|
 |
- Search
| Arch Craniofac Surg > Volume 15(1); 2014 > Article |
Abstract
Leiomyosarcoma is a rare form of soft tissue neoplasm, with only 1% to 5% occurring in the head and neck region. Current recommended treatment suggests surgical excision with a wide lateral margin, but no definite guidelines regarding excisional margin have been established yet. Recently, complete excision with a narrow surgical margin has been recommended, and the authors present a case of cutaneous leiomyosarcoma on the face that was successfully managed by complete removal with a narrow excisional margin. A 74-year-old woman presented with a 3 cm sized, rapidly growing cutaneous mass on her right preauricular area. Preoperative biopsy of the skin lesion suggested a cutaneous leiomyosarcoma. The authors performed complete surgical excision with a 1 cm lateral margin, and the resulting skin defect was repaired with bilateral V-Y advancement local flaps. Histopathology and immunohistochemistry evaluation confirmed a moderately differentiated cutaneous leiomyosarcoma, with negative margin involvement. The patient refused of any additional treatment, but showed no locoregional recurrence during the 1.5 years of postoperative follow-up period. With a regular postoperative follow-up, cutaneous leiomyosarcomas may be successfully treated with a narrow surgical margin.
Leiomyosarcoma is an uncommon malignant smooth muscle tumor. A superficial leiomyosarcoma is subdivided into cutaneous and subcutaneous tumor, depending on its primary site of origin. A primary cutaneous leiomyosarcoma derives from the erector muscles of the hair and sweat glands in the dermis and may present as a small, slow growing skin lesion [1], whereas a subcutaneous leiomyosarcoma arises from the muscular layers of blood vessels. Current recommended treatment includes local excision with a wide lateral margin of 2 to 5 cm, followed by adjuvant radiotherapy if deemed necessary [2]; however, definite guidelines for optimal safety margins are not yet been clearly defined. This article presents a case study of a rapidly growing cutaneous leiomyosarcoma occurring on the cheek of a patient that was successfully managed with a narrow excisional margin.
A 74-year-old woman presented with a painless, rapid growing, large mass on her right preauricular area (Fig. 1). The mass had developed 3 weeks prior to her visit, with no relevant past history. Physical examination showed a 3 cm-sized mass with bleeding tendency on her right cheek, and a computed tomography scan of the lesion strongly indicated a contrast-enhanced, hypervascular cutaneous tumor (Fig. 2). The authors performed a preoperative skin biopsy of the lesion, which suggested a cutaneous leiomyosarcoma. The patient underwent an en-bloc excision with a 1 cm margin under local anesthesia, and the resulting raw surface was covered with bilateral V-Y advancement skin flaps.
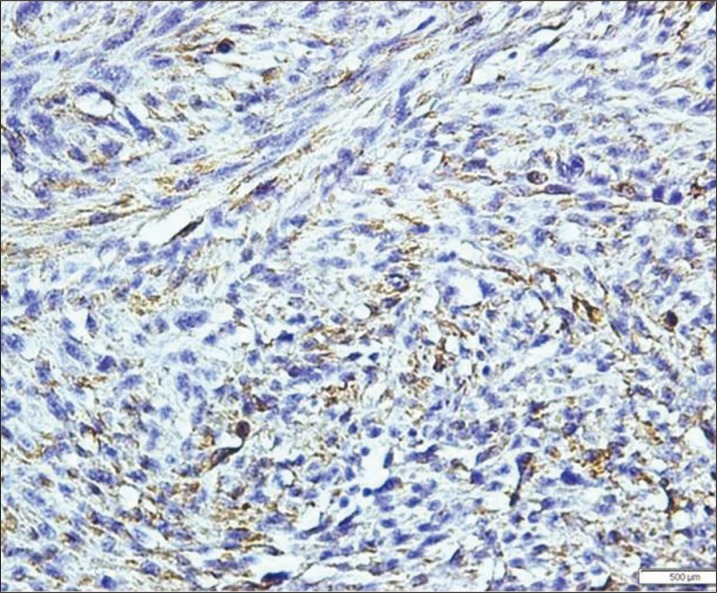
Histopathologic evaluation of the excised mass showed spindle cells with cigar-shaped nuclei, prominent cytologic atypia and high mitotic activity (Fig. 3). Subsequent immunohistochemistry revealed positive stains for muscle-specific actin and desmin (Fig. 4), with a lack of staining for S-100 protein. A moderately differentiated cutaneous leiomyosarcoma was diagnosed, with negative margin involvement. As the tumor had a relatively large size and exhibited high mitotic activity, the authors recommended adjuvant radiation therapy; however, the patient refused any additional treatment. The wound healed well postoperatively (Fig. 5), and no signs of local recurrence were observed during the 1.5 years of postoperative period.
