 |
 |
- Search
| Arch Craniofac Surg > Volume 23(4); 2022 > Article |
|
Abstract
Postoperative temporal hollowing is a common complication of craniotomy. Damage and repositioning of the temporalis muscle can lead to a depression in the temporal side of the skull with inferior bulging, worsening aesthetic outcomes. We report a case of cranioplasty with three-dimensional (3D) printed mesh involving an additional correction using a temporalis muscle sling to help address this problem. A 3D-printed bioabsorbable mesh was prepared based on preoperative facial computed tomography, and was fixed to the hollowed area for tissue augmentation. The temporalis muscle was elevated and fanned out to its original position, and a sling was attached to a screw that was fixed to the mesh. For reinforcement, an additional sling was attached to another screw fixed to the mesh 2–3 cm vertically above the first screw. Aesthetic results were confirmed immediately after surgery and later during outpatient follow-up. Both depression and lateral bulging were resolved, and there was no delayed drooping of the temporalis muscle on 6-month follow-up. There were no complications, and the patient was satisfied with the appearance. This is a simple yet effective technique with a low risk of complications, and should be considered for postoperative temporal hollowing patients, especially those with severe lateral bulging.
As neurosurgical and craniofacial techniques advance, reducing morbidity and postoperative facial deformities with consideration of aesthetic results are becoming increasingly important concerns [1,2].
The temporalis muscle is one of the mastication muscles and has the shape of a broad fan. It arises from the temporal fossa and the deep temporal fascia, and inserts to the coronoid process of the mandible, covering the temporal bone. When performing a craniotomy, the surgeon usually has to cut a part of this muscle, and the original position and function are lost [3,4].
During craniotomy, elevation of the temporalis muscle and inadequate re-suspension can lead to temporal hollowing [5]. Following this temporal hollowing, due to drooping of the temporalis muscle, inferior lateral bulging can also occur [6]. Craniotomy can lead to temporalis muscle atrophy due to nerve, vessel, or direct injuries [7]. This causes significant facial deformities with poor aesthetic outcome and patient dissatisfaction.
