INTRODUCTION
Personal mobility devices (PMDs) have become an increasingly popular transport modality globally as they help travel long distances and provide an environmentally friendly alternative to motor vehicles given their low energy consumption [
1,
2]. To reduce traffic volumes in urban settings and to increase PMD accessibility, e-bike and e-scooter rental services have been introduced in various cities worldwide.
The Global Industry Analysts Incorporated reported that amid the coronavirus disease 2019 crisis, the global market for PMDs was estimated at USD 11.2 billion in the year 2020, and is projected to reach a revised size of USD 16.1 billion by 2027 [
3]. The Korean Ministry of Land, Infrastructure and Transport reported that in Korea, approximately 60,000 PMDs were sold in 2016, approximately 75,000 were sold in 2017 (a 20% increase), and forecast that approximately 200,000 PMDs are likely to be sold in 2022 in the rapidly growing Korean PMD market [
4]. Consequently, PMD-related accidents have also increased in Korea at an average annual rate of 47.4%. The Consumer Injury Surveillance System of Korea Consumer Agency reported that the number of PMD-related accidents has steadily increased since 2013, with a significant increase from 26 such accidents in 2015 to 571 in 2020 [
5].
During the coronavirus pandemic, outdoor activities and facial injuries have been decreased, thereby reducing the burden on plastic surgeons [
6,
7]. Nevertheless, the number of individuals visiting emergency departments (EDs) with PMD-related injuries has increased annually, causing increasing social interest in and demand for PMDs. Several studies have analyzed patients admitted to the ED for PMD-related accidents [
8,
9]. Boniface et al. [
8] analyzed the medical records of patients who had been admitted to a local ED for PMD-related accidents between 2005 and 2008. Trivedi et al. [
9] undertook a retrospective study, analyzing the medical records of 228 patients admitted to the EDs at two hospitals in Southern California in relation to accidents involving standing e-scooters between September 2017 and August 2018. While these studies analyzed data regarding patients admitted to the ED for PMD-related accidents and the overall types of accidents and risks involved, studies concerning the health and financial costs of facial injuries are lacking. Facial injuries appear to be the most common PMD-related injury, with plastic surgery increasingly involved.
This study aimed to evaluate characteristics of injury patterns and treatment costs for patients treated in the department of plastic surgery in a trauma center. The study findings may help create a framework for raising safety awareness concerning PMD use and establish relevant safety laws and regulations in the future.
METHODS
The study was approved by the Institutional Review Board of Dankook University Hospital (IRB No. 2022-06-047) and performed in accordance with the principles of the Declaration of Helsinki. The informed consent was waived because this study design is a retrospective review.
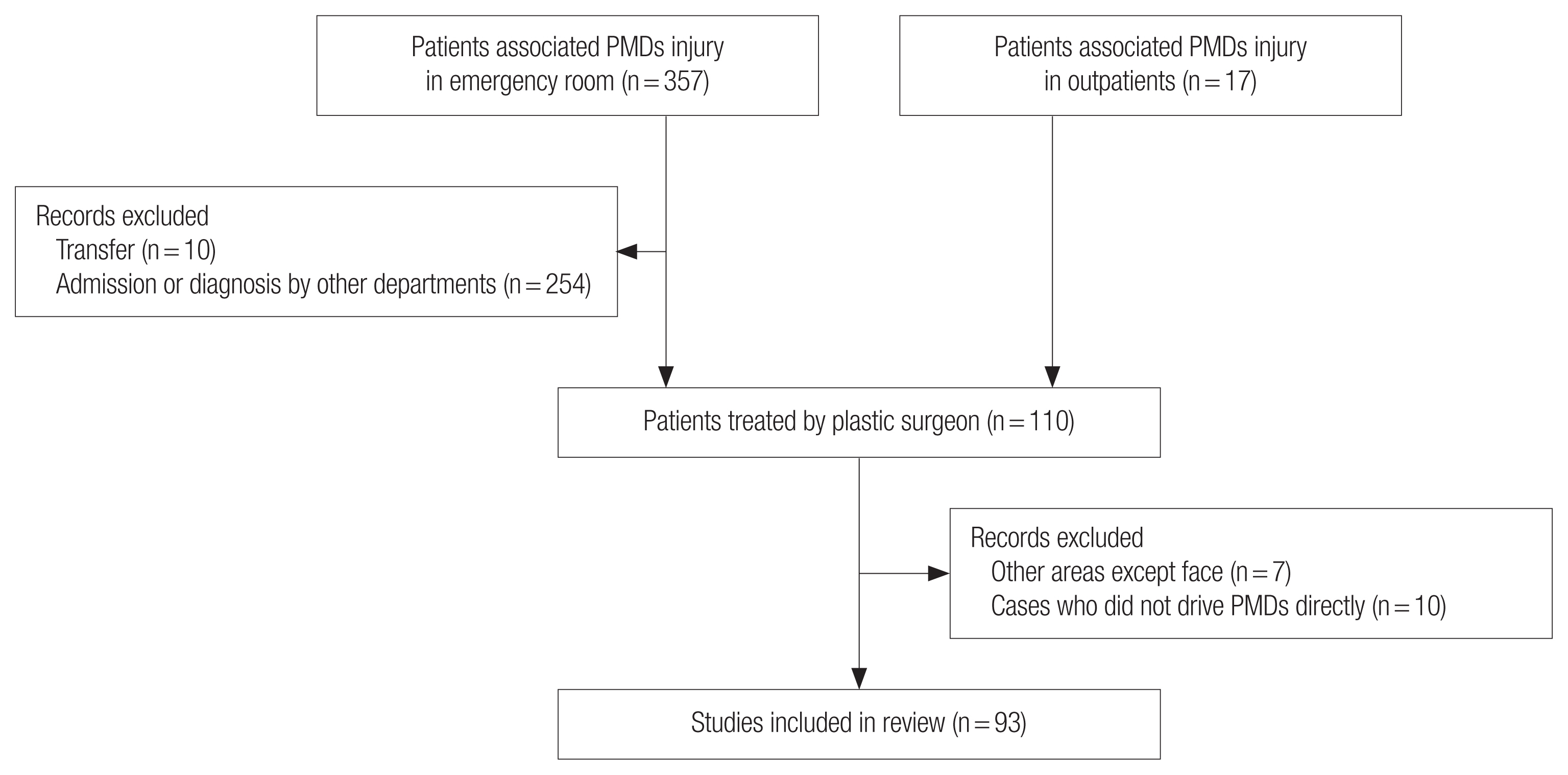
