|
 |
- Search
| Arch Craniofac Surg > Volume 20(5); 2019 > Article |
|
Abstract
Background
Treatment for venous malformations of the head and neck includes sclerotherapy, surgical resection, or a combination of both. Surgical resection can remove or reduce the volume of vascular lesions; however, surgery can cause postoperative scarring and potential surgical complications. This study sought to determine the effectiveness of surgery for the treatment of venous malformations of the head and neck.
Methods
A retrospective review of the medical records of patients who received surgeries for venous malformations of the head and neck from January 2011 to July 2019 was performed. Using clinical photographs, preoperative and postoperative Doppler ultrasonography, outpatient clinic records, and operation records, the postoperative result and complications were evaluated for each case.
Results
Among patients who visited our vascular anomalies clinic, 43 patients (ratio of male to female= 24:19) received surgeries for venous malformations of the head and neck. Twenty-nine patients had undergone surgery only, five patients received sclerotherapy after surgery, and nine patients received surgery after preoperative sclerotherapy. In postoperative evaluations, the result was excellent in 24 patients, good in 18 patients, and poor in one patient. Four patients experienced a recurrence of lesions with lagophthalmos, drooping of the corner of the mouth, partial wound necrosis, and scar widening found in one patient each.
Vascular anomalies occur as a result of abnormal vascular development and include skin and mucosa abnormalities, and various soft tissue abnormalities. The current classification of vascular anomalies was introduced by Mulliken and Glowacki [1]. This classification was based on biological, clinical, and histological features, according to which the International Society for the Study of Vascular Anomalies (ISSVA) established the current classification system.
The ISSVA classification system divides vascular abnormalities into vascular tumors and vascular malformations; vascular malformations include capillary malformations, lymphatic malformations, venous malformations (VMs), and arteriovenous malformations. VMs are the most common vascular malformation [2], where one in 5,000 people is diagnosed with VMs. VMs are the result of abnormal development of the venous network, resulting in thin and relaxed vascular walls and dysfunctional veins [3]. VMs can induce severe chronic pain, and result in minor disfigurement and discoloration depending on the size of the lesion.
Treatments for VMs include surgical removal, sclerotherapy, and sclerotherapy combined with surgery [4]. VMs in the head and neck area account for 40% of all VM cases, and sclerotherapy is generally preferred over surgery. Surgery is often used as an additional treatment [5]. Furthermore, the indications for surgical treatment of VMs of the head and neck have not been clearly established. Thus, we aimed to analyze the effectiveness of surgical treatment in patients with VMs in the head and neck area.
