. This can be attributed to the efforts undertaken to reduce the incidence of scar contracture. Damage to the orbicularis oculi and orbital septum was minimized be ensuring fine cutaneous incision during surgery, and by avoiding excessive traction, damage to the margins caused by the retractor was avoided. An anti-inflammatory drug (Seronase, Reyon Pharm. Co., Seoul, Korea) was administered after surgery to shorten the inflammatory phase of wound healing and thereby reduce scar formation. Furthermore, hematoma occurrence was minimized by using compression dressing and ice packs over the subciliary area.
Few studies have examined conservative therapy for postoperative malposition of the lower eyelid. The use of triamcinolone has been mentioned in passing for conservative therapy [4,13]. The patients in the study by Burm et al. [13] took 3 to 12 months to completely recover from postoperative malposition of the lower eyelid, while the mean recovery period of in the present study was only 10.5 weeks. This finding indicated that scar management using triamcinolone injection can shorten the period required for nonsurgical correction of postoperative lower eyelid malposition.
In conclusion, lower eyelid malposition, a common complication of the subciliary approach for treatment of orbital and zygomaticomaxillary fractures, can be managed non-operatively using triamcinolone injections.The method is safe and effective and avoids the need for operative interventions.
References
1. Converse J. Two plastic operations for repair of orbit following severe trauma and extensive comminuted fracture. Arch Ophthalmol 1944;31:323-325.

2. Rohrich RJ, Janis JE, Adams WP Jr. Subciliary versus subtarsal approaches to orbitozygomatic fractures. Plast Reconstr Surg 2003;111:1708-1714. PMID: 12655219.


3. Yun CS, Kim JH, Yang HJ. The usability of infraorbital approach on the patients with orbito-zygomatic fracture. J Korean Cleft Palate-Craniofac Assoc 2009;10:19-22.
4. Bahr W, Bagambisa FB, Schlegel G, Schilli W. Comparison of transcutaneous incisions used for exposure of the infraorbital rim and orbital floor: a retrospective study. Plast Reconstr Surg 1992;90:585-591. PMID: 1409993.


5. Appling WD, Patrinely JR, Salzer TA. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg 1993;119:1000-1007. PMID: 8357580.


6. Ridgway EB, Chen C, Colakoglu S, Gautam S, Lee BT. The incidence of lower eyelid malposition after facial fracture repair: a retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast Reconstr Surg 2009;124:1578-1586. PMID: 20009844.


7. Salgarelli AC, Bellini P, Multinu A, Landini B, Consolo U. Tarsal strip technique for correction of malposition of the lower eyelid after treatment of orbital trauma. Br J Oral Maxillofac Surg 2009;47:298-301. PMID: 19303178.


8. Patipa M. The evaluation and management of lower eyelid retraction following cosmetic surgery. Plast Reconstr Surg 2000;106:438-453. PMID: 10946945.


9. Goldberg RA, Lee S, Jayasundera T, Tsirbas A, Douglas RS, McCann JD. Treatment of lower eyelid retraction by expansion of the lower eyelid with hyaluronic Acid gel. Ophthal Plast Reconstr Surg 2007;23:343-348.


10. Holtmann B, Wray RC, Little AG. A randomized comparison of four incisions for orbital fractures. Plast Reconstr Surg 1981;67:731-737. PMID: 7243973.


11. Khan MA, Bashir MM, Khan FA. Intralesional triamcinolone alone and in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. J Pak Med Assoc 2014;64:1003-1007. PMID: 25823177.

12. Kelly AP. Medical and surgical therapies for keloids. Dermatol Ther 2004;17:212-218. PMID: 15113289.


13. Burm JS, Kim BY, Kim YW. Prevention of lower eyelid complications caused by a subciliary approach: temporary lower eyelid suspension. J Korean Soc Plast Reconstr Surg 2006;33:465-468.
Fig. 1
Degree of lower eyelid malposition measured by the ratio of the distance from the corneal light reflex point to the border of the lower eyelid between the side with ectropion A and the normal side B.
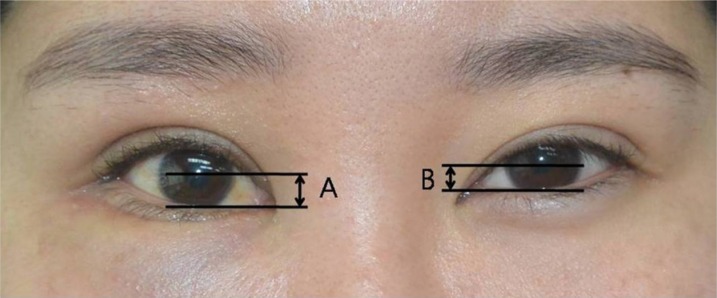
Fig. 2
(A-C) A 20-year-old man with a right-sided blow-out fracture was treated via the subciliary approach. Photographs from the sequential follow-up visits.
- TOOLS
-
METRICS

-
- 4 Crossref
- Scopus
- 5,203 View
- 71 Download
- Related articles in ACFS