|
 |
- Search
| Arch Craniofac Surg > Volume 21(5); 2020 > Article |
|
Abstract
Orthognathic surgeries often utilize rigid fixation for stabilization of the osteotomy site. The longterm fate of rigid fixations is still under investigation, and whether they should be routinely removed is under debate despite their low complication rates. Here, we report a case where a 26-year-old man suffered high-velocity trauma to his face 7 years after a two-jaw surgery. Computed tomography examination revealed a zygomaticomaxillary complex fracture, and open reduction and internal fixation was performed along with anterior maxillary wall reconstruction using absorbable mesh. Intraoperative examination revealed a broken L-shaped titanium plate near the fracture site with multiple bony fragments near each titanium screw. The rigid titanium system may have caused comminution of the fracture pattern, worsening the severity of the fracture.
Orthognathic surgeries are performed to treat congenital and acquired facial deformities, to improve facial aesthetics, to excise tumors, and more. Despite their versatility, orthognathic surgeries are not without drawbacks. Complications associated with orthognathic surgeries range from postoperative bleeding, temporary nerve injury, infection to temporomandibular joint problems, vision impairment, and most importantly, relapse [1-4].
Rigid internal fixation is widely used for stabilization of the osteotomy site during orthognathic surgery. In craniofacial surgery, there is a consensus that symptomatic plates and screws should be removed, but routine removal of asymptomatic plates is still debated [5-7]. After orthognathic surgeries, patients are advised to avoid trauma, since skeletal strength may be compromised. Here, we report a case of a trauma patient who suffered a zygomaticomaxillary fracture, 7 years after receiving a two-jaw operation.
A 26-year-old man without underlying disease visited the emergency room after a motorcycle accident. According to the patient, the patient had previously undergone two-jaw surgery 7 years ago for Class III malocclusion. Unfortunately, the previous operation record was not obtainable. Physical examination revealed severe facial edema and ecchymosis of his left side, and no evidence of entrapment of the extraocular muscles, trismus, or malocclusion.
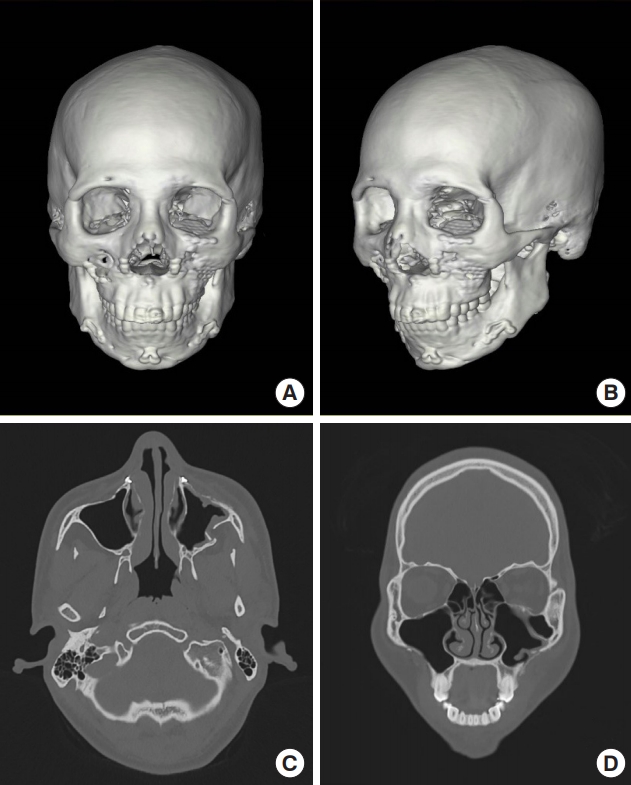
Computed tomography (CT) examination revealed a zygomaticomaxillary complex fracture of the left side, involving the zygomaticomaxillary buttress and the inferior orbital rim. The frontozygomatic suture line was not displaced. The fracture line of the anterior wall was about 2 mm medial to the plate of the zygomaticomaxillary buttress, and the plate itself was also bent into the maxillary sinus (Fig. 1).
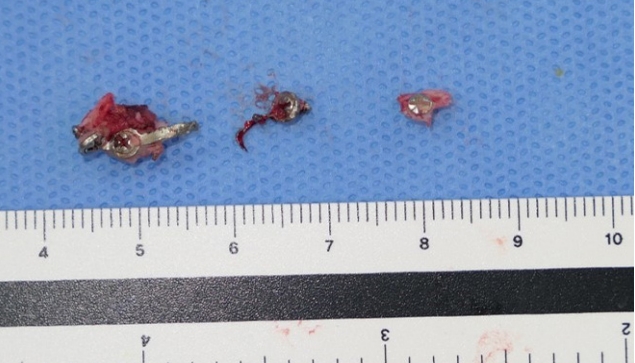
Seven days after the trauma, the patient was taken to the operating room. Through the gingivobuccal incision, the fracture site was explored. Several comminuted bone fragments were observed, and the lateral plate was tearing through the maxillary sinus mucosa. The lateral plate, which appeared bent but intact on CT, was broken into two pieces with multiple bony fragments around each screw (Fig. 2). The plate and screws were removed, and the reduction was performed using a zygomatic elevator. Also, small nonviable bone fragments were debrided. Due to the comminution of the anterior wall and bony defect after removal, anterior wall reconstruction and restoration of the zygomaticomaxillary buttress was performed using a single absorbable mesh and screws tailored to fit the curvature of the buttress (Osteotrans-MX; Takiron Co., Ltd., Osaka, Japan). Also, fixation of the infraorbital rim was performed through a subciliary incision. Since bony continuity of the zygomaticomaxillary buttress and frontozygomatic suture was restored after the reduction, fixation was only performed at the infraorbital rim and the zygomaticomaxillary buttress.
