|
 |
- Search
| Arch Craniofac Surg > Volume 23(6); 2022 > Article |
|
Abstract
Naso-orbito-ethmoidal (NOE) fractures are complicated fractures of the mid-face. The treatment of NOE fractures is challenging and a comprehensive treatment strategy is required. We introduce a case of NOE fracture treated with open reduction and suspension sutures. A 28-year-old woman presented with a unilateral NOE fracture. To reduce the frontal process of the maxilla, a suspension suture was made by pulling the fragment using a double arm suture via a transcaruncular incision. The suture thread was placed in the horizontal plane. Another suspension suture on the inferior orbital rim assisted reduction procedure, and they passed through the overlying skin. The reduction alignment could be finely adjusted by tightening the transcutaneous suture threads while checking the degree of bone alignment through the subciliary incision. The two suture threads were suspended using a thermoplastic nasal splint. An additional skin incision on the medial canthal area, which would have resulted in a scar, could be avoided. Four months postoperatively, computed tomography showed an accurate and stable reduction. The patient was satisfied with her aesthetic appearance, and functional deficits were not present.
Naso-orbito-ethmoidal (NOE) fractures are complicated fractures of the mid-face that usually result from severe blunt trauma, such as motor vehicle accidents and assaults [1]. NOE fractures account for 15% of pediatric facial fractures and fewer than 5% of adult facial fractures [2]. The central feature of NOE fractures is a displacement of the medial orbital rim with the medial canthal tendon (MCT) attached [3]. Although the severity of their sequelae varies according to the extent of the fracture and injuries of the surrounding structures, NOE fractures can cause severe disfigurement (e.g., flattening of the mid-face, telecanthus, and dystopia) and functional loss (e.g., diplopia and loss of nasal support) [1,4].