New techniques are being used to address this problem. Van Kouwenberg et al. [8] suggested a buried anchoring suture in the temporal hair-bearing scalp in 2019, but this was done a few months after cranioplasty. Park et al. [9] suggested a method of placing the three-dimensional (3D) printed implant between the superficial and deep layers of the temporalis muscle to improve esthetic outcomes in 2019. Kim et al. [10] reported three cases of satisfying outcomes using silicone implants made with a toy-clay model.
We suggest a simple suture sling technique to help resolve this problem. The 3D implant is applied using the conventional method [11], and since the original soft tissue or skull is augmented with a 3D mesh, the muscle origin has to be predicted and the sling has to be fixed at this predicted spot on the 3D mesh. This technique is easily applicable and effectively addresses temporal hollowing and lateral bulging.
In the supine position, an incision was made on the previous craniotomy scar to minimize additional scarring. Exposure of the skull around the hollowed area and the upper portion of the temporalis muscle was achieved. Dissection and elevation of the temporalis muscle was performed. The muscle was displaced downward and partially overlapped, resulting in the lateral bulging. Thus, the adhesion was dissected and the muscle was spread and pulled upward towards its original anatomical position.
A 3D-printed bioresorbable mesh that was prepared in advance was inserted at the targeted hollow area. It was positioned between the skull and temporalis muscle, and fixed with titanium screws onto the skull. A large bite with #3-0 nylon was made on the superior portion of the temporalis muscle, and both ends of the string were wrapped around a titanium screw that was fixed to the mesh. Using the remaining ends of the same string for reinforcement, an additional sling was tied to another screw fixed to the mesh 2 to 3 cm vertically above the first screw (Fig. 1). The position of the second screw was around the uppermost boundary of the temporal fossa from which the temporalis muscle is supposed to arise from. When adequate aesthetic results were noted, the skin was closed.
3D-printed bioresorbable mesh (T&R Biofab, Siheung, Korea) with a thickness of 0.15 to 30 mm was used. The design was obtained via conversion of DICOM files of computed tomography (CT) scans, and fabricated by a 3D printer. The mesh has a porous structure that allows the surrounding tissues to migrate into, and later promotes the generation of extracellular matrix material (Fig. 2).
At the age of 21, a female patient underwent craniectomy due to an epidermoid tumor in the left basal and cerebellopontine angle cisterns. Six years later, the patient visited our outpatient department. The patient’s temporalis muscle was retracted, and it resulted in a very noticeable temporal hollowing with inferior lateral bulging (Fig. 3). Preoperative facial CT scan also showed depression of the left temporal area of the skull.
