INTRODUCTION
The face is one of the most essential parts of the body. Scars or skeletal deformation on the face can have significant serious functional and psychological consequences for patients [
1]. If facial fractures are not properly treated, they can lead to post-traumatic facial deformity; the greater the separation and dislocation of the fracture, the worse the facial deformity. Post-traumatic facial deformity is an acquired deformity caused by trauma. Therefore, when treating facial features, it is essential to consider the diagnosis of fracture as well as the presence and degree of dislocation of the broken bone fragments.
Nasoethmoid orbital fracture is a complicated midface structure facture that can include the nasal, lacrimal, maxillary, frontal, and ethmoid bones and may be caused by high-velocity blunt trauma. Reconstructing the orbital wall using conventional plates and screws is extremely difficult and can often result in complications, such as facial deformation, nose and forehead depression, and telecanthus [
2]. Reoperation is inevitable in such cases. Therefore, it is necessary to reduce cosmetic and functional complications to improve medical care and quality of life. Plates and screws are currently widely used in facial reconstruction and are manufactured in uniform shape and size. Plates are bent appropriately during surgery to fit the contour; however, the deformation limit of these readymade products poses several disadvantages.
A three-dimensional (3D) printer produces a 3D object in the desired shape using a computer-aided design and by converting it into 3D design data and stacking materials. Studies on 3D printing-based patient-customized craniomaxillofacial reconstruction are currently underway [
3]. Several studies have found that the functional and aesthetic prognosis of patients is better than surgery using conventional plates and screws for treating fractures [
3,
4].
However, only a few studies have been conducted on nasoethmoid orbital fractures. Therefore, it is necessary to develop a patient-customized nasoethmoid orbital fracture prosthesis based on 3D printing.
IDEA
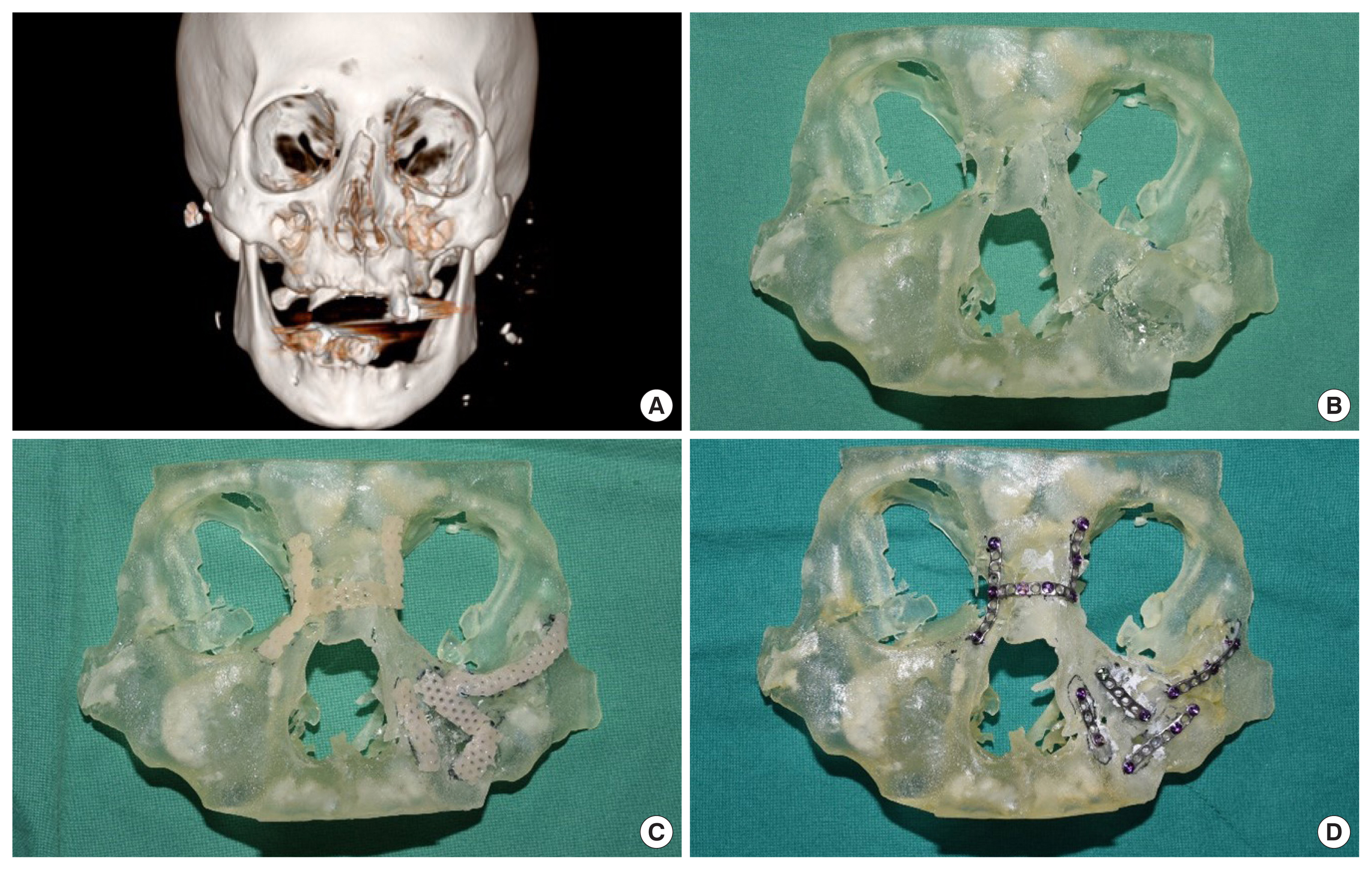
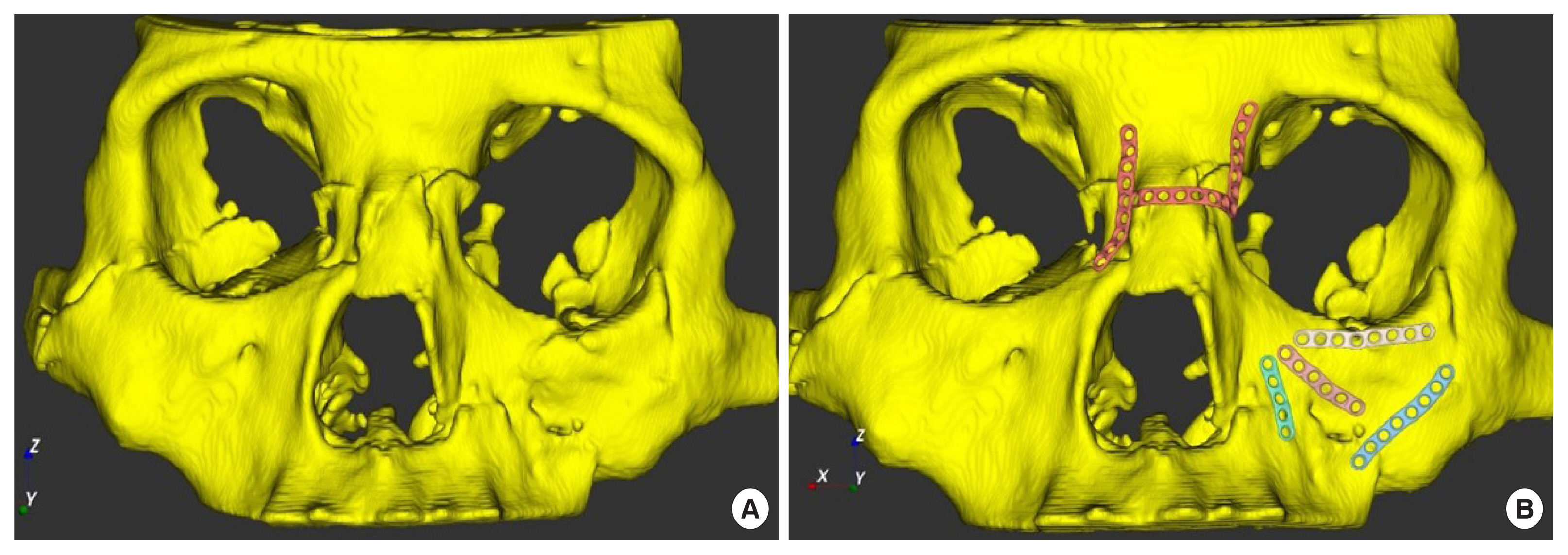
In this study, 10 patients underwent simulated surgery for nasoethmoid orbital fracture. Patient history was taken, and two-dimensional/3D imaging were taken to evaluate the patients’ facial fractures.