Soft tissue sarcomas amount to approximately 1% of malignant tumors of the head and neck area, and leiomyosarcoma accounts for less than 3% of these [3]. Leiomyosarcoma may develop anywhere on the body, but has a predilection for the extremities. Only 1% to 5% of cases are being reported to occur in the head [4]; the rarity of this neoplasm in the head and neck area may be attributed to the scarcity of smooth muscle in this anatomic region. Leiomyosarcoma develops more common in males at a ratio of 2:1 to 3:1, between the 4th and 6th decades of life [5]. Its etiology is unknown, and previous reports have suggested trauma, radiation exposure, and preceding leiomyoma as possible risk factors [4].
Depending on its origin, superficial leiomyosarcoma is subdivided into cutaneous and subcutaneous types. The former tends to be a smaller, slow-growing lesion, while the latter takes a larger form characterized by rapid growth [1]. This categorization has clinical significance, as subcutaneous forms of this soft tissue neoplasm have a higher rate of local recurrence and distant metastasis. Besides its site of origin, Eppsteiner et al. [6] proposed high mitotic rate, lesions greater than 5 cm in size, and positive surgical margins as poor prognostic factors; other variables related to increased local recurrence rate include subcutaneous extension and advanced age [7].
Current proposed treatment of superficial leiomyosarcoma is local excision with wide margins, and adjuvant radiotherapy may be considered for patients who have the predisposing factors mentioned above. Existing literature suggests a 2 to 5 cm excisional margin for effective management; however, guidelines for optimal surgical margins are not yet clearly defined to date, and reports of successful management with a narrow margin have been published recently.
Tsutsumida et al. [4] performed complete excision of low-grade cutaneous leiomyosarcomas with a narrow margin, and reported no local recurrences or distant metastasis. Deneve et al. [8] surgically treated 33 patients with a 1 cm margin, and those with negative resection margin involvement showed no local recurrence during the average follow-up of 15.5 postoperative months.
In the present study, the authors performed complete surgical excision with a 1 cm lateral margin; the resulting small defect was adequately repaired with local skin flaps, precluding further morbidity in the region otherwise necessary in alternative methods such as skin grafting for larger defects.
It is well-known that the risk of malignant transformation increases with age, and any suspicious skin lesions in elderly patients mandate alert medical attention. Cutaneous leiomyosarcoma should be considered along with other possible skin tumors, such as pyogenic granuloma, basal cell carcinoma, squamous cell carcinoma, and keratoacanthoma. A suspected leiomyosarcoma, based on preoperative biopsy, necessitates surgical excision of the lesion, as well as subsequent medical follow-up for possible local recurrences, or in some cases, newly-developed skip lesions. Although previous literature recommends obtaining a wide excisional margin, the present authors propose that complete excision with a narrow margin may also be considered as an alternative method; coupled with a thorough and timely follow-up, this may produce satisfactory results by preventing unnecessary sacrifice of adjacent soft tissue, as well as by decreasing the locoregional recurrence rates.
References
1. Torres T, Oliveira A, Sanches M, Selores M. Superficial cutaneous leiomyosarcoma of the face: report of three cases. J Dermatol 2011;38:373-376. PMID: 21352334.