NOE fractures are quite challenging to treat, and therefore require a comprehensive treatment strategy. Through accurate and elaborate reduction, good aesthetic and functional outcomes can be obtained. Various approaches have been described to achieve this goal [3]. The suspension technique was introduced as a useful option for maintaining unstable nasal bones [5]. With regard to the previous report, we utilized suture threads for fracture site reduction as well as maintenance of alignment. The authors present a patient with a unilateral NOE fracture who was treated with open reduction and suspension sutures.
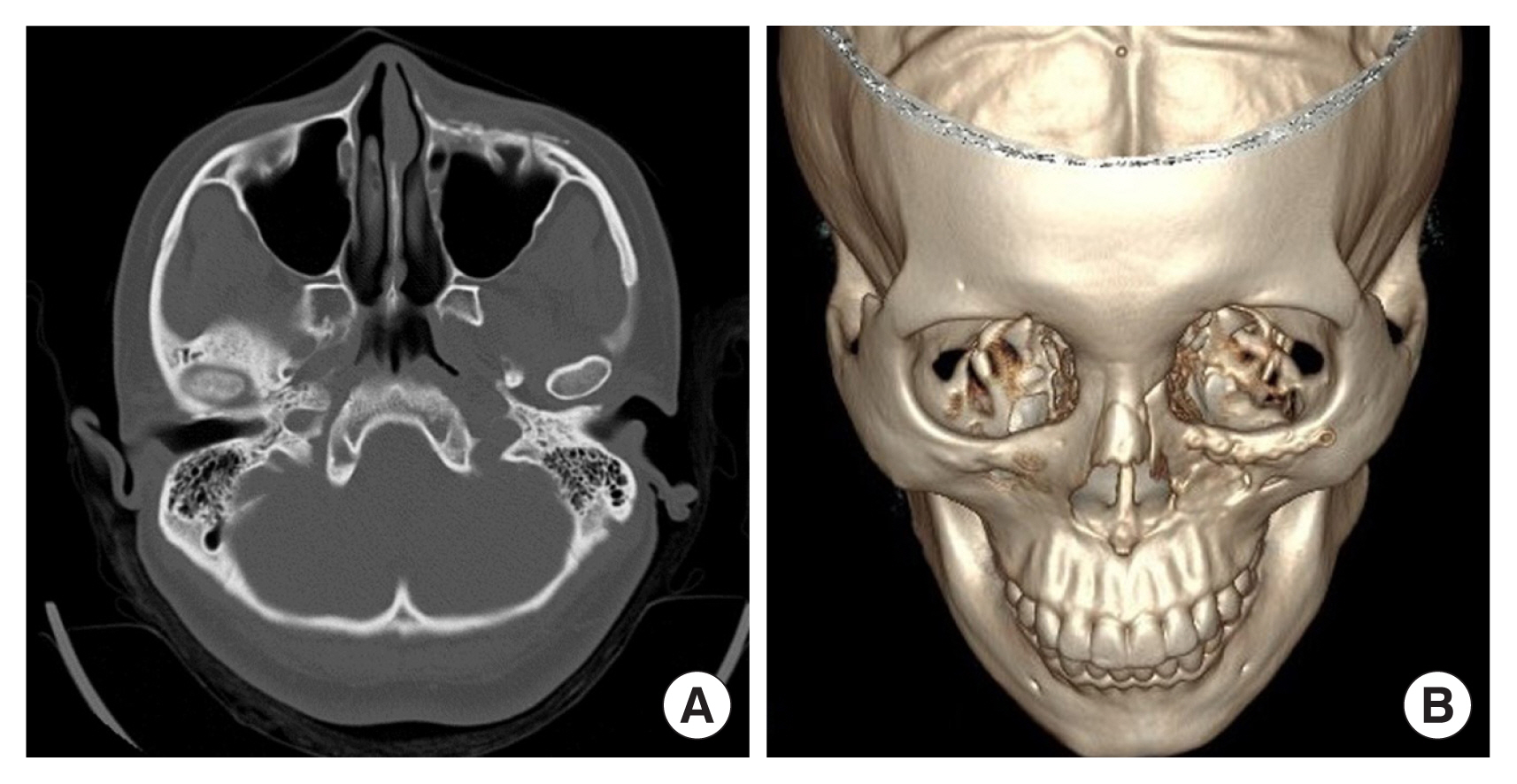
A 28-year-old woman presented to the emergency department with facial trauma. She had fallen from an electric scooter and complained of blurred vision in the left eye without diplopia. Left facial paresthesia was noted, and partial injury of the infraorbital nerve could be assumed considering a comminuted fracture around the infraorbital foramen. The patient had no previous history of trauma to the left periorbital area and had no underlying diseases. Computed tomography (CT) images demonstrated displacement of the left NOE complex (Fig. 1). In addition, a nasomaxillary buttress fracture was observed, nonetheless zygomaticomaxillary buttress was maintained. Ophthalmologists diagnosed preretinal and vitreous hemorrhage. The distance from the lateral orbital rim to the corneal apex in both eyes was the same as 17 mm. The distance from the facial midline to bilateral pupils was the same on both sides, and the interpupillary distance was 6.5 cm.
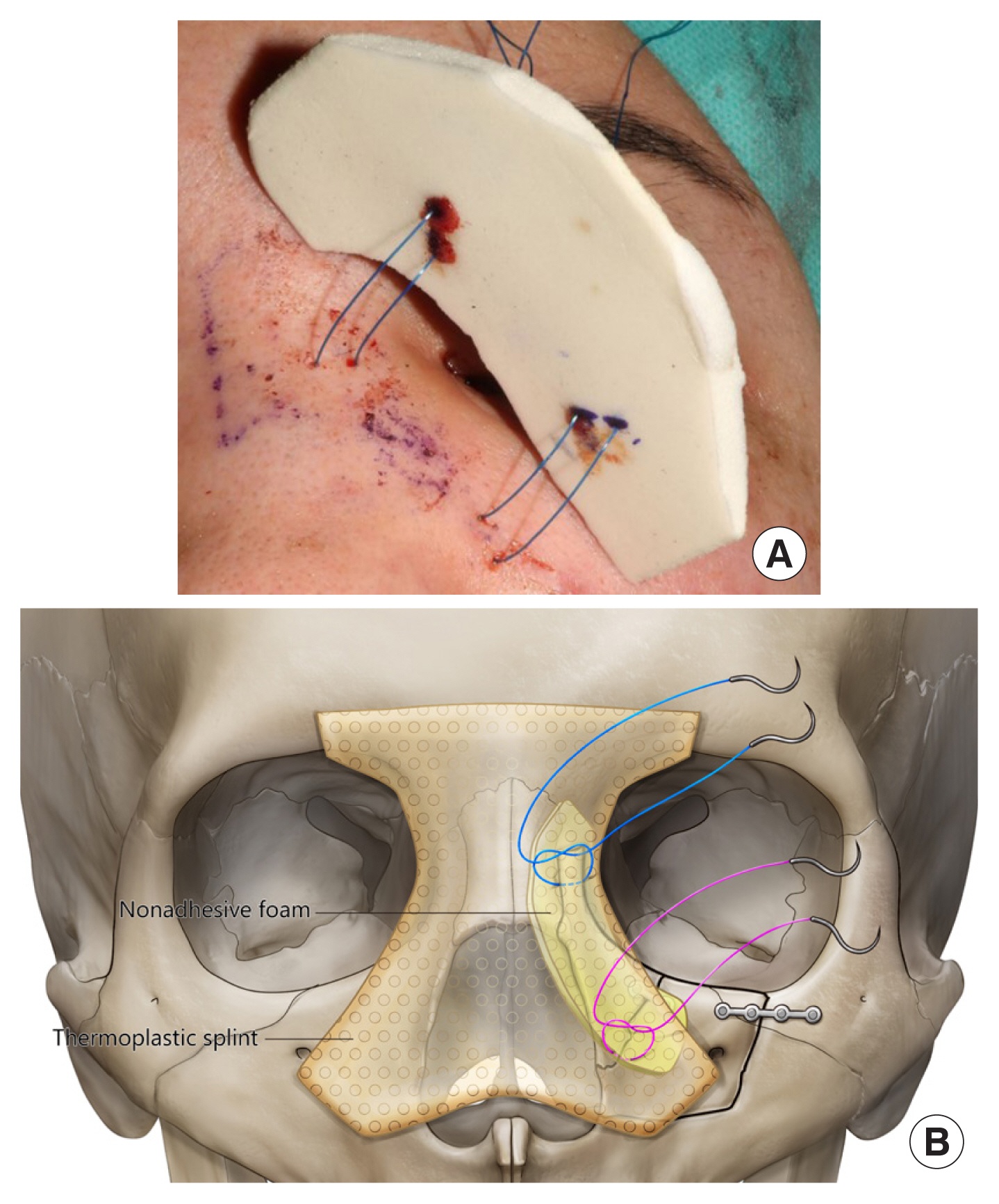