In this retrospective study, data concerning patients treated at our hospital for PMD-related injuries from January 2017 to December 2021 were reviewed. Inclusion criteria comprised admission to the ED or to the plastic specialist outpatient clinic for PMD-related injuries. Exclusion criteria comprised admission to other specialty services for PMD-related injuries, death, or transferral to other hospitals. We additionally excluded patients with injuries to areas other than the face and injured patients who had been passengers at the time of the accident. Of the patients admitted to the ED, we excluded 10 patients who were transferred to another hospital and 254 patients who had been treated by or admitted to another department. Additionally, seven patients with non-facial injuries and 10 patients who were passengers were also excluded (
Fig. 1).
All patient data were retrieved from the Trauma Registry System of our institution. Data included age, sex, alcohol consumption, helmet use, the type of impact, onset of injury (hour, month, and year), place of first visit, type of injury, admission status (general ward or intensive care unit), operation status, and cost. For the onset of injury, the 24-hour period was divided into four 6-hour intervals, and the 12-month period was divided into four seasons (3-month intervals). Injuries were classified into four categories (fractures, only laceration, hematoma, and abrasion), and facial fractures were classified according to the region of the injury (pan-facial, frontal, orbital, nasal, zygoma, maxilla, or mandible).
t-test were performed comparing mean of cost according to variable factor. Chi-square test was performed comparing type of admission or fracture by characteristics. Multiple linear regression analysis was performed to determine the effects of various factors on cost. A stepwise method was selected for the analysis. All statistical analyses were performed using IBM SPSS version 23 (IBM Corp., Armonk, NY, USA) software. Statistical significance was set at p<0.05.
RESULTS
The demographics of 93 patients, including 76 patients admitted to the ED and 17 outpatients, treated from January 2017 to December 2021 are shown in
Table 1. The average age of patients was 29.7±10.3 years (range, 13–56 years), and patients aged 20–29 years (n=39, 40.9%) were significantly predominant. Of the 93 patients, 75 patients (80.6%) were male and 18 patients (19.4%) were female, highlighting a male predominance. Twenty-five patients (26.9%) had consumed alcohol and 68 patients (73.1%) had not at the time of the accident. Ten patients (10.8%) wore helmets, but the majority (n=83, 89.2%) did not. Eighty-seven patients were injured due to a fall alone, while the remaining six were injured upon collision with an object. Of the collision cases, four patients collided with a 4-wheel vehicle, one collided with a stationary object, and one collided with another PMD. Fracture was the most common injury type (n=46), followed by only laceration (n=40). Zygoma bone fractures (n=17) were the most prevalent type of fracture, followed by nasal bone fractures (n=13). Severe cases such as pan-facial bone fracture (n=4) were included (
Fig. 2). Of the ED or outpatient outcomes, non-admission was more common (n=70, 75.3%), and 23 patients (24.7%) required admission for operation.