This study is a retrospective analysis of patients at our vascular anomalies clinic who had been diagnosed with VMs of the head and neck and had undergone surgery between January 2011 and July 2019. Patients were classified according to sex, age, and the type of treatment (surgery only, surgery after preoperative sclerotherapy, and postoperative sclerotherapy). Moreover, the severity of VMs were classified based on the 4-grade classification of VMs by Goyal et al. [6]. Well-defined VMs sized 5 cm or smaller were defined as grade 1, and welldefined VMs sized greater than 5 cm were defined as grade 2A. Ill-defined VMs sized 5 cm or smaller were defined as grade 2B, and ill-defined VMs sized greater than 5 cm were defined as grade 3.
Postoperative outcomes were classified as poor, good, or excellent based on a postoperative image test, reduction of VM size, and the patient’s subjective symptoms. Three plastic surgeons (JYR, PSE, and HYC) participated in the postoperative evaluation. Considering to the differing opinions on the evaluation, three evaluators were composed. Poor was defined as almost no improvement in symptoms or imaging results, and good was defined as adequate reduction in VM size and symptom relief. Excellent was defined as complete elimination of the VM as determined by a radiologic follow-up. Based on this, patient outcomes were classified into excellent, good, and poor. Further postoperative complications were also investigated.
A total of 43 patients were diagnosed with VMs in the head and neck area and underwent surgical treatment between January 2011 and July 2019. Of these patients, 24 were male and 19 were female.
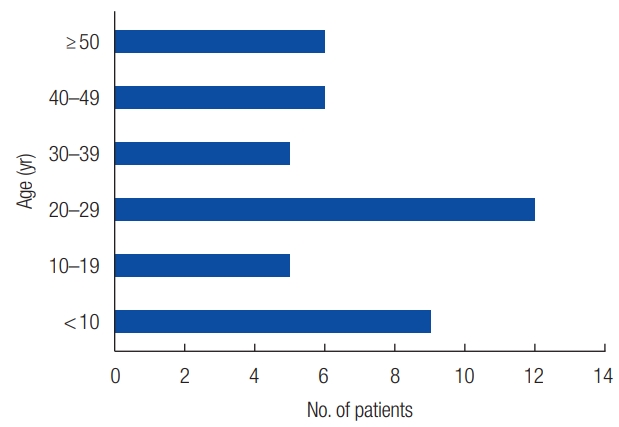
There were nine patients aged <10 years, five patients between the ages of 10–19 years, 12 patients between the ages of 20–29 years, five patients between the ages of 30–39 years, six patients between the ages of 40–49 years, and six patients aged ≥50 years (Fig. 1). Twenty-nine patients had surgical excision only, five patients had surgical excision followed by sclerotherapy, and nine patients had sclerotherapy followed by surgical excision. Per the grading suggested by Goyal et al. [6], 36 were grade 1, three were grade 2A, three were grade 2B, and one was grade 3.
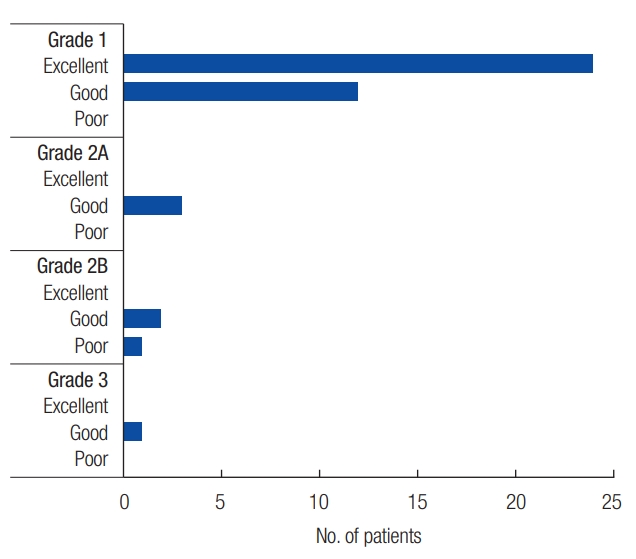