The patient was concerned about the possibility of a large visible scar on the mid-face after surgery, and there was no injury on the MCT. In this context, an open reduction surgery via subciliary and transcaruncular incisions was planned under general anesthesia. A gingivobuccal incision was also made to check the nasomaxillary buttress fracture. The inferior wall of the orbit was exposed through a subciliary incision and the medial wall of the orbit was exposed through a transcaruncular incision. To reduce the upper portion of the frontal process of the maxilla, the first suspension suture was made by pulling the fragment using a double arm suture via the transcaruncular incision (Fig. 2). The suture thread was inserted from the lateral to medial direction. To reduce the fragment in the infraorbital area, the second suspension suture passed through the lower portion of the frontal process of the maxilla and displaced infraorbital fragment via the subciliary approach (Fig. 3).
The reduction alignment could be finely adjusted by tightening or loosening the transcutaneous suture threads while checking the degree of bone alignment through the subciliary incision. The suture threads were suspended using a thermoplastic nasal splint for 2 days (Fig. 4). The infraorbital fragment was reduced using a K-wire and fixed with absorbable plates and screws. The K-wire was removed intraoperatively. The screw-wire traction technique can be utilized alternatively, which is safe and efficient for precise alignment. Finally, closed reduction was performed for the nasal bone fracture using a freer elevator. Both suture treads and nasal splint were removed 2 days after the operation. The patient was discharged 5 days after the operation without any complications.
