INTRODUCTION
Primary cutaneous marginal zone B-cell lymphoma (PCMZL) is a very uncommon neoplasm [
1,
2]. PCMZL mainly occurs in Black individuals, and Asians have a particularly low incidence [
2,
3]. The most common locations of PCMZL are the trunk and upper extremity, and it less frequently occurs on the head and neck [
1,
3]. PCMZL is often misdiagnosed due to its atypical clinical manifestations [
4,
5]. In this report, we present a rare case of PCMZL that occurred on the face of an Asian patient.
CASE REPORT
A 51-year-old man visited our hospital with skin lesions on the forehead and nose tip that he had incidentally detected 2 months ago. The patient had no other comorbidities or relevant medical history other than taking aspirin for atrial fibrillation. A physical examination demonstrated a 0.8├Ś0.8 cm papule at the forehead and a 2.5├Ś2.0 cm patch at the nose tip with erythema. No symptoms such as pain, tenderness, or bleeding were observed in either lesion. There were no masses on the other parts of the body. The C-reactive protein level was normal in the laboratory test. His recent contact history, travel history, and food history were not noteworthy. So, the possibility of infection was low.
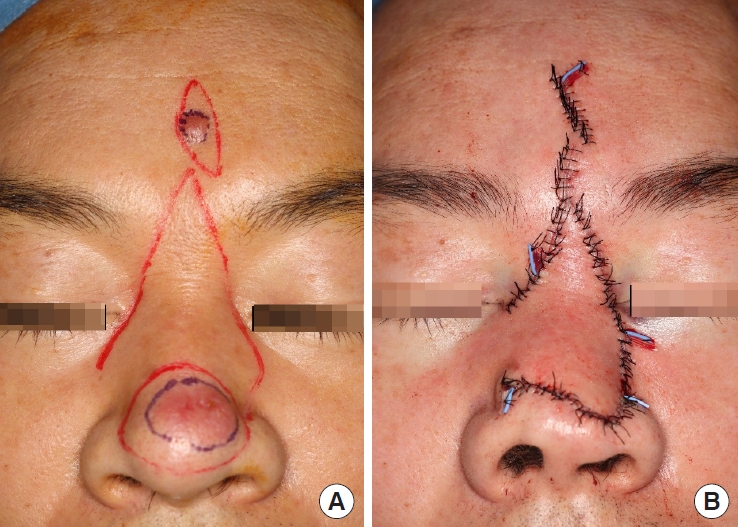
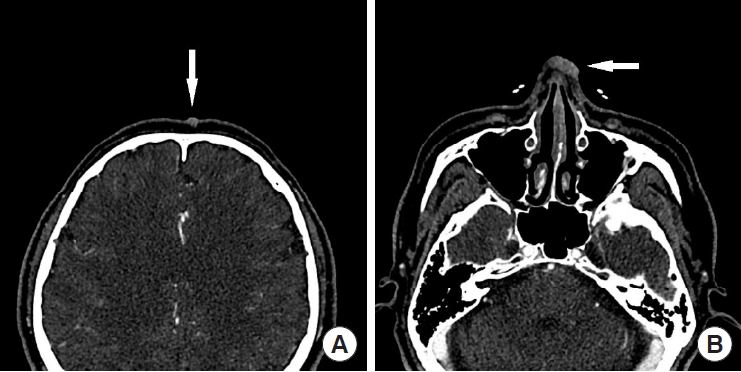
The mass had recently exhibited rapid growth in 2 months, making it necessary to evaluate its potential for malignancy. Histopathological examination of a punch biopsy showed lymphoid aggregations with multiple granulomas. The tumor was therefore suspected to be a lymphoma. Complete blood count and lactate dehydrogenase (LDH) levels were normal. Contrast-enhanced facial computed tomography (CT) revealed a 0.8├Ś0.8 cm mass on the forehead and a 2.5├Ś2.0 cm mass on the nose tip. Both lesions showed homogeneous enhancement and involvement extending from the skin to the subcutaneous layer (
Fig. 1) Enlargement of lymph nodes were not seen including the neck.