The patient was discharged on the 5th day without acute postoperative complications. A follow-up CT examination was performed 30 days postoperatively. The CT examination revealed a well-reduced zygomaticomaxillary complex and bony continuity of the anterior maxillary wall with the absorbable mesh (Fig. 3).
It is necessary to advise patients to avoid facial trauma after orthognathic surgery, especially during the first few weeks when bony healing is under progress. However, due to the scarcity of documented cases, it is difficult to know when bony integrity is fully recovered after orthognathic surgery. Wilson and Iovino [8] reported a case of a 21-year-old man who was involved in a traffic accident 6 weeks after a two-jaw surgery. The patient suffered anterior maxillary wall fracture and inferior orbital rim fracture with severe comminution, requiring open debridement of bony fragments and reduction of entrapped extraocular muscles. The patientãs anterior wall was not reconstructed due to severe comminution.
Our patient demonstrates a rare case of a delayed facial bone fracture after a two-jaw surgery. Several studies have analyzed bony stability after Le Fort I osteotomy with rigid fixation, but the exact timing of complete bony healing is still under investigation [9,10]. In our case, the patient suffered trauma 7 years after the initial two-jaw operation. Preoperative CT examination showed complete bony continuity along the suspected initial Le Fort I osteotomy line without any bony gap (Fig. 1). Previous operation record was unavailable, hence initial advancement amount is unknown, but our patient demonstrated complete bony healing even at the pterygomaxillary junction.
Intraoperative findings revealed multiple small bone fragments around each screw of the broken plate. Nonviable fragments were debrided. The rigidity of the titanium plate may have been the cause of comminution of the anterior wall of maxilla while breaking into two pieces. In a mechanical strength and stiffness test study comparing biodegradable and titanium osteofixation systems, titanium systems were significantly stronger and stiffer than biodegradable systems [11]. During the acute postoperative phase, such mechanical strength and rigidity may help prevent relapse. However, as in our case, such rigidity may aggravate the severity of fracture in unexpected trauma. Also, the use of foreign bodies in a non-sterile oral field carries the risk of being a source of acute and delayed infection, foreign body reaction, and blood-borne bacteria colonization leading to recurrent infections [12].
When the anterior wall of the maxillary sinus is comminuted, rigid fixation using the conventional methods with straight or L-shaped titanium plates may be difficult. Without proper reconstruction of the anterior wall of the maxillary sinus, complications such as chronic sinusitis, rhinitis, pain may occur [13]. In our patient, anterior wall reconstruction was performed using an absorbable mesh molded to fit the curvature of the zygomatic buttress. On the contrary, absorbable fixation systems near sinuses have been reported to cause delayed infection during the degeneration phase which may take up to 3 years [14], leading to sinusitis or mucocele formation. Therefore patients should be followed for any delayed complications when absorbable materials are used near the sinuses.
Previous studies have shown comparable strength of the absorbable system to conventional titanium system in facial bone surgeries [15,16]. Thirty-day postoperative CT showed restored continuity of the anterior wall of the maxillary sinus and the zygomaticomaxillary buttress. The patient did not complain of complications such as rhinitis, sinusitis, or pain 6 months postoperatively.
Notes
REFERENCES
1. el Deeb M, Wolford L, Bevis R. Complications of orthognathic surgery. Clin Plast Surg 1989;16:825-40.