The patient underwent cranioplasty with the anchoring suture method described above. A large bite was made on the temporalis muscle with #3-0 nylon, and a sling was created and fixed vertically on a 6-mm titanium screw attached on the 3D mesh, and another vertical sling was fixed on another 6-mm titanium screw 3 cm above the first screw (Fig. 4). Adequate lengthening and suspension of the temporalis muscle was achieved, and the anchored screw and suture slings were non-palpable through the skin.
The patient showed no other postoperative complications such as seroma, hematoma, wound dehiscence, or infection. One drain was inserted and was removed in about 2 weeks, and the patient was discharged. One month after surgery, 50 units of botulinum toxin were injected into the temporal region. This was done to achieve muscle atrophy due to the patient’s persistent swelling, and also to weaken the muscle to prevent the screws and nylon sling from deviating as the mesh is absorbed. Correction of the deformity was achieved, and visually normal contour was maintained 6 months after surgery (Fig. 5). The patient was also satisfied with the aesthetic results.
Bi-temporal length measured from the facial CT showed a near symmetrical shape on both sides. Four levels (superior, lower superior, upper inferior, and inferior) were selected and compared. Before the operation, superior measurements were longer on the normal right side, and the most inferior measurement was longer on the abnormal left side. After the operation, a 1-week follow-up CT scan showed a much more symmetrical shape. Each measurement was similarly 4–5 mm longer on the left, operative side (Table 1, Fig. 6).
Temporal hollowing is a common complication of craniectomy that worsens aesthetic outcomes. Multiple treatment plans have been implemented, including a 3D implant to make up for the loss in tissue, repositioning of the temporalis muscle, and microfat graft [12,13]. Soft tissue fixation to bone itself is a basic technique especially in orthopedic surgeries, and suture anchors have been developed for this purpose [14]. However, this has not been commonly used in cranioplasty, and we suggest a simple method to address this lateral bulging with a temporalis muscle sling.