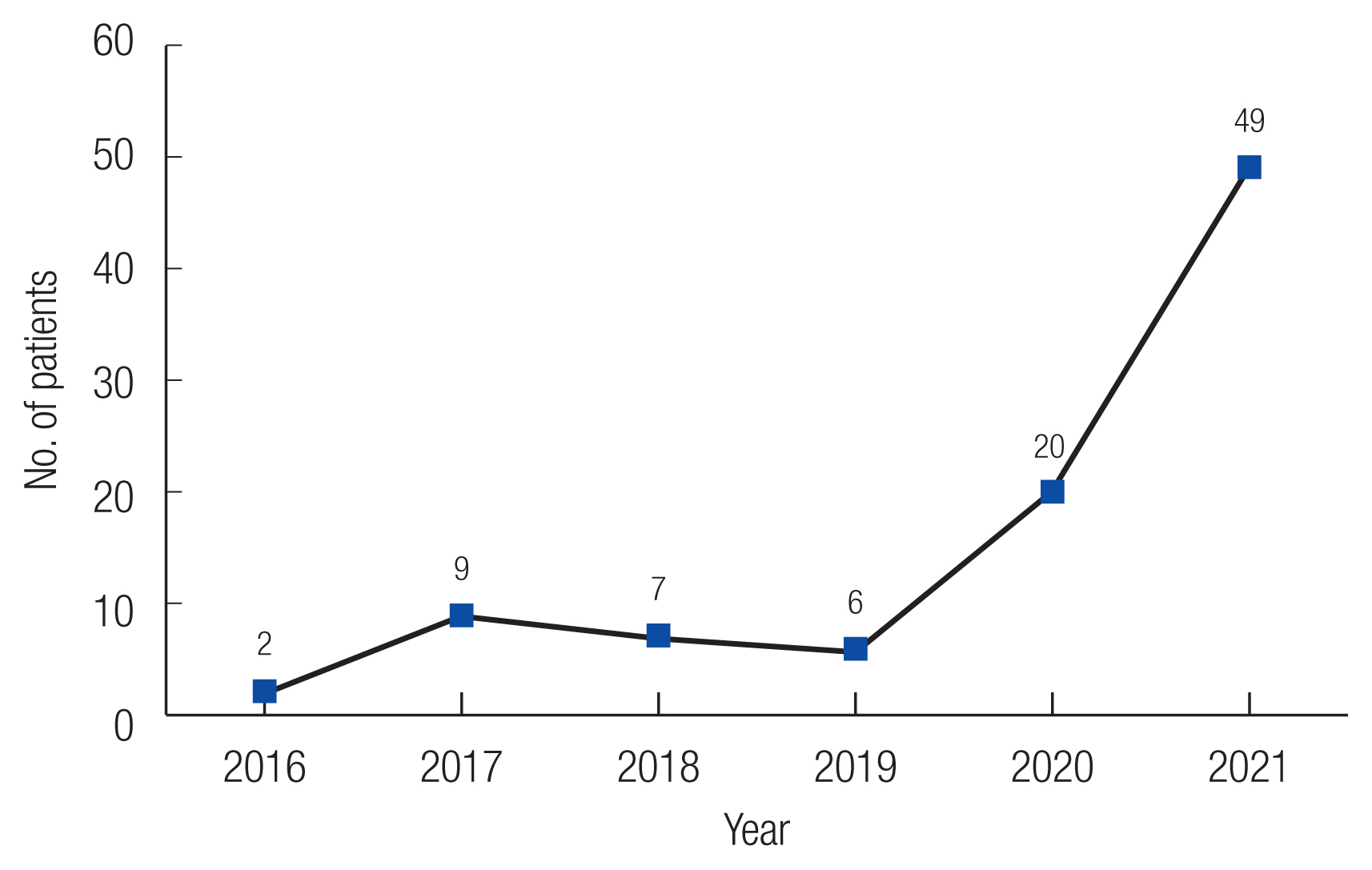
Until 2019, the annual number of PMD-related accidents was below 10; however, this number increased sharply in 2020 (
Fig. 3). For the time of day, the highest number of accidents occurred between 18:00 and 24:00 hour (n=49, 52.6%). There were more occurrences after sunset (18:00 to 06:00 hour: n=63, 67.7%) than during daylight hours (06:00 to 18:00 hour: n=30, 32.3%). The season with the highest number of cases was autumn (n=35, 37.6%), followed by summer (n=26, 28.0%), and the lowest number of accidents was in winter (n=14, 15.1%) (
Table 1).
