Comparison of Mechanical Stability between Fibular Free Flap Reconstruction versus Locking Mandibular Reconstruction Plate Fixation
Article information
Abstract
Background
The fibular free flap has been used as the standard methods of segmental mandibular reconstruction. The objective of mandibular reconstruction not only includes restored continuity of the mandible but also the recovery of optimal function. This paper emphasizes the advantage of the fibular free flap reconstruction over that of locking mandibular reconstruction plate fixation.
Methods
The hospital charts of all patients (n=20) who had a mandibular reconstruction between 1994 and 2013 were retrospectively reviewed. Eight patients had plate-only fixation of the mandible, and the remaining 12 had vascularized fibular free flap reconstruction. Complications and outcomes were reviewed and compared between the 2 groups via statistical analysis.
Results
Overall complication rates were significantly lower in the fibular flap group (8.3%) than in the plate fixation group (87.5%; p =0.001). Most (7/8) patients in the plate fixation group had experienced plate-related late complications, including plate fracture or exposure. In the fibular flap group, no complications were observed, except for a single case of donor-site wound dehiscence (1/12).
Conclusion
The fibular free flap provides a more stable support and additional soft tissue support for the plate, thereby minimizing the risk of plate-related complications. Fibular free flap is the most reliable option for mandibular reconstruction, and we believe that the flap should be performed primarily whenever possible.
INTRODUCTION
Mandibular reconstruction continues to be a challenge faced by reconstructive surgeons. There are frequently used options: the fibular free flap and the locking mandibular reconstruction plate fixation. The fibular free flap was first used in mandibular reconstruction by Hidalgo [1]. This flap has been used as the standard method in the reconstruction of segmental mandibular defects. The advantages of fibular free flap over other microvascular free flaps include its consistency and uniformity in width and length, the sufficiency of its pedicle length and vessel diameter, and the ability to incorporate a skin or muscle component with the flap. The fibula is at the opposite end of the body from head and neck, and this allows for a simultaneous 2-team approach and shortens the operative time [2].
Locking mandibular reconstruction plate fixation has been used as a temporary or permanent bone graft substitute in conjunction with a soft tissue free flap for mandibular defects. It provides a predictable, safe, and efficient means for the surgeon to maintain mandibular continuity. The locking system made the screw lock itself to the plate, creating a single functional unit and minimizing the transmission of pressure to the underlying bone. Plate fixation method has many advantages with no risk for donorsite morbidity as well as decreased technically demand and operation time. However, plate-only fixation confers greater risk for plate-related complications (e.g., plate fracture and plate exposure).
Few reports have compared these two methods of mandibular reconstruction. In this study, we compare the results of our mandibular reconstruction cases between the fibular flap and plate fixation. To our knowledge, this is the first study to compare the fibular flap with the plate fixation within Korea.
METHODS
A retrospective chart review of mandibular reconstruction cases treated between 1994 and 2013 revealed that 20 patients with partial mandibulectomy for the extirpation of head and neck tumors underwent mandibular reconstruction. In principle, we reconstructed the defect using a fibular free flap while fixing the bony portion with plates (n=12). In patients at high risk of cancer recurrence, however, we performed only locking plate fixation (n=8) with a soft tissue-only free flap. Data were collected retrospectively through a chart review, including patient age, sex, pathological result, reconstruction method, history of radiotherapy, length of hospital stay, follow-up period, and incidence of complications. Follow-up period was defined as the time from initial reconstruction until revisional operation, in case of any complication.
Patients in the plate fixation group, who had a higher risk of cancer recurrence, underwent mandibular reconstruction with plate-only fixation. In most of these patients, the cancer had already recurred or had advanced too far to be treated, so the mandibular reconstruction was performed with a temporary plate. We used a 2.4-mm reconstruction plate and covered the soft tissue defect with a soft tissue free flap (e.g., radial forearm fasciocutaneous or transverse rectus abdominis musculocutaneous free flap). Six patients received preoperative radiotherapy, and most (7/8) of the patients received radiotherapy after surgery.