There are several advantages to our procedure. First, it is a simple yet effective technique that is easily applicable with a short learning curve. Cranioplasty is performed in the conventional way, and the temporalis muscle is quite superficial, leading to easy access and visual confirmation of its original position. The results can be predicted during the operation by visualization after repositioning the scalp flap. Second, no other special materials or tools are needed. A pre-designed 3D mesh is required, but this is required in most cranioplasty surgeries. For the additional suture anchoring technique, only a simple nylon suture with a few titanium screws are needed, and these are materials that are already used in conventional surgery. Third, there were no noted complications, and we believe that no additional complications will arise from our muscle sling procedure. Previous reports show overall complication rates of cranioplasty ranging from 25.9% to 33.8%, with infection rates from 6.6% to 14.9% [15]. Due to minimal differences from the conventional cranioplasty method, complication rates are thought to be similar.
There have been previous reports of similar suture anchoring techniques, but poor results occurred due to osteolysis around the anchored sutures [16]. In our case, there was minimal bony defect and the absorbable mesh was used for soft tissue augmentation. It was mainly used to compensate for muscle and soft tissue loss caused by atrophy. The mesh is thought to be absorbed in about 2 to 3 years. During that period, we believe that there will not be many changes in the anchored area as the tissue around the implant becomes fixed with adhesion, scarring or capsule formation.
In our illustrative case, CT scans showed that preoperative length was longer on the normal right side at the superior, lower superior, and upper inferior levels, and was longer on the affected left side at the inferior level, thus showing a concave and convex shape aligned with the temporal hollowing with inferior bulging. Next, postoperative length was longer on the affected left side at all levels, and the difference in length was quite constant; 5.5% to 6.3%. This over-correction of the surgical side seems to be caused by soft tissue swelling after surgery, and is expected to improve with time.
Additional contouring can be done postoperatively if needed. Botulinum toxin has been widely used for aesthetic purposes [17]. As we have explained in our illustrative case, muscle swelling with scarring and adhesion was seen, and botulinum toxin injection was done to decrease muscle volume. It is also thought to help keep the screws and nylon sling in its original position by weakening the muscle. Liposuction and autologous fat grafting have also been widely used in reconstruction and soft tissue augmentation, and recent research with the addition of adipose-derived stem cells are showing greater results [18].