Cost based on admission by type of injury was also investigated (
Table 2). The average cost of admission was USD 7,698, whereas the average cost of non-admission treatment was USD 631. The diagnosis with the highest social cost was pan-facial bone fracture (mean USD 17,092), and the mean length of hospital stay for these injuries was 25.8 days. The diagnosis with the second highest cost was zygoma bone fracture (mean USD 6,475), with a mean length of stay of 11.3 days. The most prevalent diagnosis among non-admission patients was laceration, with an average cost of USD 563. A linear regression analysis was performed to investigate the associations between various factors (age, sex, alcohol consumption, helmet use, type of impact, and type of injury) and total cost. Total cost was not significantly associated with age, sex, alcohol consumption, helmet use or type of impact; however, there were significant differences in fractures (β=0.405,
p<0.001) (
Table 3).
Fracture had a significant effect on total cost, and accordingly, patient features were compared between fracture and non-fracture groups (
Table 4). The male sex (82.6% vs. 78.7%) was predominant in both groups, and a significant difference was not found between the groups. In the fracture group, most common age at the time of injury was 30–39 years (34.8%), whereas in the non-fracture group, the most were aged 20–29 years (48.9%), however, the difference was not statistically significant. Most of the patients in both groups had not been drunk driving (71.7% and 74.5%) and had not worn a helmet (93.5% and 85.1%) with no significant difference. The type of impact had significant differences in both groups (
p=0.012), with falling off being the most common cause (87.0% vs. 100.0%). However, in the group without fractures, there was no case of collision. There was no difference by time or season, but admission and operation were significantly different in both groups (
p<0.001). There were more patients with fractures than without.
DISCUSSION
In accordance with the Korean Road Traffic Act [
10], a PMD is defined as a device that meets the following three conditions: (1) it is equipped with a motor that cuts out when the device reaches a speed at ≥25 km per hour, (2) weighs <30 kg, and (3) has a safety verification authorization according to Article 15-1 of the Electrical Appliances and Consumer Products Safety Control Act. Any vehicle that qualifies as being: (1) an electric kickboard, (2) an electric two-wheeled self-balancing vehicle, or (3) a bicycle that moves solely with power from an electric motor is called a PMD.
A literature review related to PMDs was performed (
Table 5). According to sex, 80.6% of injured patients in our study were males, which accords with findings in previous studies that males are predominantly injured [
9,
11–
15], apart from one study [
8]. In our study, the 20–29-year age group sustained the highest number of accidents (n=38, 40.9%), with patients aged 20–49 years accounting for 80.6% of all accidents. In other studies, the 20–39-year age group has been found to sustain the highest average number of injuries [
13]. One study reported an increased diagnostic rate along with older age, but the actual accident rate was not high [
16]. Currently in Korea, a PMD may be purchased or rented using an internet mobile phone application. Older adults may be less familiar with PMD rentals using the internet or a mobile phone or may have poor accessibility, which may explain why more young people have been using PMDs to date.
Alcohol consumption is considered a significant factor in facial trauma, and two studies found that alcohol consumption increased the incidence and severity of facial trauma [
17,
18]. Drink-driving is punishable by law, but no specific measures or regulations have been implemented to date concerning the use of PMDs. In this study, 26.9% of patients who had PMD-related accidents had consumed alcohol, which was higher than the 4.8%–11.2% reported in other studies [
9,
14]. Because blood alcohol levels were not measured, it was difficult to determine the amount of alcohol consumed. In this study, 10.8% of the patients had been wearing a helmet, with other studies reporting helmet use to have ranged from 2.8% to 18.6% [
9,
11,
13–
16]. One study reported that the risk of head and neck injury increased due to failure to wear a helmet [
12]. In this study, our regression analysis showed no significant association with cost. We excluded patients with head injuries who had been admitted to other departments, which may have affected our study findings concerning cost. However, a helmet is designed to protect the head to prevent a serious brain injury, and thus, may not have had any relation to facial injuries sustained.