A CT image taken 4 months after the operation showed an accurate and stable reduction, with the displaced segments and the frontal process of the maxilla in their anatomical positions (Fig. 5). Although slight depression was presented compared to the contralateral side on the CT image, it was not problematic. The overlying skin and soft tissue could compensate for the postoperative change. The patient was satisfied with her aesthetic appearance since an additional external surgical scar was not created in the medial canthal area.
NOE fractures are caused by high-energy impacts and, as a result, are often accompanied by other facial fractures and injuries to the surrounding structures, such as the nasofrontal duct and ocular region [6]. Common complications of NOE fractures include exophthalmos, telecanthus, and leakage of cerebrospinal fluid through the cribriform plate [7]. Although several classifications have been suggested in previous studies, one of the most commonly used classifications is that presented by Markowitz et al. in 1991 [8]. This system, which grades the extent of damage based on the status of the MCT and the central bone fragment, is used to assess the severity of the injury preoperatively and to plan treatment. In class I fractures, the MCT is attached to a relatively large central bone fragment; in class II fractures, the MCT is still attached to more comminuted fragments; and in class III fractures, the MCT has been detached from the place of bony insertion.
In a physical examination, the stability of the central bone fragment, and detachment of the MCT are important for determining the treatment plan. Whether the MCT is detached can be confirmed by palpating it directly and the âbowstring testâ [9]. This test is positive if there is a mobile fracture segment or lack of resistance when the MCT portion is palpated while pulling the medial portion of the lower eyelid laterally [10]. Epiphora may occur as a result of associated injury to the lacrimal duct. In addition to the primary injury of the lacrimal duct, epiphora can result from swelling of soft tissue or obstruction caused by bony fragments [9].