2. DãAgostino A, Trevisiol L, Gugole F, Bondi V, Nocini PF. Complications of orthognathic surgery: the inferior alveolar nerve. J Craniofac Surg 2010;21:1189-95.


3. Jung GS, Kim TK, Lee JW, Yang JD, Chung HY, Cho BC, et al. The effect of a condylar repositioning plate on condylar position and relapse in two-jaw surgery. Arch Plast Surg 2017;44:19-25.




4. Patel PK, Morris DE, Gassman A. Complications of orthognathic surgery. J Craniofac Surg 2007;18:975-85.


5. Orringer JS, Barcelona V, Buchman SR. Reasons for removal of rigid internal fixation devices in craniofacial surgery. J Craniofac Surg 1998;9:40-4.


6. Murthy AS, Lehman JA Jr. Symptomatic plate removal in maxillofacial trauma: a review of 76 cases. Ann Plast Surg 2005;55:603-7.


7. Nagase DY, Courtemanche DJ, Peters DA. Plate removal in traumatic facial fractures: 13-year practice review. Ann Plast Surg 2005;55:608-11.


8. Wilson GW, Iovino WM. Severe facial trauma after orthognathic surgery with rigid fixation. J Oral Maxillofac Surg 1989;47:640-2.


9. Ueki K, Miyazaki M, Okabe K, Mukozawa A, Marukawa K, Moroi A, et al. Assessment of bone healing after Le Fort I osteotomy with 3-dimensional computed tomography. J Craniomaxillofac Surg 2011;39:237-43.


10. Brandtner C, Hachleitner J, Rippel C, Krenkel C, Gaggl A. Long-term skeletal and dental stability after orthognathic surgery of the maxillo-mandibular complex in Class II patients with transverse discrepancies. J Craniomaxillofac Surg 2015;43:1516-21.


11. Chu SG, Lee JS, Lee JW, Yang JD, Chung HY, Cho BC, et al. Comparisons among four types of absorbable plates used for internal fixation of zygomaticomaxillary complex fractures. J Craniomaxillofac Surg 2019;47:383-8.


12. Dobbins JJ, Seligson D, Raff MJ. Bacterial colonization of orthopedic fixation devices in the absence of clinical infection. J Infect Dis 1988;158:203-5.



13. Ballon A, Landes CA, Zeilhofer HF, Herzog M, Klein C, Sader R. The importance of the primary reconstruction of the traumatized anterior maxillary sinus wall. J Craniofac Surg 2008;19:505-9.


14. Lee HR, Shin HK, Lee DL, Jung GY. Delayed-onset methicillin-resistant Staphylococcus aureus infection at 18 months after absorbable plate fixation for zygomaticomaxillary complex fracture. Arch Craniofac Surg 2016;17:229-32.




- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 3,442 View
- 96 Download
- Related articles in ACFS
-
Oroantral fistula after a zygomaticomaxillary complex fracture2019 June;20(3)
Surgical Methods of Zygomaticomaxillary Complex Fracture2016 December;17(4)