Studies on accident frequency according to the hour, month, and year have also been conducted. One study reported that 56.6% of accidents occurred during the late afternoon and evening hours, between 15:00 and 23:00 hour [
9]. Another study explored two time periods (between 07:00 and 18:00 hour and between 18:00 and 07:00 hour) to take into account the field of view after sunset, and the results showed that 48.6% and 51.4% of accidents occurred during these time periods, respectively [
8]. In this study, 52.6% of all accidents occurred in the hour between 18:00 and 24:00 hour. Although different studies have used different time ranges, the frequency of accidents appears to be high during the hours after sunset. Therefore, PMD operators need to be especially careful during these hours. In terms of accidents by months, a study conducted in Singapore reported that 78.1% of accidents occurred from June to September [
12]. In this study, most accidents were in autumn (37.6%), followed by summer (28.0%). Accidents occurred at a relatively lower rate in winter (15.1%), when there were relatively fewer outdoor activities due to the weather being too cold. Since 2020, it has provided services that can be easily rented around university and subway stations. This seems to have contributed to the rapid increase in accidents since 2020 that anyone can easily access PMD.
Concerning the type of accident, all previous studies reported that falling was the most common [
9,
11,
12,
15,
16], which also accounted for 93.5% of injuries in this study. According to the current Road Traffic Act, anyone over the age of 16 years who has a current motor vehicle license can operate a PMD. Because PMDs are a recent form of transport, many accidents are likely to occur due to inexperience in operating a PMD, even if the operator has a motor vehicle license. In the near future, an independent license to operate a PMD is expected to be required. PMDs may not be operated on sidewalks, and no passengers are permitted. However, given current infrastructure and in attempts to avoid motor vehicles on the roads, PMD users do appear to utilize pedestrian sidewalks and common passageways between buildings. Consequently, there has been an associated increase in the number of collisions between pedestrians and PMD users. Wearing a helmet is a mandatory requirement and drink-driving is punishable by law. However, there appears to be low adherence to these requirements, resulting in an increasing number of accidents. Therefore, it appears there needs some legal amendment regarding PMD operation and safety maintenance. Concerning injury sites, head injury is reported to be the most common. One study reported that head (38%) and facial (33%) injuries were predominant in children while adults had more extremity fractures (73%) [
11]. In addition, another study reported that external wounds occurred in 89.2% of patients [
12]. These injury sites are closely associated with plastic surgery; thus, the role of plastic surgery in PMD-related accidents is likely to become more significant.
The increase in the number of PMD-related accidents has led to an increased burden for both patients and society. The median hospital charge has been reported to be USD 1,333 (range, USD 723–5,155) for ED and USD 25,733 (range, USD 4,366–69,139) for admission [
8]. Another study reported the median cost of admission to be USD 5,620 [
15]. In our study, the average cost was USD 7,698 for admission and USD 631 for non-admission. The cost of admission per patient is lower than that of patients with injuries sustained from accidents involving other modes of transport. For motorcycle accidents, the mean total cost of admission has been reported to be USD 209,515 in Brazil [
19]. Another study reported that the average hospital charges would be USD 95,376 for a nonhelmeted motorcycle patient and USD 71,774 for a helmeted motorcycle patient [
20]. For bicycle accidents, the mean cost per case including medical costs, work loss, and quality-of-life loss were USD 437,872 for admission and USD 33,842 for ED [
21]. However, due to the extent of variation reported in the literature, accurate comparison is difficult. We reported purely the cost of admission, and we did not include costs incurred by follow-up visits or by productivity and economic losses. When the healthcare and societal costs are factored into the analysis, the actual total cost is expected to be higher than the values presented. In addition, since there was no study limited to facial injury, it is expected that the cost of our patients differs from that of patients in other studies.
The limitations of this study include a single-center study design and the inherent bias associated with retrospective studies. Therefore, the PMD-related injuries and hospital costs were identified based on the patient’s medical chart, which might have led to an underestimation. In addition, information about known risk factors that may affect the injury severity, such as weather, place of the accident, speed at the time of the accident, and status of license acquisition could not be obtained. Lastly, no comparison was made with similar modes of transportation.
The prevalence of PMD use and related injuries requiring plastic surgery during the study period showed significant health and financial costs to both the patients involved and society. This cost could be reduced through stricter regulations concerning PMD use, advocating the use of protective gear, and promoting greater awareness of safety measures and of the consequences of PMD-related accidents.