Excisional surgery was done with a 3ŌĆō5 mm safety margin. To reduce the risk of nasal asymmetry, the safety margin was set unevenly. After confirmation of tumor free margins by frozen biopsy, the defect on the nasal tip was reconstructed with a V-Y advancement flap. The forehead was covered with a local advancement flap (
Fig. 2). A histopathological examination demonstrated that the forehead and nasal tumors were PCMZL with lymphoid aggregations and multifocal granulomas (
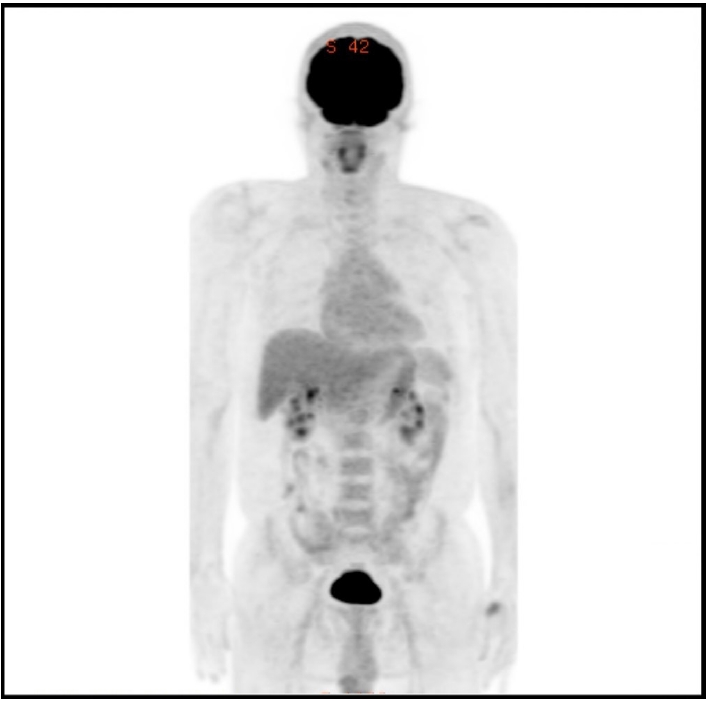
Fig. 3). After discharge, the patient was referred to the hemato-oncology department. Complete blood count, LDH, and beta-2 microglobulin values were normal in follow-up laboratory tests. Positron emission tomography-computed tomography (PET-CT) showed no lymph node invasion or distant metastasis (
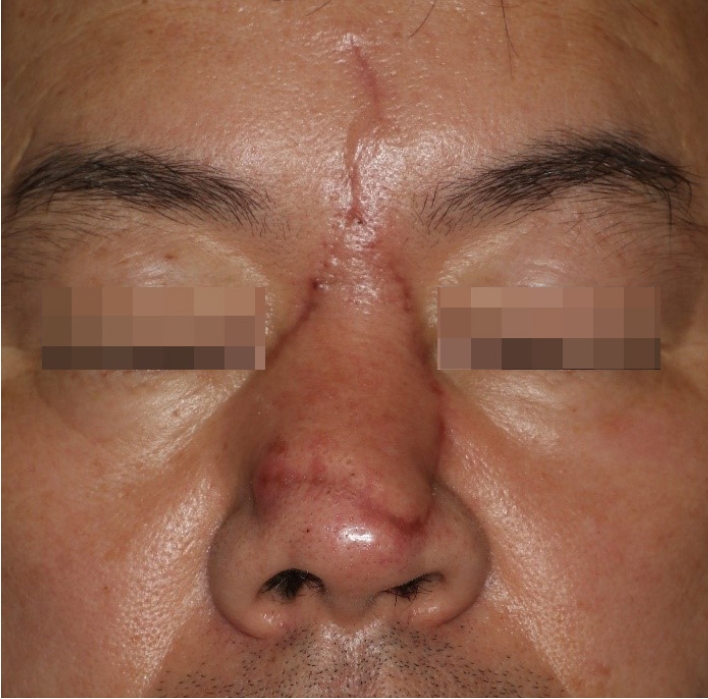
Fig. 4). No postoperative complications were seen and the surgical site was found to be well healed 6 months after the reconstruction without signs of recurrence (
Fig. 5). The patient is under follow-up at the hemato-oncology department with normal laboratory tests values and without adjuvant radiotherapy or immunochemotherapy.