In the fibular flap group, mandibular reconstruction was performed immediately upon wide tumor excision. From 2009, three-dimensional computed tomography (CT) for stereolithographic modeling was performed for all patients. The 2.4-mm reconstruction plate was pre-bended over these models. The flap design and elevation was performed using the conventional method over the whole period. The donor site was closed with direct repair or with the use of a split thickness skin graft. Once harvested, the fibular flap is transferred to the recipient site in the head and neck region. We performed 1 or 2 osteotomies along the curvature of resected mandibular segment. The insetting of fibula was usually performed with the pre-bended 2.4-mm reconstruction plate by placing the fibula approximately 1 cm superior to the inferior border of mandible. Then, microvascular anastomosis was performed under microscopy using 9-0 nylon sutures. Eight patients received preoperative radiotherapy, and most (11/12) of the patients received radiotherapy after surgery.
Statistical analysis was performed using the Mann-Whitney test to compare age distribution, length of hospital stay, and follow-up period between the 2 groups. Fisher's exact test was used to compare the sex ratio, pathological type, radiotherapy, and incidence of complication. All data were analyzed using SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). A p-value <0.05 was considered statistically significant.
RESULTS
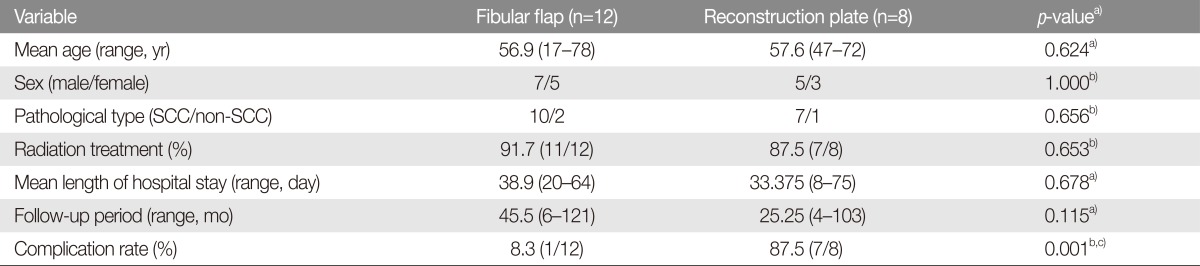
Demographic information and outcomes in each group are shown in Table 1. No significant differences were observed between the groups in term of age, sex, pathological tumor type, history of radiation treatment, length of hospital stay, and follow-up period. The proportion of men was slightly higher than that of women, and age at time of reconstruction was widely distributed. Seventeen of 20 patients were diagnosed with squamous cell carcinoma through histological confirmation. Almost all of the patients had a stage IV disease, except for one case of ameloblastoma. Most of the patients had previously received radiation treatment. The complication rate was significantly lower for the fibular flap group (p=0.001). In these patients, no flap-related complication was identified, with a single patient experiencing a donor-site problem (case 1). Plate-related problems were found in 7 patients in the plate fixation group.
In the fibular flap group, only 1 patient had wound dehiscence at the donor site, which was repaired with direct closure. In the plate fixation group, the plates became exposed in 6 patients and fractured in 1 patient. Most of plate exposure occurred within 6 months of reconstruction, if the patients were treated with radiotherapy. In a patient who did not receive radiation treatment, the plate was exposed at 103 months after the first surgery. In the single case of plate fracture, the patient began to experience malocclusion, trismus, and difficulty in mouth opening about 6 months after surgery (case 2). The plate fracture was confirmed by a radiologic finding at 12 months.
Case 1
A 55-year-old woman had partial hemiglossectomy and right segmental mandibulectomy with an immediate mandibular reconstruction using an osteocutaneous fibular free flap. The donor site was closed primarily, but her lower leg showed signs of compartment syndrome on the day after operation. Thus, we opened the donor wound and applied negative pressure wound therapy (V.A.C. Therapy, KCI USA, San Antonio, TX, USA) for 2 weeks. This wound was completely healed with a split-thickness skin graft. At 50-month visit, the patient remains stable without any problems or cancer recurrence (Fig. 1).

Case 1. A 55-year-old woman had a mandibular reconstruction using an osteocutaneous fibular free flap. The donor wound had dehiscence and was treated with negative pressure therapy, and the wound was completely healed with the use of a skin graft. (A) Preoperative photograph. (B) Photograph at 2 years after surgery. (C) Intraoperative photograph. (D) Donor site scar at 2 years after surgery.