Severe NOE fractures may present with loss of nasal support due to injury of the nasal bone and cartilage, which may require a bone graft on the nasal dorsum and the tip of the nose in rare cases [4]. Since physical examination often does not yield a precise clinical evaluation due to swelling, CT is a good radiographic tool to obtain a more accurate diagnosis. Although CT cannot show the MCT directly, the gap in the anterior aspect of the medial orbital wall and the presence of a comminution fracture of the medial orbital wall, where the MCT inserts, helps to define the extent of fracture and avulsion of the MCT [11].
An essential goal of NOE fracture treatment is to restore the previous facial appearance. There is no universally accepted surgical technique due to variations in the types of NOE fractures and the degree of injury to the surrounding structures. Several methods of exposing the fracture site have been studied. The coronal approach is the standard method for complicated NOE fractures because it can expose the fracture site sufficiently for the fracture to be evaluated and visualized, as well as enable manipulations such as internal fixation of the nasal dorsum. However, it results in a long scar on the scalp and has complications such as numbness of the scalp and alopecia, so it is not suitable for simple NOE fractures and requires an additional incision if the fracture site is located in the lower part of the mid-face [4]. To avoid these shortcomings, Cultrara et al. [12] described mid-facial degloving as a method of exposing the entire medial facial skeleton through bilateral labial incisions in the maxilla. However, this technique also has complications such as temporary infraorbital numbness, nasal obstruction, and nasal deformity. The open-sky and medial brow incisions are suitable approach methods, however the patient was concerned about postoperative scars [13,14]. In this context, we decided on subciliary and transcaruncular incisions.