DISCUSSION
PCMZL is a subgroup of primary cutaneous B-cell lymphomas, which belong to the larger category of extranodal B-cell non-Hodgkin lymphoma [
6,
7]. PCMZL accounts for about 2-7% of all primary cutaneous lymphomas [
1,
8]. It appears as small, reddish- purple, single or multiple papules or nodules. PCMZL mainly occurs on the trunk and upper extremity, although it can infrequently occur on the head [
1,
9]. In this case, PCMZL presented as a papule on the forehead and a patch on the nose tip.
PCMZL most often occurs in middle-aged adults, and its incidence is higher in men than in women [
1,
2]. The prognosis of PCMZL is favorable, with a 5-year survival rate exceeding 95% [
1,
10]. The physiopathology of PCMZL is not precisely understood, although it is thought that lymphoma develops through a reactive inflammatory lymphoproliferative process due to stimulation by chronic antigens such as viruses and bacteria [
4]. Several case reports have suggested that PCMZL and
Borrelia burgdorferi infection may be related, but no such cases have been reported in Asians [
6]. In this case, a test for
B. burgdorferi infection was not performed because South Korea is not an endemic area of this bacterium and the patient did not have any symptoms suggestive of Lyme disease. PCMZL is often asymptomatic as in this case [
5]. Because of its potential for misdiagnosis as an infection or a benign mass, detailed imaging studies and laboratory tests are necessary. Above all, it is appropriate to perform a punch biopsy before excision surgery.
PCMZL is primarily diagnosed through histopathological and immunohistochemical examinations of an excisional biopsy specimen [
4,
11]. The characteristic feature of PCMZL on a histopathological examination is dermal lymphoid infiltration, which is classified as having a nodular or diffuse pattern. This infiltrate is composed of small lymphocytes, marginal zone B cells, lymphoplasmacytic cells, and plasma cells. Marginal zone B cells are surrounded by small to medium-sized cells with irregular and inconspicuous nuclei and a large amount of pale cytoplasm. On periodic acid-Schiff staining, intranuclear or intracytoplasmic inclusions can be observed, along with a predominance of lymphoplasmacytic cells [
1,
6]. A low proliferation index on Ki-67 immunohistochemical staining is another characteristic of marginal zone B-cell lymphoma [
12].
PET-CT is recommended to check the degree of invasion and existence of metastasis to adjacent or distant areas [
1]. In patients with PCMZL, elevated serum beta-2-microglobulin and LDH levels are sometimes observed [
2]. Our patient did not show abnormally high levels of beta-2-microglobulin and LDH, but lymphoid aggregations with multifocal granulomas were observed in the histopathological examination.
For single or multiple localized lesions, surgical excision or radiotherapy is the treatment of choice [
13]. Immunochemotherapy using interferon-gamma or rituximab can also be considered [
13,
14]. In the present case, all skin lesions were completely removed by surgery, and postoperative PET-CT showed no lymphoid involvement. Serum markers such as beta-2-microglobulin and LDH were also normal. Therefore, the patient is being observed without radiotherapy and immunochemotherapy.
Skin lesion recurrence occurs in approximately 50% of patients with PCMZL, but extracutaneous spread is extremely rare [
1]. The diagnosis and treatment of recurrent cases follow the sample principles as used in primary cases. Agnihotri et al. [
5] and Dumont et al. [
9] recommended complete excision for solitary lesions, but did not precisely state the safety margin. In this case, wide excision of the tumor was performed, with a safety margin of 3ŌĆō5 mm, to prevent recurrence and simultaneously allow the defect to be closed with a local flap. It is possible that excision with a wider safety margin can more efficiently prevent recurrence rather than simple complete excision. This hypothesis, however, needs to be verified through subsequent large-scale studies.
Although PCMZL is relatively infrequent in Asian patients and in the facial region, it must be included in the differential diagnosis of a facial mass with atypical and rapid progression. If cutaneous lymphoma is suspected, it is important to select an appropriate treatment method by testing for an infectious etiology and promptly performing an excisional biopsy to determine the cause of the lesion.