2. Porter CJ, Januszkiewicz JS. Cutaneous leiomyosarcoma. Plast Reconstr Surg 2002;109:964-967. PMID: 11884817.


3. Kransdorf MJ. Malignant soft-tissue tumors in a large referral population: distribution of diagnoses by age, sex, and location. AJR Am J Roentgenol 1995;164:129-134. PMID: 7998525.


4. Tsutsumida A, Yoshida T, Yamamoto Y, Itoh T, Minakawa H, Sugihara T. Management of superficial leiomyosarcoma: a retrospective study of 10 cases. Plast Reconstr Surg 2005;116:8-12. PMID: 15988239.


5. Fields JP, Helwig EB. Leiomyosarcoma of the skin and subcutaneous tissue. Cancer 1981;47:156-169. PMID: 7459804.


6. Eppsteiner RW, DeYoung BR, Milhem MM, Pagedar NA. Leiomyosarcoma of the head and neck: a population-based analysis. Arch Otolaryngol Head Neck Surg 2011;137:921-924. PMID: 21930982.



7. Suit HD, Spiro I. Role of radiation in the management of adult patients with sarcoma of soft tissue. Semin Surg Oncol 1994;10:347-356. PMID: 7997728.


8. Deneve JL, Messina JL, Bui MM, Marzban SS, Letson GD, Cheong D, Gonzalez RJ, Sondak VK, Zager JS. Cutaneous leiomyosarcoma: treatment and outcomes with a standardized margin of resection. Cancer Control 2013;20:307-312. PMID: 24077407.



Fig. 1
Preoperative appearance showing a 3 cm sized, hemorrhagic mass on the right preauricular area.

Fig. 2
Preoperative computed tomography scan showing a contrast-enhanced, hypervascular cutaneous mass confined to the dermal layer.
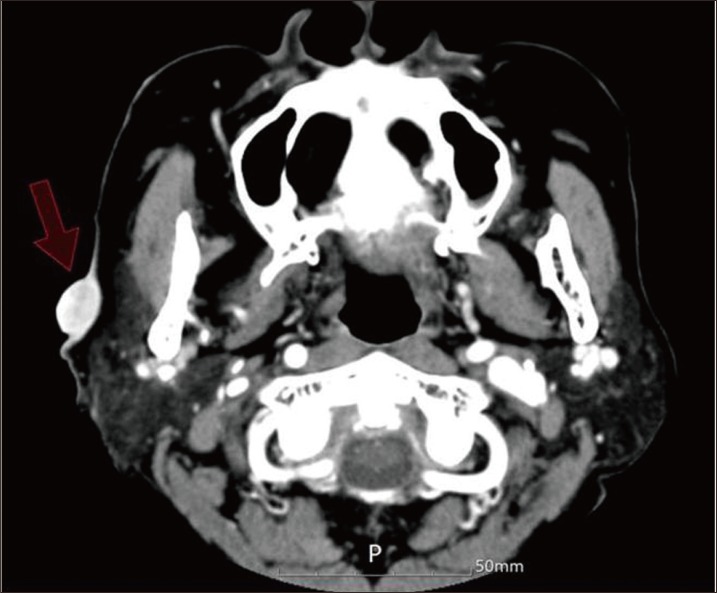
Fig. 3
Histopathology evaluation shows spindle cells with cigar-shaped nuclei, prominent cytologic atypia and mitotic figures (H&E, ×400).

- TOOLS
-
METRICS

-
- 3 Crossref
- Scopus
- 4,279 View
- 52 Download
- Related articles in ACFS
-
Soft-tissue osteoma of the temple2021 October;22(5)
Aggressive cutaneous squamous cell carcinoma of the scalp2020 December;21(6)
Meningothelial hamartoma of the scalp2020 June;21(3)