In recent years, minimally invasive surgical techniques, such as endoscopy, have provided the advantage of reducing patient morbidity and operation time enabling faster recovery, while producing similar outcomes compared with previous approaches [15,16]. Additionally, since visible surgical scars on the mid-face are undesirable, a minimally invasive approach is important for treating NOE fractures. The patient described herein, a young woman, was concerned about a large visible scar after surgery. The intact surrounding structures including frontal bone, zygomatic body, and contralateral orbital rim enabled proper reduction to be maintained using suspension sutures made via subciliary and transcaruncular incisions. Although reduction using a suspension suture through a transcaruncular incision has the disadvantage of not allowing confirmation of the reduction due to insufficient exposure of the fracture, it was possible to confirm the reduction state through a subciliary incision. Our method can be applied in NOE fractures that do not present telecanthus, severely comminuted fragments, and accompanying frontal sinus fractures.
Postoperative scars may lead to discoloration, skin dimpling, or disfiguration [17]. Additional procedures can be necessary to relieve the scar. In this context, strategic operative planning is essential to minimize a postoperative scar in facial plastic surgery [18]. Minimally invasive open reduction supplemented with suture suspension can be an adequate alternative to treat NOE fractures [19]. The technique was efficacious in both fracture reduction and maintenance of alignment.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Konkuk University Hospital (IRB No. KUH 2020-10-019).