Regarding postoperative assessment, 24 patients had excellent outcomes, 18 had good outcomes, and one had a poor outcome. Among patients with grade 1 VM, 24 patients had excellent outcomes and 12 had good outcomes, with no patient experiencing a poor outcome. Among patients with grade 2A, three patients had good outcomes, with no patient having excellent or poor outcomes. Among patients with grade 2B, two patients had good outcomes and one had a poor outcome, with no excellent outcomes. One patient with grade 3 had a good outcome (Fig. 2). Regarding postoperative complications, four patients experienced a lesion relapse, namely lagophthalmos (n=1), drooping of the corner of the mouth (n=1), partial wound necrosis (n=1), and scar widening (n=1).
A 38-year-old woman presented to the hospital with a bulky lower lip. She was diagnosed with VM of the lower lip based on preoperative T2-weighted magnetic resonance imaging (MRI). Excision of the lesion, including some of the lower lip skin and mucosa, was performed. Postoperative Doppler ultrasonography confirmed that the lesion was almost completely excised. The result in this case was excellent as the symptoms, contours of the lip and radiologic findings all improved (Fig. 3).
A 55-year-old man presented to the hospital with a bulky lower cheek. He was diagnosed with VM of the lower cheek based on preoperative T2-weighted MRI. Excision of the lesion, including some skin in the right lower cheek, was performed. Postoperative Doppler ultrasonography confirmed that the lesion was almost completely excised. In this case, the result was excellent since the symptoms, bulkiness and radiologic findings were all improved (Fig. 4).
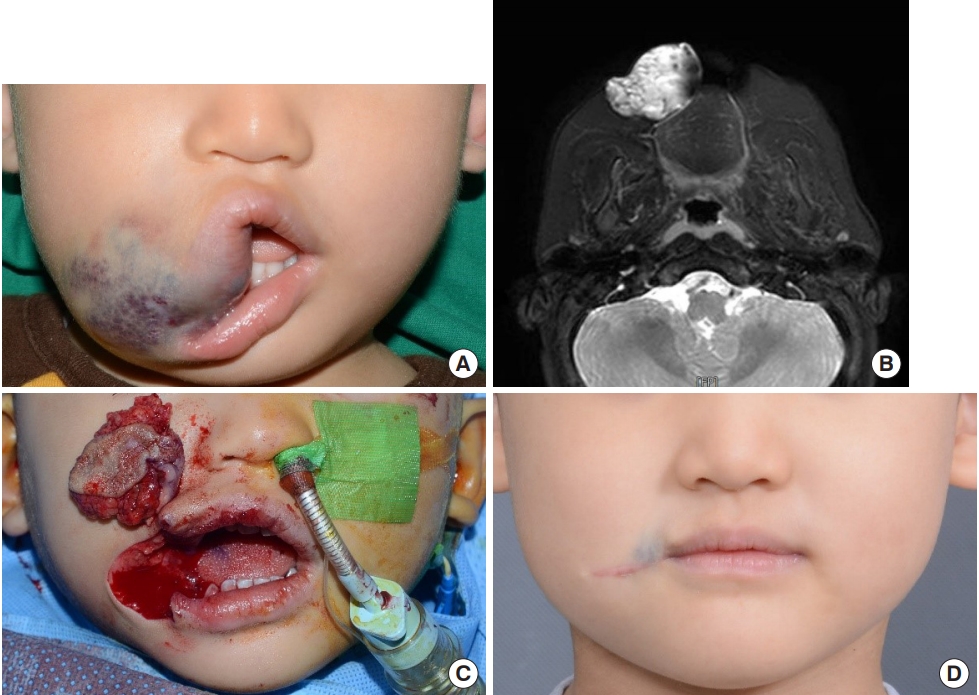
A 5-year-old boy presented to the hospital with a bluish bulging mass encroaching on the right oral commissure. He was diagnosed with VM of the right upper lip and oral commissure based on preoperative T2-weighted MRI. After excising the VM including part of the skin from the right oral commissure area, a neo-oral commissure was reconstructed. While reconstructing the neo-oral commissure, a 1-mm medial overcorrection was performed to correct for the lengthening of the right oral commissure to prevent scar contracture after surgery. After 2 years, the bulging mass recurred, for which a second excision was performed; until 5 months after surgery, the patient showed good outcomes without lesion recurrence. The case was also decided as excellent as the postoperative symptoms, lip contours and radiologic findings were all good (Fig. 5).
VMs is a challenging condition to treat clinically and is associated with high morbidity and frequent recurrence after treatment; therefore, a multidisciplinary approach is crucial for the treatment of VMs [7]. As VMs generally occur in superficial areas, it is easily detected and diagnosed. However, lesions located deep within the head and neck area need to be diagnosed via Doppler ultrasonography and MRI, as do other vascular anomalies. Doppler ultrasonography can be used to identify the type of vascular anomaly, and MRI can be used to examine the size and depth of the lesion as well as its relationship with surrounding soft tissue [8]. VMs show