Case 2
A 45-year-old woman was diagnosed with recurrent tongue cancer. The cancer had recurred despite 3 previous resections at another hospital 6 years ago. Because she had shown improvement after neoadjuvant chemotherapy, the head and neck oncological team decided to perform a hemiglossectomy with segmental mandibulectomy and selective neck dissection. The mandible, tongue, and mouth floor were reconstructed using a 2.4-mm reconstruction plate and transverse rectus abdominis musculocutaneous free flap. We decided to apply a temporary plate fixation instead of a fibular free flap because of the risk for cancer recurrence, in which case the fibular flap would have to be removed. We planned a secondary reconstruction with a fibular flap or bone graft after complete cancer remission. The patient recovered without any early complication and was discharged home 5 weeks later, after undergoing a swallowing training. However, the patient began to experience malocclusion, trismus, and difficulty in mouth opening about 6 months after surgery, which were caused by mandibular displacement. As a result, the plate was fractured at about 1 year after surgery. We finally decided to change the reconstruction plate and perform autologous bone grafting using the eighth costal bone. The mandible was reconstructed successfully by this second surgery (Fig. 2).

Case 2. A 45-year-old woman had a mandibular reconstruction using reconstruction plate fixation at first. (A) Preoperative photograph. (B) Photograph at 12 months after surgery. (C) Intraoperative photograph. (D) Radiographs at 1 year after surgery revealed a plate fracture and dislocation of the right temporomandibular joint. (E) Postoperative radiograph after the reconstruction plate change and autologous costal bone graft.
Case 3
A 23-year-old man had a huge mass on his left chin, which had continued to enlarge for 4 years. The mandible was resected, and the defect was immediately reconstructed using a fibular free flap. We elevated the osteocutaneous flap, including a 13-cm×7-cm skin paddle and 15-cm-long fibular bone segment with peroneal vascular pedicles. The bone segment was split by 2 osteotomies and fixed to the mandibular defect with a locking mandibular reconstruction plate. Flap was inset, and the vessels were anastomosed. The mass was diagnosed as an ameloblastoma, a benign tumor originated from the mandible. The patient was followed up for 6 months and recovered without any problem (Fig. 3).

Case 3. A 23-year-old man with an extremely large submandibular mass underwent mandibular reconstruction using a vascularized fibular flap. The mass was diagnosed as ameloblastoma. (A) Preoperative photograph. (B) Photograph at 6 months after surgery. (C, D) A fibular osteocutaneous flap, including a 13-cm×7-cm skin paddle and 15-cm-long fibular bone segment with peroneal vascular pedicles, was elevated. (E) The bone segment was split via 2 osteotomies and fixed to the mandibular defect with a locking mandibular reconstruction plate. Microvascular anastomosis and flap insetting were performed.
DISCUSSION
The fibular flap is currently the first option for mandibular reconstruction. The fibula flap was introduced in 1978 by Taylor [3] and first used clinically for mandibular reconstruction in 1989 by Hidalgo [1]. This versatile osteocutaneous flap simultaneously provides a long bone with a large skin paddle. A bone graft of up to 25 cm and a skin paddle as large as 10×20 cm can be used. The bony structure is excellent for placement of osseointegrated implants or conventional dentures. The thin and pliable skin paddle can also be used for orotracheal reconstruction and transferred as a sensate graft. Multiple skin paddles can be designed within the single flap, based on septocutaneous and musculocutaneous perforators.
We created stereolithographic models using 3-dimensional CT. Exactly fitting the reconstruction plate into the mandibular defect is difficult and time-consuming. It will be impossible to fit exactly unless the plate is pre-bended before the mandibulectomy. We always ensured that we attempted to fit the plate first and mark the points where screws are to be fixed on the mandibular body and ramus.
A CT scan also allows for identification of osteotomy angle before the operation. We used templates made with a ruler. The templates allowed us to accurately perform the osteotomies. With this procedure, the neo-mandible can be made suitable for 3-dimensional mandibular defects, with which the operation and flap ischemic times can be reduced. Many articles have described computer-aided design of mandible cuts for precise reconstruction. Hirsch et al. [4] described the method of preoperative planning for all procedures using detailed 3-dimensional stereolithographic models. Matros et al. [5] introduced the method of simplified osteotomy design.