Patient consent
The patient provided written informed consent for the publication and use of her images.
Author contributions
Conceptualization: Myungchul Lee. Methodology: Youngsu Na, Yongseok Kwon, Myungchul Lee. Visualization: Youngsu Na, Yongseok Kwon, Jeenam Kim. Writing - original draft: Youngsu Na, Yongseok Kwon, Myungchul Lee. Writing - review & editing: Chaneol Seo, Jeenam Kim, Hyungon Choi, Donghyeok Shin. Investigation: Chaneol Seo. Resources: Chaneol Seo. âSupervision: Jeenam Kim, Hyungon Choi, Donghyeok Shin.
Fig. 1
Preoperative computed tomography (CT) images. (A) Preoperative CT image demonstrating displacement of the left naso-orbito-ethmoid complex, axial view. (B) Preoperative three-dimensional CT image, birdâs eye view.
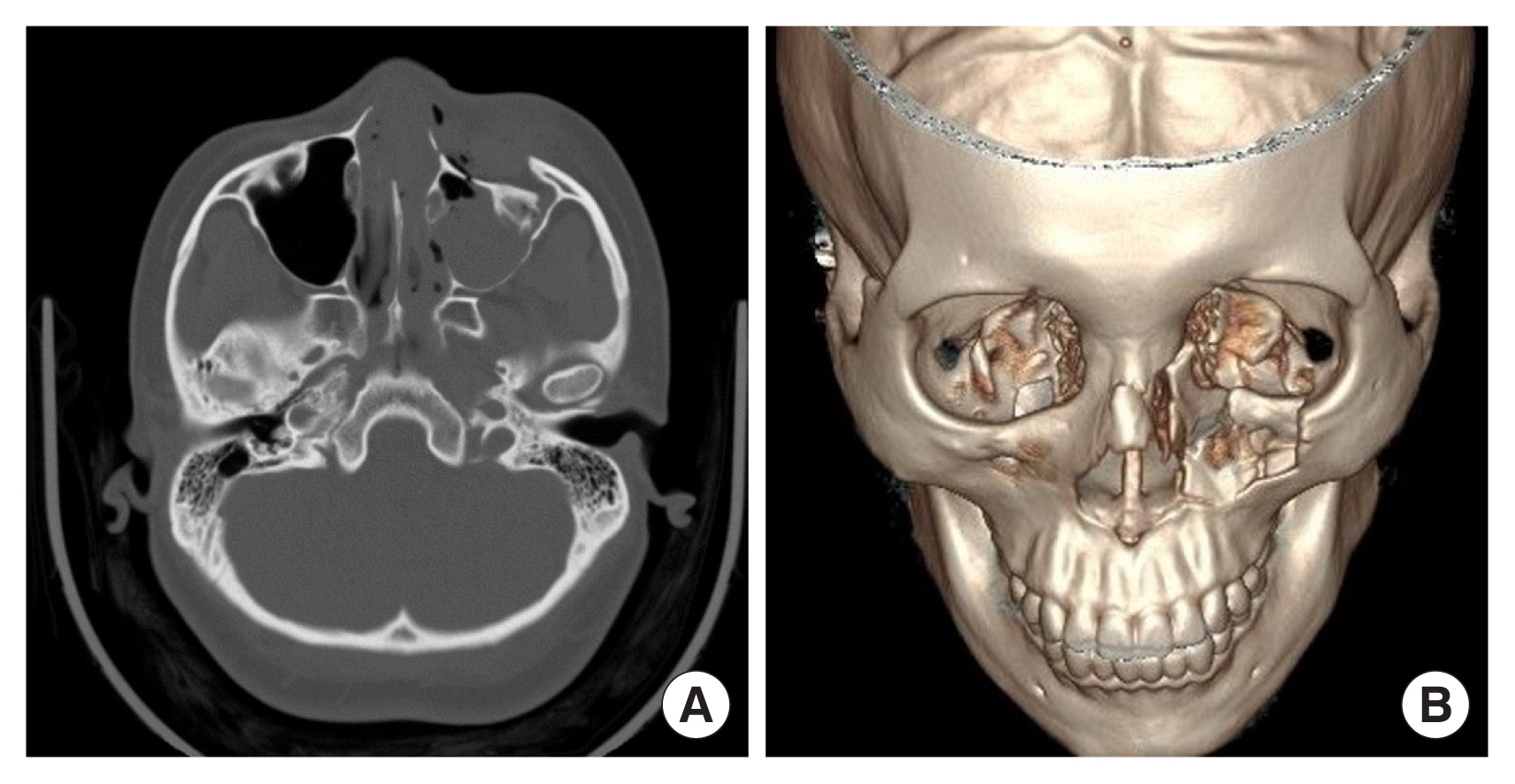
Fig. 2
Illustration of surgical technique. The first thread was inserted from the lateral to medial direction (double-armed Prolene #2-0 suture, blue line) to reduce the frontal process of the maxilla. The second thread passed through drilled holes (double-armed Prolene #2-0 suture, pink line) to reduce the displaced infraorbital fragment. A K-wire on one side of the fragment assisted fracture reduction.
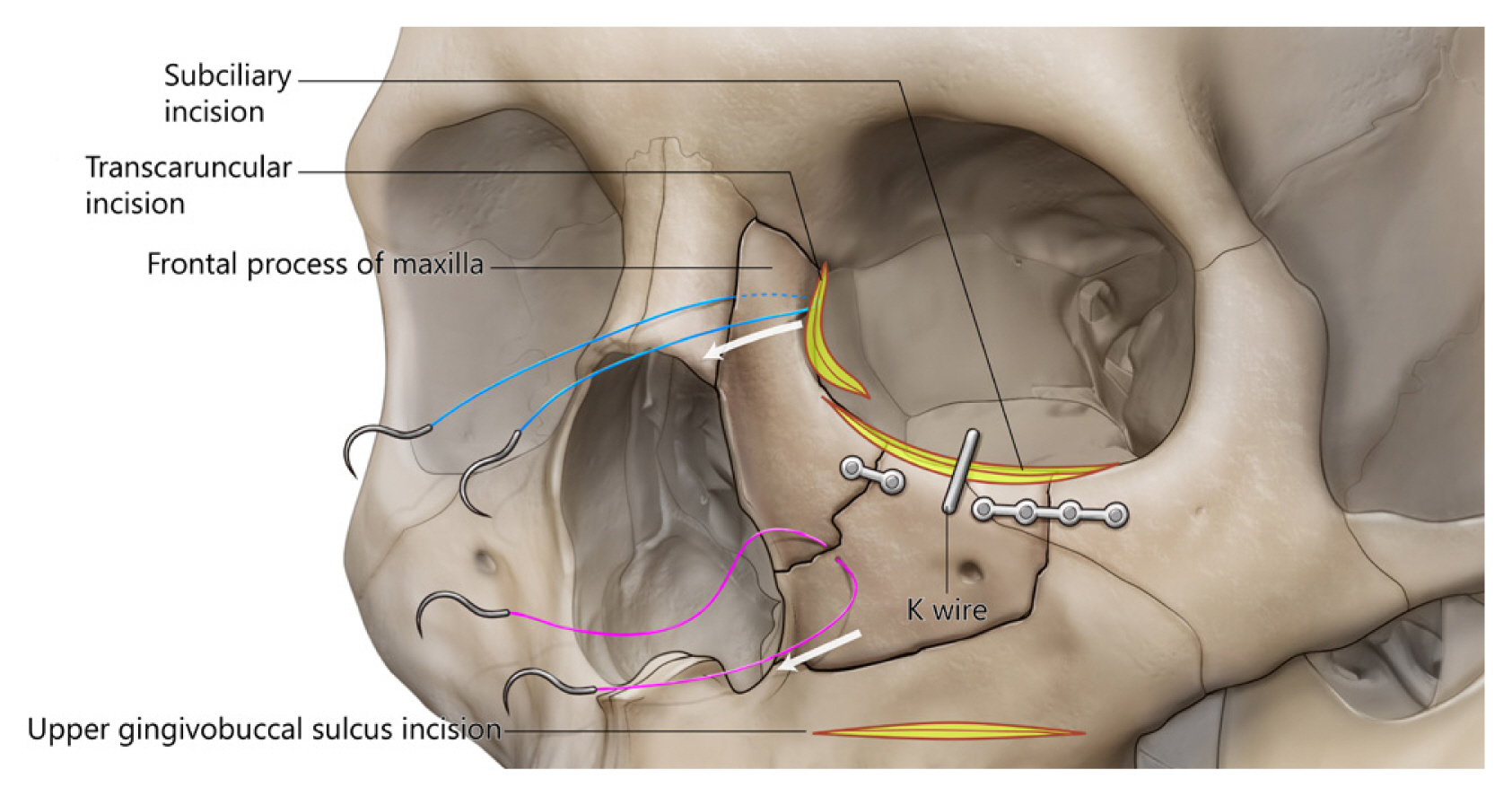
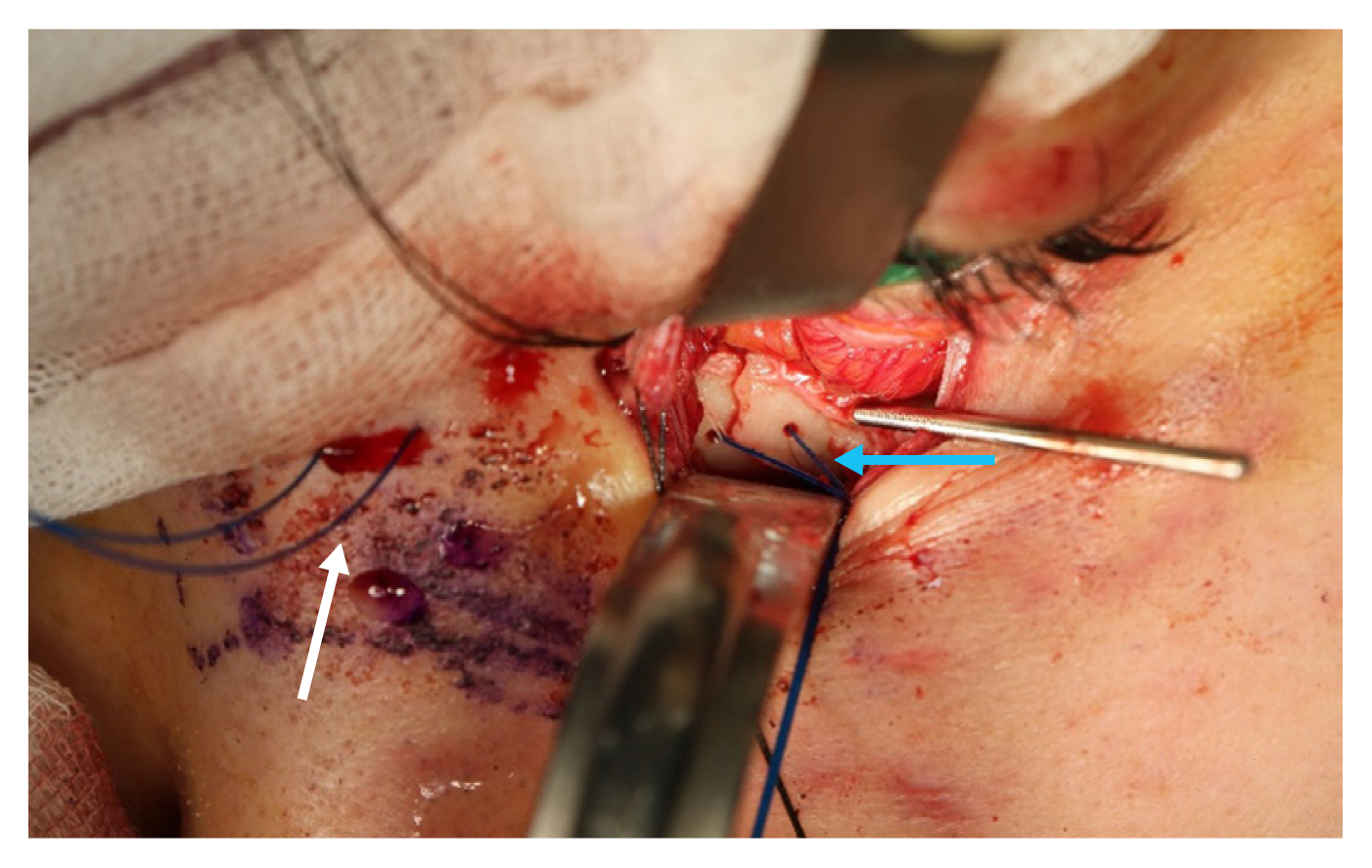
Fig. 3
Intraoperative photograph showing suspension sutures. The first thread (white arrow) comes out of the skin, and the second thread (blue arrow) passes through the bone via drilled holes. A K-wire on one side of the fragment assisted fracture reduction, and the reduction state could be confirmed through a subciliary incision.
REFERENCES
1. Buchanan EP, Hopper RA, Suver DW, Hayes AG, Gruss JS, Birgfeld CB. Zygomaticomaxillary complex fractures and their association with naso-orbito-ethmoid fractures: a 5-year review. Plast Reconstr Surg 2012;130:1296-304.