There are limitations to our study. Due to the short follow-up period, long-term complications could not be confirmed. Also, it was not possible to confirm the change of state after the mesh was completely absorbed, and long-term CT scan follow-up could not be confirmed. However, since the mesh has a porous structure in which the tissue migrates into, it is expected that the screw and sling stay sufficiently fixed even after mesh absorption. The aesthetic results were acceptable after 6 months, but confirmation is needed after a longer period of time.
In conclusion, we believe that this simple suture anchoring technique will be useful to other plastic and neurosurgeons when performing cranioplasty, and should be considered for patients with postoperative temporal hollowing, especially those with severe lateral bulging. No additional complications were noted, but longer follow-up is thought to be needed.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (IRB No. 1-2022-0765).
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Author contribution
Conceptualization: Jae Hyeok Choi, Tai Suk Roh, Won Jai Lee, Wooyeol Baek. Formal analysis: Jae Hyeok Choi. Methodology: Jae Hyeok Choi, Tai Suk Roh. Project administration: Wooyeol Baek. Visualization: Wooyeol Baek. Writing - original draft: Jae Hyeok Choi. Writing - review & editing: Won Jai Lee, Wooyeol Baek. Investigation: Jae Hyeok Choi. Supervision: Tai Suk Roh, Won Jai Lee, Wooyeol Baek Validation: Tai Suk Roh, Won Jai Lee.
Fig. 1
Schematic diagram of the surgical technique. (A) Showing temporal hollowing with inferior lateral bulging due to craniectomy and displaced temporalis muscle. (B) Showing corrected soft tissue contour after cranioplasty with muscle sling, black dots depicting screws and black lines depicting nylon sling.
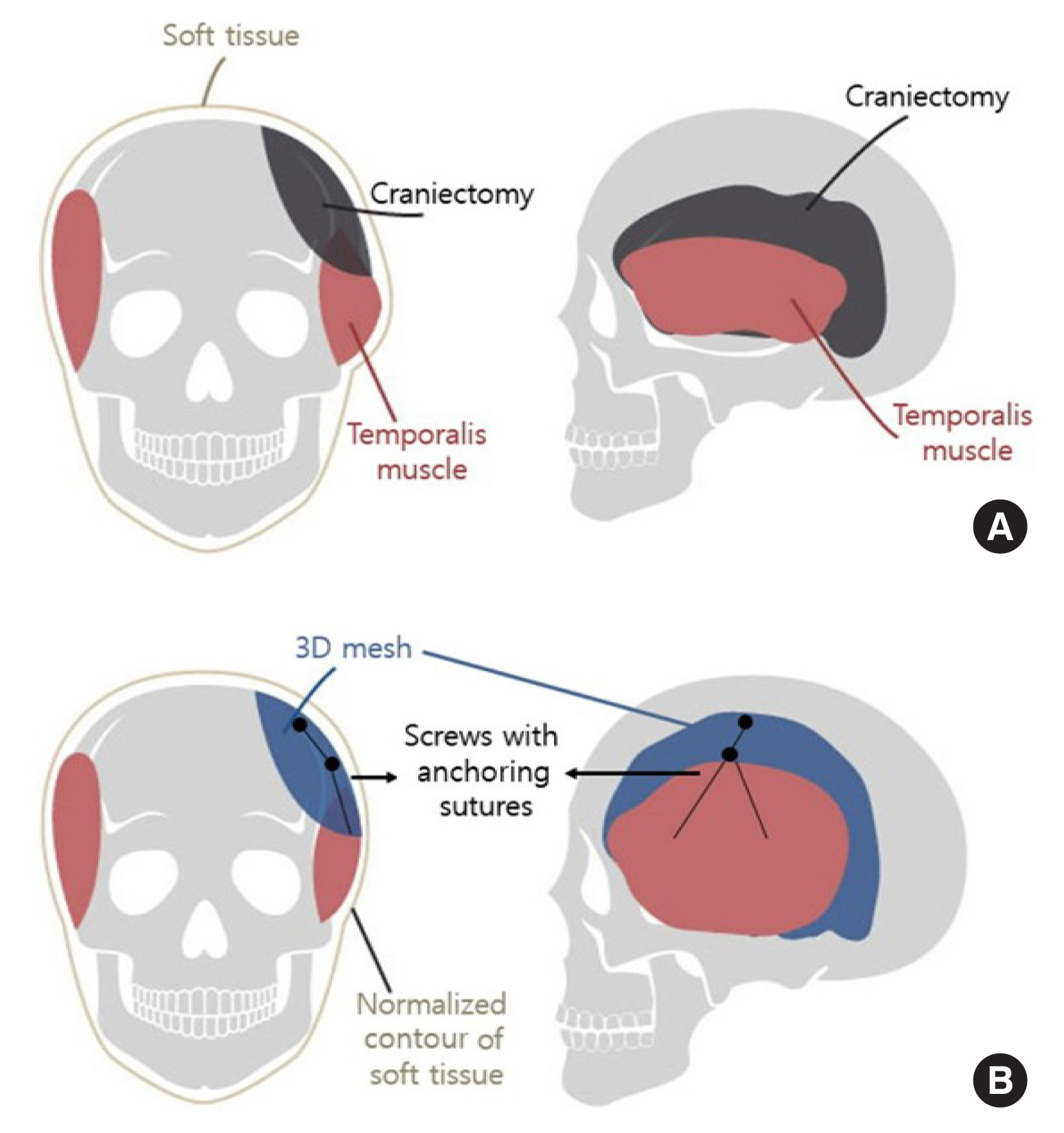
Fig. 3
Preoperative state after craniectomy and before cranioplasty, showing left temporal hollowing with inferior lateral bulging.
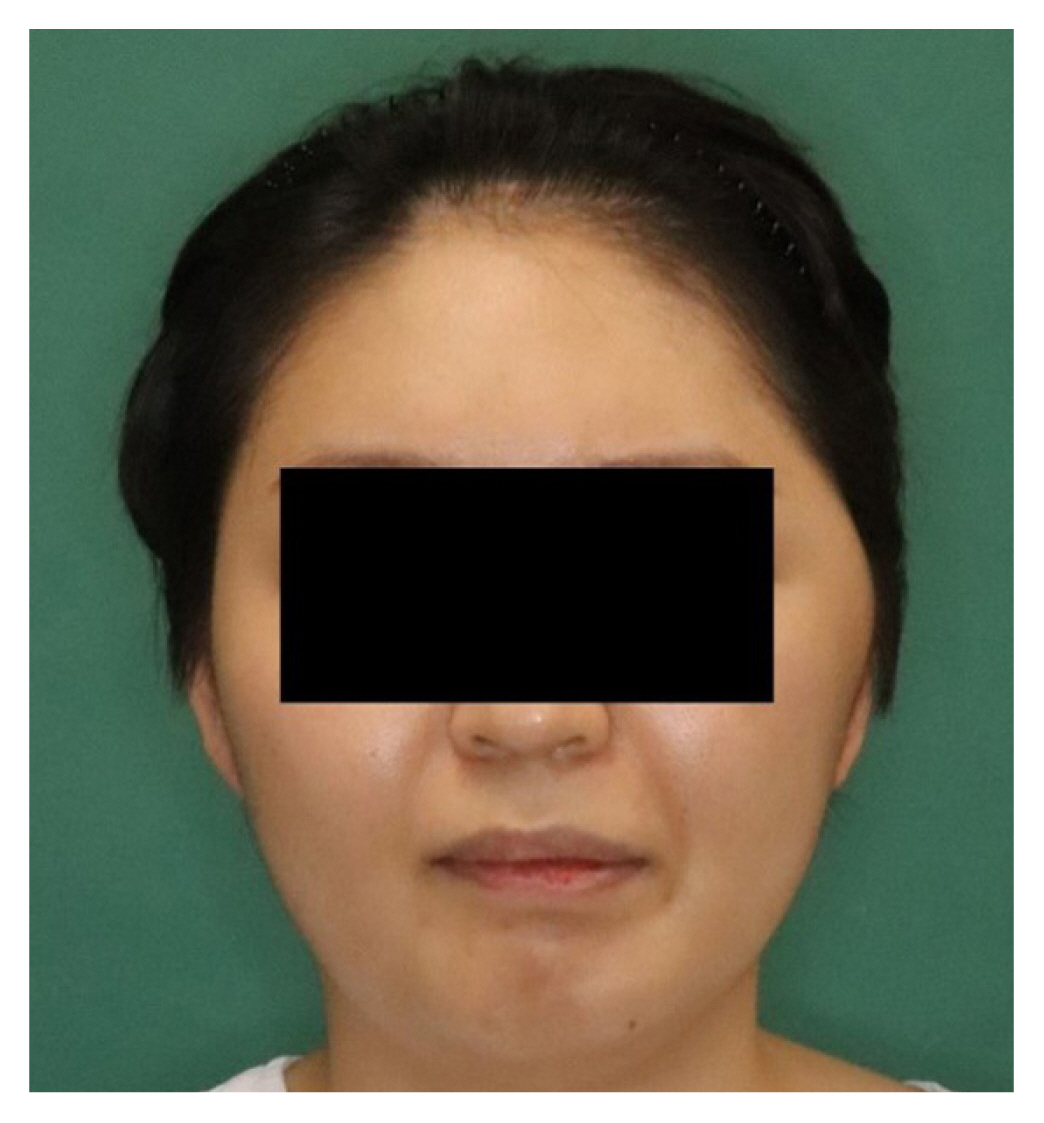
Fig. 4
Intraoperative photograph showing the three-dimensional (3D) mesh with the temporalis muscle nylon anchoring sling. A large bite is made on the temporalis muscle and both ends of the string were fixed on a 6 mm titanium screw that is fixed on the 3D mesh, and another vertically strengthening sling is tied on another 6 mm titanium screw that is also fixed on the 3D mesh.
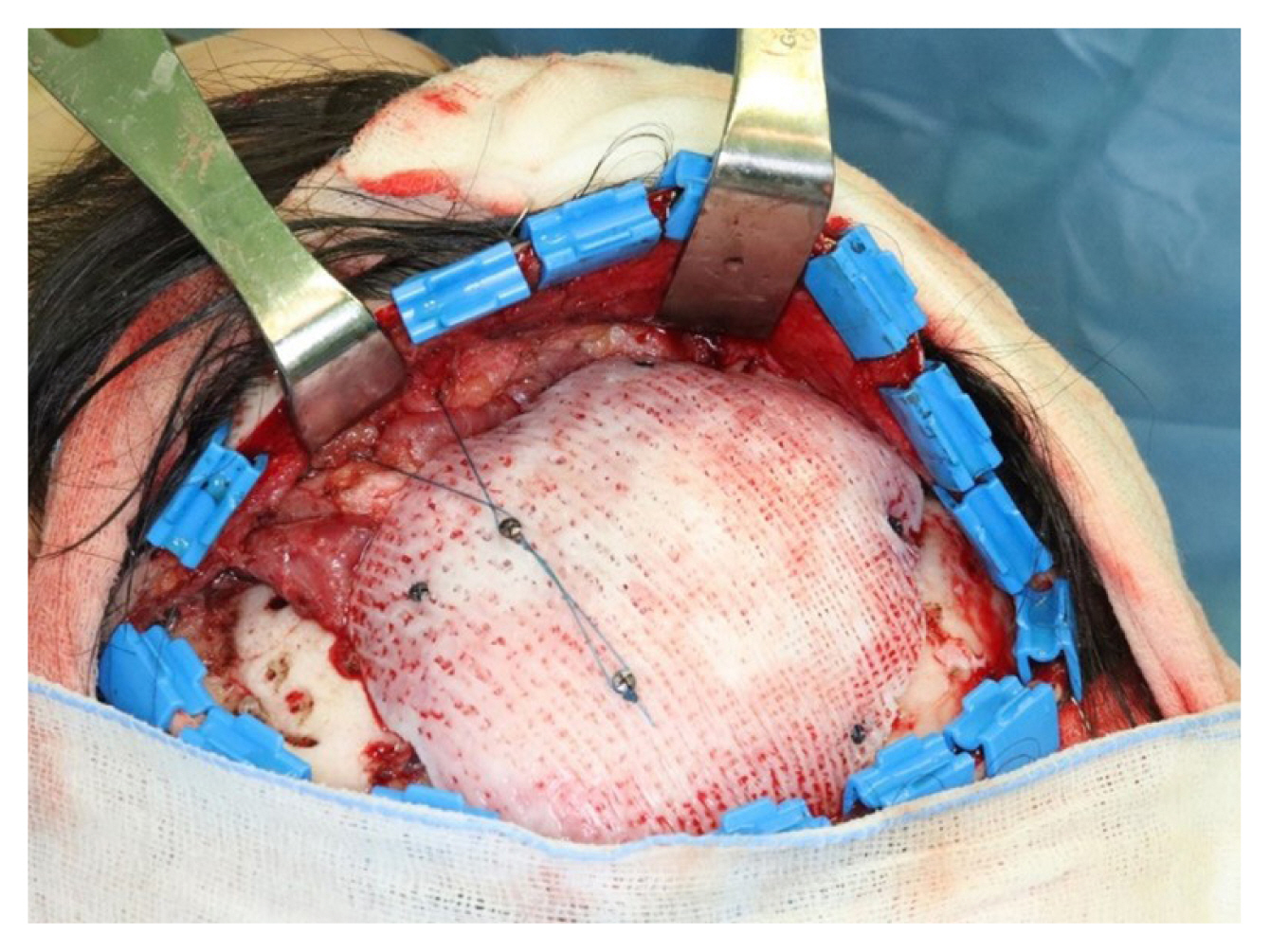
Fig. 5
Postoperative state 6 months after the surgery, showing resolved left temporal hollowing with inferior lateral bulging.