Based on 3D facial computed tomography (CT) results of all patients, facial bones were 3D printed using a Stratasys J826 3D printer (Stratasys, Eden Prairie, MN, USA) and Agilus30 clear (Stratasys) as the printing material. During the simulated surgery, the osteotomy site was appropriately designed, and osteotomy was done using a surgical saw. Further, a reduction surgery was performed on the displaced bone. For fixation, an Aquaplast (WFR/Aquaplast Corp., Wyckoff, NJ, USA) was used, which is suitable as a temporary model for the plates because it can deform easily with heating and hardens rapidly after cooling. The optimal position for fixing the patient-customized plate was determined using the Aquaplast. The patient-customized plate was manufactured based on the Aquaplast for simulation in five patients using a ProX DMP 320 3D printer (3D Systems, Rock Hill, SC, USA). The screws were printed using a ProX DMP 320 3D printer, using LaserForm Ti Gr2 (3D Systems) made of titanium as the printing material. Simulated surgery using the 3D-printed plate was performed on five patients (
Figs. 1,
2), whereas simulated surgery using a readymade plate was performed on the other five patients. The average duration of the surgery using the 3D printing customized plate and the readymade plate was 27.5 minutes and 41.2 minutes, respectively.
DISCUSSION
Nasoethmoid orbital fractures are complex fractures that may involve the nasal, lacrimal, maxillary, frontal, and ethmoidal bones. Compared with other facial fractures, nasoethmoid orbital fractures are rare; however, diagnosing and treating these fractures is extremely challenging. Moreover, they can have severe adverse effects if treatment is delayed or incorrect [
3]. The nasoethmoid orbital region is anatomically complex because it is directly connected to the anterior cranial base, leading to frequent outflow of cerebrospinal fluid after trauma and various neurosurgical problems, such as olfactory disorders. Furthermore, such fractures are difficult to treat because of a variety of complex problems, such as medial orbital wall fracture and probable damage to the medial canthal tendon, nasal bone, and lacrimal system.
Over a period of 3 years, Ellis [
5] reported 26 cases of nasoethmoid orbital fractures. In their study, 11 patients were unilateral, and 17 had different facial bone fractures. Further, 11 of these patients presented with cerebrospinal fluid outflow, which stopped 10 days after reduction, without occurrence of meningitis. In another study, Cruse et al. [
6] reported 18% of nasoethmoid orbital fractures in 182 cases of facial bone fractures, with an average age of 31 years. Further, 51% of these cases were associated with neurological damage, and 42% of the cases had cerebrospinal fluid outflow. These complications can have serious adverse effects, and secondary treatment may be difficult or impossible if they occur. Therefore, only accurate diagnosis and treatment can reduce complications in cases of nasoethmoid orbital fractures.
The first 3D printer was developed in 1984, and the first patent for a metal 3D printer was filed in 1986 [
7]. The most common manufacturing methods are mechanical processing and laser cutting or polishing of large stereoscopic materials. Alternatively, 3D printing can be performed by stacking layers of solid, liquid, or powdered materials based on design data. Machine processing is a cutting process that discards a large number of raw materials [
7]. In contrast, 3D printing reduces the use of raw materials by spraying and using only the necessary raw materials [
7]. As a result, 3D printing is widely used in the medical field for cases requiring personalized medical care and medical cost reduction [
4]. Currently, a typical application of 3D printer for customized care is for the creation of customized prostheses (e.g., hearing aids, dental materials, and prosthetic limbs) [
8]. The development of 3D printers had markedly reduced the manpower and time required for producing customized hearing aids; however, the current hearing aid production methods require manual ear modeling owing to the individuals’ differences in ear shapes. Furthermore, dental prosthetics can be effectively manufactured using a 3D printer, conferring the advantage of rapidly constructing certain high-quality dental prosthetics. Fracture surgery or anatomically complex surgery can be performed using a 3D printer by constructing customized prostheses prior to surgery, followed by simulation to reduce surgical time and minimize postsurgical complications. Currently, 3D printers are used in numerous clinical applications in the field of facial plastic surgery and reconstruction, including orthogonal surgery, post-traumatic surgery, tumor surgery, cranioplasty, and implantation [
9]. In a recent study, the mandible was 3D modeled using a 3D printer before partial resection, and the prosthesis for reconstruction after the incision was designed in advance [
10]. By creating templates in advance for maxillary surgery using 3D printers based on reported preoperative simulations, LeFort fracture surgery or fracture potentials resulted in better postoperative results [
11]. However, few studies have been conducted on reconstruction using a customized prosthesis for nasoethmoid orbital fractures. This study can be used as the basis for the manufacture of a customized prosthesis via 3D printing and to achieve better aesthetic and functional prognosis than conventional surgical methods.
Although we conducted simulated surgery, surgery using a 3D printer was completed in less time than that using conventional plates for treating nasoethmoid orbital fractures. Furthermore, based on the preoperative 3D CT results of the patient, it was possible to predict the reduction and location of fixation using plates. This suggested that the aesthetic and functional prognosis could be further improved in the patients during the treatment.