intermediate signal intensity on T1-weighted images and high signal intensities on T2-weighted images. Particularly, for VMs of the head and neck area, where the lesions tend to expand deeply into the surrounding tissue, MRI plays a critical role in accurately understanding the relationships between the lesion and surrounding soft tissues [9]. Appropriate treatment plans can be developed only with an accurate diagnosis of the size and depth of the lesion, and its relationship with surrounding tissues.
Treatment for VMs includes surgical excision, sclerotherapy, and a combination of both surgery and sclerotherapy. Sclerotherapy is generally a less invasive treatment that produces adequate therapeutic effects when used individually. Sclerotherapy may be an effective preoperative adjuvant therapy to reduce bleeding after surgery. Further, sclerotherapy is preferred in cases in which the lesion is located near an important structure in the head and neck area where surgical treatment is likely to result in serious complications. Sclerotic agents such as ethanol, bleomycin, and sodium tetradecyl sulfate are effective at treating VMs [10-12].
Surgical resection can be effective in patients with pain or pronounced disfigurement. In particular, well-defined and well-localized VMs may be curable via surgical resection. In such cases, complete resection of the lesion is crucial, and functional as well as anatomical factors must be considered. Even if complete resection of the lesion is impossible, partial resection can reduce the volume of the mass, and thus, lead to an improved aesthetic outcome.
Because the head and neck is the most exposed part of the human body, sclerotherapy is preferred to surgical excision, as the latter may cause unwanted, excessive scar formation [5,8]. However, sclerotherapy alone cannot effectively reduce the volume of VMs and cannot alleviate symptoms caused by the mass effect. If complete resection is feasible through surgical resection, both the mass and debulking effects can be achieved; even if complete resection is not possible, an adequate debulking can be achieved. However, because the head and neck area contains many important anatomical structures, it is imperative that these structures are not damaged or functionally impaired during surgical resection. Particularly, both functional and aesthetic aspects must be considered when performing surgery in the lip area [8]. In case 3 of our study, a neo-oral commissure was reconstructed for the new defect that occurred after excision of VMs. If the neo-oral commissure is reconstructed based on the length from the contralateral cupid’s bow to the oral commissure, scar contracture would cause an infero-lateral migration of the neo-oral commissure; thus, we performed a 1-mm medial overcorrection [13].