Fig. 6
Bi-temporal length measured from the facial computed tomography. (A) Preoperative state showing temporal hollowing with inferior bulging; superior measurements showing longer distance on the normal right side, and inferior measurement showing longer distance on the abnormal left side. (B) Postoperative state showing resolved temporal hollowing and inferior bulging; each measurement showing a similar 4–5 mm longer distance on the surgical left side.
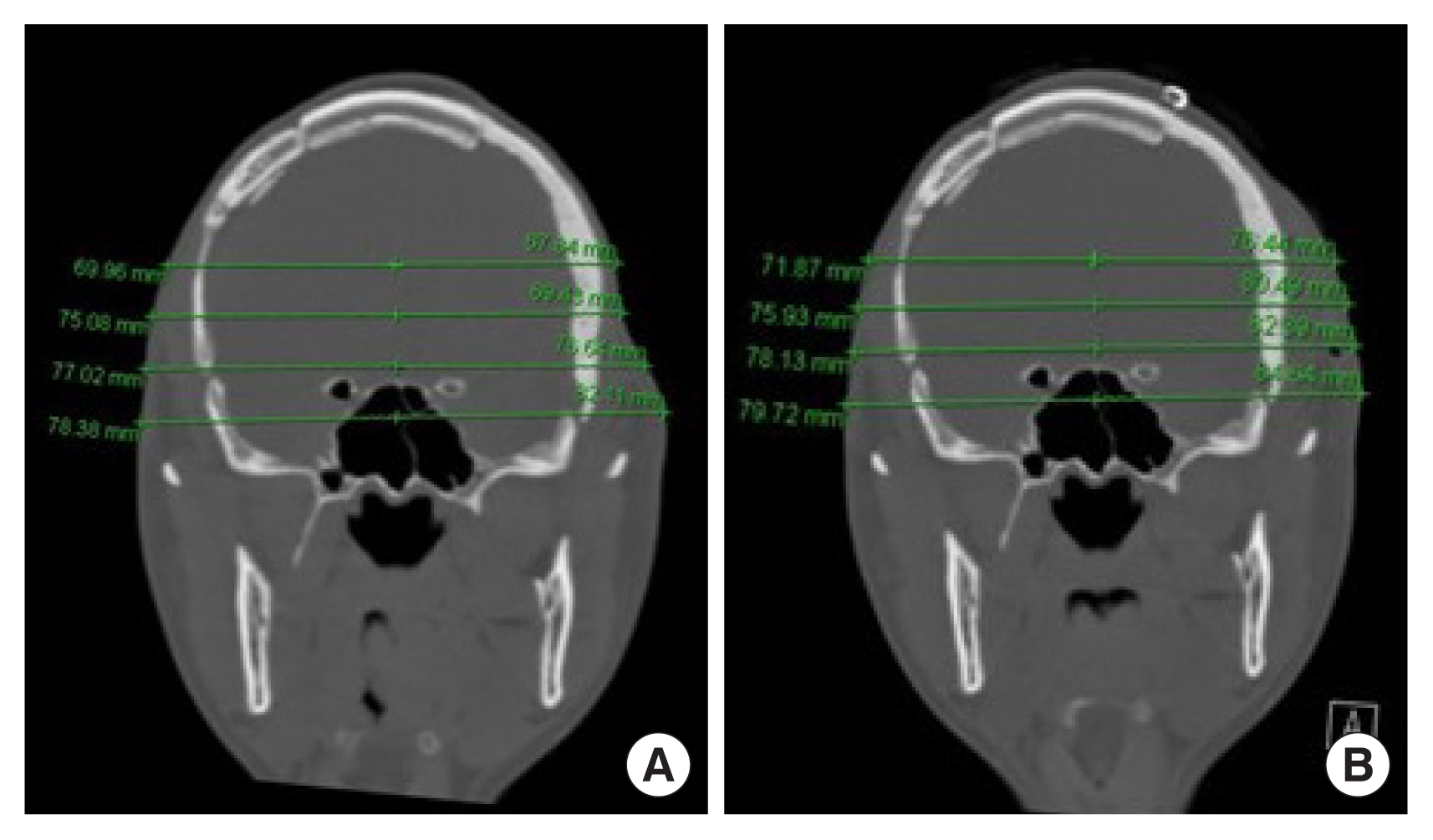
Table 1
Difference in length of operative and non-operative sides
REFERENCES
2. Zhong S, Huang GJ, Susarla SM, Swanson EW, Huang J, Gordon CR. Quantitative analysis of dual-purpose, patient-specific craniofacial implants for correction of temporal deformity. Neurosurgery 2015;11(Suppl 2):220-9.