In case 2, we did not use a fibular flap or any other autologous or tissue-engineered bone components as a primary option. We thought that this choice was reasonable because the patient was at a high risk for recurrence. In compromised patients, surgeons should evaluate reconstructive options with deliberation. Many surgeons choose a relatively simple reconstruction method, such as a combination of plate fixation and soft tissue flap coverage, in such patients because of the idea of "days of life lost". Previous studies have reasoned that the reconstruction plate can be used both as a permanent and as a temporary substitute for bone graft [6,7]. However, the clinical context in which reconstruction plates can be used are limited. Head et al. [6] suggested that a soft tissue free flap combined with a bridging mandibular reconstruction plate is a reasonable alternative to vascularized bone-containing flap reconstruction for select lateral oromandibular defects. However, plate fracture might occur more frequently and earlier in dentulous patients than in edentulous patients [7]. Although many reports have described that plate-only reconstruction could provide a stable and rigid support, our current experience suggests that it carries a high risk for plate-related complications.
The effect of radiation treatment has remained unclear despite the number of studies published on this topic. Some authors have reported a higher incidence of complications in irradiated patients. Schoning et al. [8] reported that irradiation was found to be associated with a significantly higher rate of plate-related complications and revision (53.6% vs. 31.5%). Ettl et al. [9] also explained that patients who received neoadjuvant radiochemotherapy had a significantly higher risk (p=0.027) for infection-related plate losses (46.1%) than patients without preoperative treatment (28.9%). Meanwhile, Kammerer et al. [10] and Wang et al. [11] reported that mandibular reconstruction using a titanium plate was not adversely affected by radiation treatment. In a meta-analysis on alloplastic mandibular reconstruction [12], radiotherapy seemed to be a relative risk factor for complications (1.387; p=0.014) and plate loss (1.585; p=0.006).
In the present study, we thought that radiation treatment would have a negative effect on reconstruction plate. In irradiated patients, the plates were exposed earlier than in non-irradiated patients. Most plate exposures occurred at about 6 months after surgery. By contrast, the only non-irradiated plate was exposed at 103 months. This means that radiation could have had a negative effect on the plate and flap, especially in the earlier stage. In the earlier stage when the flap is unstable, the vascularized bone can reinforce the rigid fixation of reconstruction plate, thus the platerelated complications rarely occur.
Some investigators have referred to early complications as those occurring during the first 6 weeks [9], 3 months [12], and mostly 6 months [13,14] after surgery. According to these studies, patients should be followed closely for 6 months as the shortest period to monitor for possible complications. In our study, the mean follow-up period of 45.5 months was enough to evaluate the risk of earlier complications.
It is known that the type of the soft tissue flap is a variable risk factor for plate exposure [15], with thinner flaps more likely to break down and expose the plates. For this reason, some surgeons prefer thicker musculocutaneous flaps, pectoralis major flap for example, to the fasciocutaneous flap. However, the pectoralis major flap often results in poor functional and aesthetic outcomes because of excessive bulkiness, and decreased neck mobility caused by tethering by the flap pedicle. In our practice, microvascular fasciocutaneous free flap reconstructions, radial forearm flap or anterolateral thigh flap for example, are generally preferred. Indeed, most patients (7/8) in the plate fixation group underwent the radial forearm fasciocutaneous free flap as the soft tissue coverage over the plate. This might explain the higher rates of plate exposure in this group.
There are some articles that compare outcomes between the fibular flap and plate fixation. However, this had not been reported within Korea. Our study shows that the fibular flap group has lower plate-related complication rate than the plate fixation group. We suggest that the vascularized osteocutaneous flap should be considered for a stable mandibular reconstruction, whenever possible. Our present study has a small number of cases because mandibular reconstructions are relatively uncommon. However, the number of patients who undergo mandibulectomy is growing, and the need for mandibular reconstruction is also on the rise. Future studies with long-term follow-up periods and larger groups are needed. The causative factors of fracture of each type of reconstruction plate will have to be quantified through experimental studies.
Locking mandibular reconstruction plate fixation for mandibular reconstruction after tumor extirpation is associated with a high rate of plate-related complications, which includes plate fracture and exposure. The fibular free flap provides a more stable and rigid support for the plate bearing the loading force of the temporomandibular joint motion and masticatory movement. It also provides additional soft tissue support around the plate for minimizing the risk of plate exposure. The authors recommend that fibular free flap reconstruction, being the most reliable option for mandibular repair, should be performed primarily.
Notes
No potential conflict of interest relevant to this article was reported.