VM grade 1 as suggested by Goyal et al. [6] refers to well-defined masses that are smaller than 5 cm, and most of these cases are suitable for surgical excision, as good outcomes are anticipated. In our study, all patients who had excellent outcomes had grade 1 VM. However, most patients with grade 2A or 2B were considered to have good outcomes, with only one patient having poor outcomes. This is surmised to be due to the debulking effects that cannot be obtained through sclerotherapy alone, and diminished mass effect on surrounding soft tissues.
Four patients had a recurrence of VMs, for which secondary surgical excision was performed. In addition, a patient who had undergone surgical excision for a lesion in the orbital area later developed lagophthalmos, and thus, a corrective surgery was performed. A patient who had undergone excision for a lesion near the Risorius later developed drooping at the corner of the mouth; thus, muscle suspension was performed at the corner of the mouth. The same patient developed wound necrosis after the excision of VMs in the tongue; thus, secondary debridement was performed. One patient showed scar widening at the incision site; thus, fractional laser therapy was performed. All complications that occurred in this study were corrected through secondary surgeries.
In conclusion, sclerotherapy is a less invasive treatment for VMs that leaves no scarring and has little risk of hemorrhage; however, it cannot markedly reduce the volume of the lesion. In contrast, surgical excision can reduce the size of the lesion or completely remove it; however, surgery is invasive and leads to scars. Furthermore, surgery can result in postoperative complications if the lesion is located near important structures; therefore, there is a risk of serious postoperative hemorrhage. We were able to achieve good outcomes with a low incidence of complications by actively performing surgical treatments to not only remove the lesions, but also resolve the aesthetic problems caused by bulky lesions in the head and neck area. Therefore, although sclerotherapy is effective, surgery is essential for treating VMs in the head and neck area.
Notes
Fig. 3.
Case 1: venous malformation (VM) on the lip. (A) Bulky lower lip was observed. (B) Preoperative magnetic resonance imaging showed a VM on the lower lip. (C) Postoperative contour of the lip was improved. (D) Postoperative Doppler ultrasonography showed almost removed lesions.
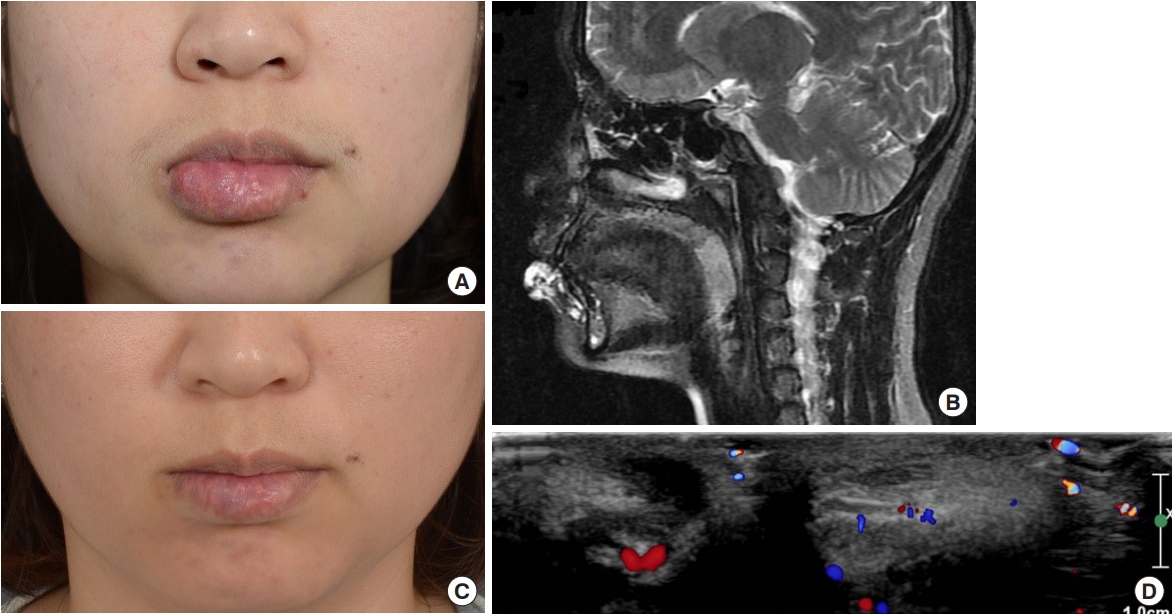
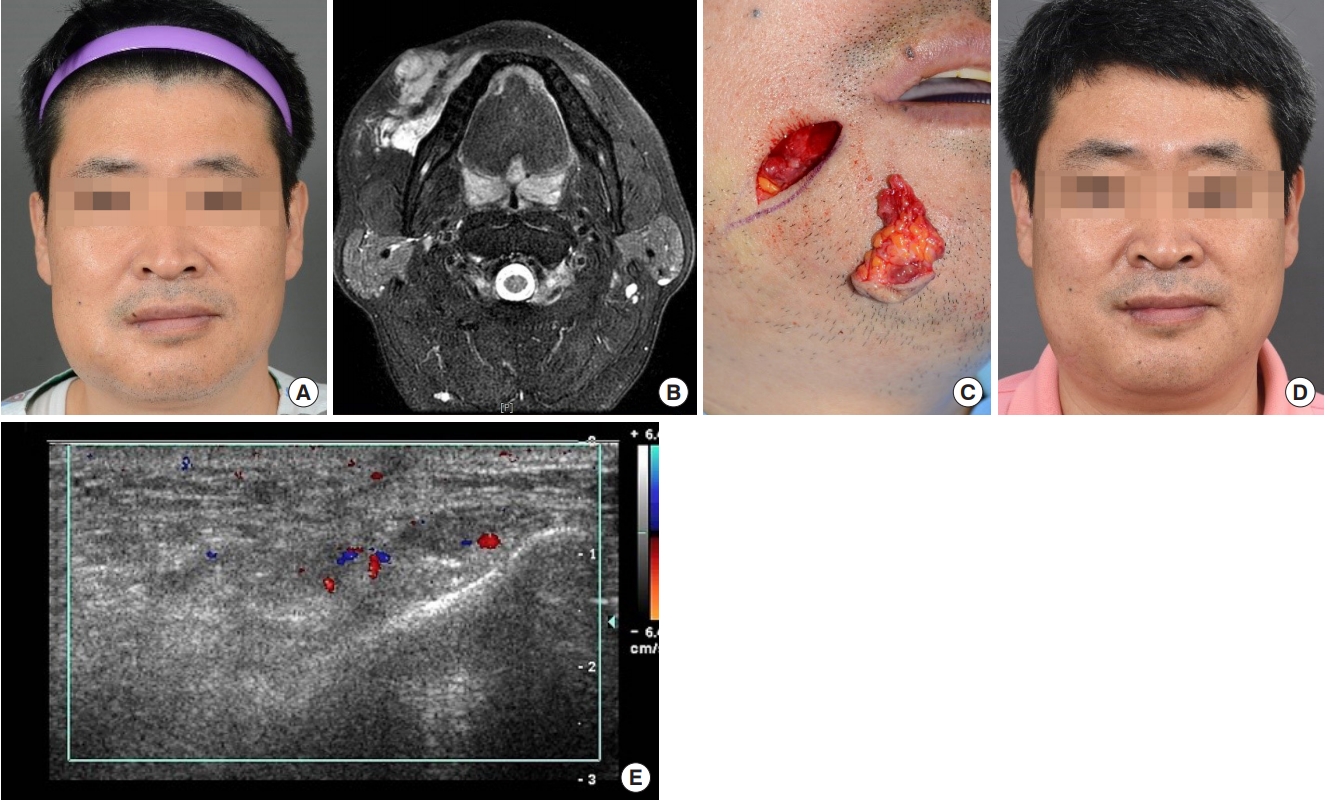
Fig. 4.
Case 2: venous malformation (VM) on the right cheek. (A) Bulky right cheek was observed. (B) Preoperative magnetic resonance imaging showed a VM on the right cheek. (C) VM was surgically excised. (D) Postoperative contour of the right cheek was improved. (E) Postoperative ultrasonography shows that most of the lesions have been removed.
REFERENCES
1. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22.