3. van der Meulen JJ, Willemsen J, van der Vlugt J, Nazir PR, Hilling D, Mathijssen IM, et al. On the origin of bitemporal hollowing. J Craniofac Surg 2009;20:752-6.


4. Vaca EE, Purnell CA, Gosain AK, Alghoul MS. Postoperative temporal hollowing: is there a surgical approach that prevents this complication? A systematic review and anatomic illustration. J Plast Reconstr Aesthet Surg 2017;70:401-15.


5. Park G, Kim J, Chang C, Jung Y. Pre-planned cranioplasty using computer-assisted designed temporalis muscle augmentation in patients with decompressive craniectomy involving resection of the temporalis muscle. J Craniofac Surg 2021;32:e60-2.


6. Kadri PA, Al-Mefty O. The anatomical basis for surgical preservation of temporal muscle. J Neurosurg 2004;100:517-22.


7. Oikawa S, Mizuno M, Muraoka S, Kobayashi S. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy: technical note. J Neurosurg 1996;84:297-9.


8. Van Kouwenberg E, Kotamarti V, Reinhardt M, Adetayo OA. Cranial suture anchor temporalis resuspension: a new technique to reconstruct temporal hollowing after craniotomy. J Craniofac Surg 2019;30:1696-9.


9. Park SE, Park EK, Shim KW, Kim DS. Modified cranioplasty technique using 3-dimensional printed implants in preventing temporalis muscle hollowing. World Neurosurg 2019;126:e1160-8.


10. Kim MW, Kim SH, Nam SB, Lee JW, Jeong DK, Kim YH. Reconstruction of temporal hollowing deformities using silicone implants made using a toy-clay model: a report of three cases. Arch Craniofac Surg 2022;23:34-8.




11. Park EK, Lim JY, Yun IS, Kim JS, Woo SH, Kim DS, et al. Cranioplasty enhanced by three-dimensional printing: custom-made three-dimensional-printed titanium implants for skull defects. J Craniofac Surg 2016;27:943-9.


12. Choi J, Choi H, Shin D, Kim J, Lee M, Kim S, et al. Autogenous fat grafting for mild-to-moderate postoperative temporal hollowing after decompressive craniectomy: one-year follow-up. Arch Plast Surg 2018;45:69-73.




13. Yoon HG, Ko Y, Kim YS, Bak KH, Chun HJ, Na MK, et al. Efficacy of 3D-printed titanium mesh-type patient-specific implant for cranioplasty. Korean J Neurotrauma 2021;17:91-9.




14. Goble EM, Somers WK, Clark R, Olsen RE. The development of suture anchors for use in soft tissue fixation to bone. Am J Sports Med 1994;22:236-9.



15. Zanaty M, Chalouhi N, Starke RM, Clark SW, Bovenzi CD, Saigh M, et al. Complications following cranioplasty: incidence and predictors in 348 cases. J Neurosurg 2015;123:182-8.


16. Park HB, Keyurapan E, Gill HS, Selhi HS, McFarland EG. Suture anchors and tacks for shoulder surgery, part II: the prevention and treatment of complications. Am J Sports Med 2006;34:136-44.



- TOOLS
-
METRICS

-
- 4 Crossref
- Scopus
- 2,613 View
- 68 Download
- Related articles in ACFS