2. Kelley P, Crawford M, Higuera S, Hollier LH. Two hundred ninety-four consecutive facial fractures in an urban trauma center: lessons learned. Plast Reconstr Surg 2005;116:42e-49e.


3. Ha YI, Kim SH, Park ES, Kim YB. Approach for naso-orbito-ethmoidal fracture. Arch Craniofac Surg 2019;20:219-22.




4. Nguyen M, Koshy JC, Hollier LH Jr. Pearls of nasoorbitoethmoid trauma management. Semin Plast Surg 2010;24:383-8.



5. Hunter BG, Tasman AJ. Suspension technique for unstable nasal bones. JAMA Facial Plast Surg 2019;21:460.


6. Roden KS, Tong W, Surrusco M, Shockley WW, Van Aalst JA, Hultman CS. Changing characteristics of facial fractures treated at a regional, level 1 trauma center, from 2005 to 2010: an assessment of patient demographics, referral patterns, etiology of injury, anatomic location, and clinical outcomes. Ann Plast Surg 2012;68:461-6.

7. Garg RK, Alsheik NH, Afifi AM, Gentry LR. Pterygoid plate fractures: not limited to Le Fort fractures. J Craniofac Surg 2015;26:1823-5.

8. Fraioli RE, Branstetter BF 4th, Deleyiannis FW. Facial fractures: beyond Le Fort. Otolaryngol Clin North Am 2008;41:51-76.


9. Gruss JS, Hurwitz JJ, Nik NA, Kassel EE. The pattern and incidence of nasolacrimal injury in naso-orbital-ethmoid fractures: the role of delayed assessment and dacryocystorhinostomy. Br J Plast Surg 1985;38:116-21.


10. Rosenberger E, Kriet JD, Humphrey C. Management of nasoethmoid fractures. Curr Opin Otolaryngol Head Neck Surg 2013;21:410-6.


11. Doerr TD. Evidence-based facial fracture management. Facial Plast Surg Clin North Am 2015;23:335-45.


12. Cultrara A, Turk JB, Har-El G. Midfacial degloving approach for repair of naso-orbital-ethmoid and midfacial fractures. Arch Facial Plast Surg 2004;6:133-5.


13. Converse JM, Hogan VM. Open-sky approach for reduction of naso-orbital fractures: case report. Plast Reconstr Surg 1970;46:396-8.

14. Hwang K, Joong Kim D. Reduction of supraorbital fractures via a short sub-brow incision. J Craniofac Surg 2018;29:2164-5.


15. Jung JS, Kang DH, Lim NK, Kim H. Orbital wall restoration with primary bone fragments in complex orbital fractures: a preliminary study. Arch Craniofac Surg 2020;21:156-60.




16. Kim T, Kim BK. Endoscopic slide-in orbital wall reconstruction for isolated medial blowout fractures. Arch Craniofac Surg 2020;21:345-50.




17. Kim YJ, Kim JH, Kim YS, Cheon YW. Pin-site scar revision with subcisions and acellular dermal matrix. Arch Aesthetic Plast Surg 2020;26:38-40.


- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 2,249 View
- 98 Download
- Related articles in ACFS