2. Wieck MM, Nowicki D, Schall KA, Zeinati C, Howell LK, Anselmo DM. Management of pediatric intramuscular venous malformations. J Pediatr Surg 2017;52:598-601.


3. Seront E, Van Damme A, Boon LM, Vikkula M. Rapamycin and treatment of venous malformations. Curr Opin Hematol 2019;26:185-92.


4. Limaye N, Kangas J, Mendola A, Godfraind C, Schlogel MJ, Helaers R, et al. Somatic activating PIK3CA mutations cause venous malformation. Am J Hum Genet 2015;97:914-21.



5. Steiner F, FitzJohn T, Tan ST. Surgical treatment for venous malformation. J Plast Reconstr Aesthet Surg 2013;66:1741-9.


6. Goyal M, Causer PA, Armstrong D. Venous vascular malformations in pediatric patients: comparison of results of alcohol sclerotherapy with proposed MR imaging classification. Radiology 2002;223:639-44.


7. Park H, Kim JS, Park H, Kim JY, Huh S, Lee JM, et al. Venous malformations of the head and neck: a retrospective review of 82 cases. Arch Plast Surg 2019;46:23-33.




8. Ryu JY, Lee JS, Lee JW, Choi KY, Yang JD, Cho BC, et al. Clinical approaches to vascular anomalies of the lip. Arch Plast Surg 2015;42:709-15.




9. Zheng JW, Mai HM, Zhang L, Wang YA, Fan XD, Su LX, et al. Guidelines for the treatment of head and neck venous malformations. Int J Clin Exp Med 2013;6:377-89.


10. Steiner F, FitzJohn T, Tan ST. Ethanol sclerotherapy for venous malformation. ANZ J Surg 2016;86:790-5.


11. Azene E, Mitchell S, Radvany M, Agrawal N, Eisele D, Weiss C. Foamed bleomycin sclerosis of airway venous malformations: the role of interspecialty collaboration. Laryngoscope 2016;126:2726-32.


- TOOLS
-
METRICS

-
- 14 Crossref
- Scopus
- 5,204 View
- 134 Download
- Related articles in ACFS
-
A practical approach to nasal reconstruction in Asian patients 2021 October;22(5)
A case of Merkel cell carcinoma of the head and neck2019 December;20(6)
A surgical approach to linear scleroderma using Medpor and dermal fat graft 2019 April;20(2)