INTRODUCTION
Many individuals suffer from accidents and facial trauma, resulting in fractures and post-traumatic facial deformities. Enophthalmos is defined as a discrepancy between the orbital contents and volume [
1]. Typically, posterior and inferior (hypoglobus) displacement of the eye is observed, resulting in functional and esthetic consequences. Functionally, global malposition can lead to a restriction of ocular movement and diplopia [
2–
4]. Esthetically, asymmetry of the globes is highly conspicuous, since the periorbital area is one of the first regions noticed during social interaction [
5].
In many cases, however, enophthalmos is diagnosed late and adequate treatment is not provided. Surgical treatment is difficult due to uncontrolled tissue responses within the orbit. In addition, the timing of reconstruction, technique, type of implant, and indications remain controversial [
6–
8]. These issues are encountered even more frequently in cases of late presentation. We accordingly present three cases of late correction of post-traumatic enophthalmos and hypoglobus with three-dimensional (3D) implants. One case was treated with an absorbable implant, and two were treated with non-absorbable implants, resulting in high patient satisfaction.
The absorbable implant (T&R PSI; T&R Biofab, Siheung, Korea) is made of polycaprolactone, which is Food and Drug Administration approved and has been used in various areas. The non-absorbable implant (Easymade CF; CGBio, Seoul, Korea) is made of a combination of polycaprolactone and BGS-7 (bioactive glass ceramic) and has also received Food and Drug Administration approval in 2021. BGS-7 forms a hydroxyapatite layer during transplantation and has the property of quickly integrating with the bone. Due to these characteristics, it has been widely used as an implant for spinal fusion since the mid-2010s, and has been recently used as an implant for facial bone defects.
To convert the computed tomography (CT) data into 3D data, AVIEW Modeler (Coreline Soft, Seoul, South Korea) was used to check the defect area. Then, Geomagic Freeform Plus (3D systems, Rock Hill, SC, USA) was used to design the implant by mirroring the normal shape and volume of the opposite orbital structures. Subsequently, using Simplify 3D (Simplify3D Software, Cincinnati, OH, USA), a slicing file was created for the final manufacture.
For the size and thickness of the implant, first, a volume-centered design was created to determine the extent of reconstruction needed, by mirroring the opposite normal side. Additional corrections were then made in accordance with each patient’s needs.
CASE REPORT
Case 1
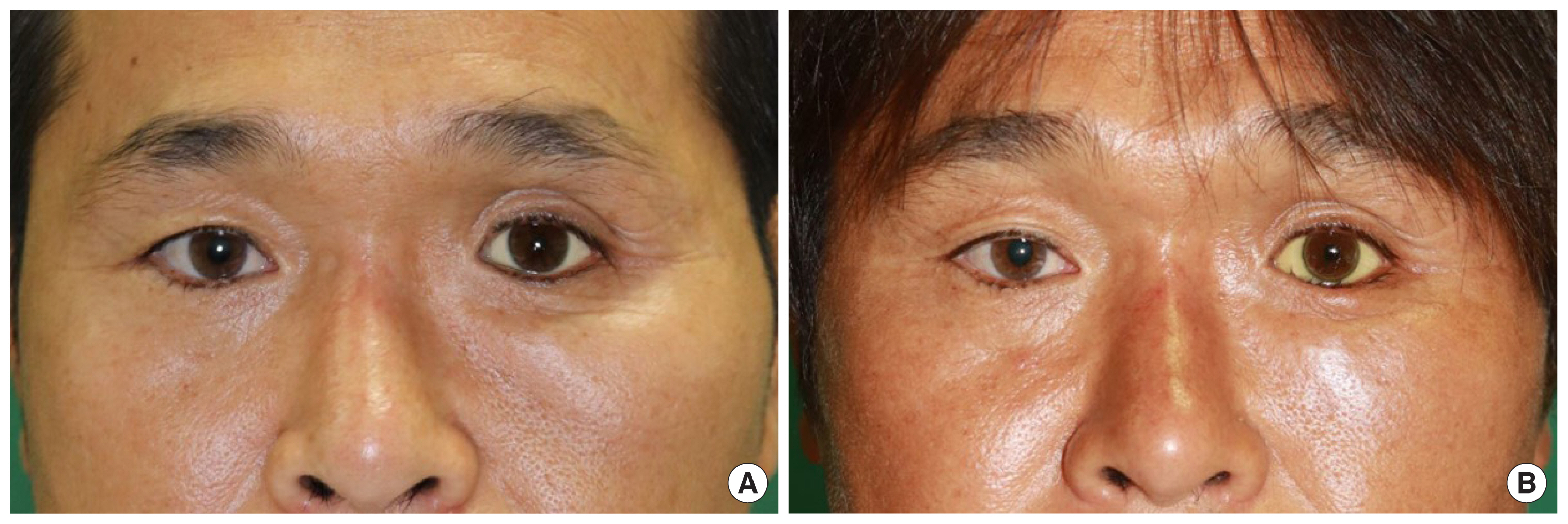
A 43-year-old male experienced a traffic accident, resulting in a Lefort I fracture and fracture of the left zygomaticomaxillary complex and coronoid process of the mandible. An open reduction with internal fixation and orbital floor reconstruction was performed a week after the accident. Two years and four months later, the patient visited our outpatient department for correction of enophthalmos. He had undergone left eye enucleation due to an eyeball rupture from the accident and had a prosthetic eye. Esthetic concern was the main purpose of this visit. The patient did not undergo exophthalmometry because of the prosthetic eye, and CT showed a 1 mm difference in the height of the globes.
An absorbable polycaprolactone 3D implant was manufactured and inserted into the subperiosteal plane on the infraorbital rim through a subciliary incision and fixed with screws. The patient was discharged within 6 days. Surgery was performed 2 years and 8 months after the accident. The difference in the height of the globes improved to near zero. There were no complications and the patient was satisfied with the results 9 months after the surgery. However, 1 year and 9 months after the surgery, the patient complained of worsening esthetic results (
Fig. 1).
Case 2
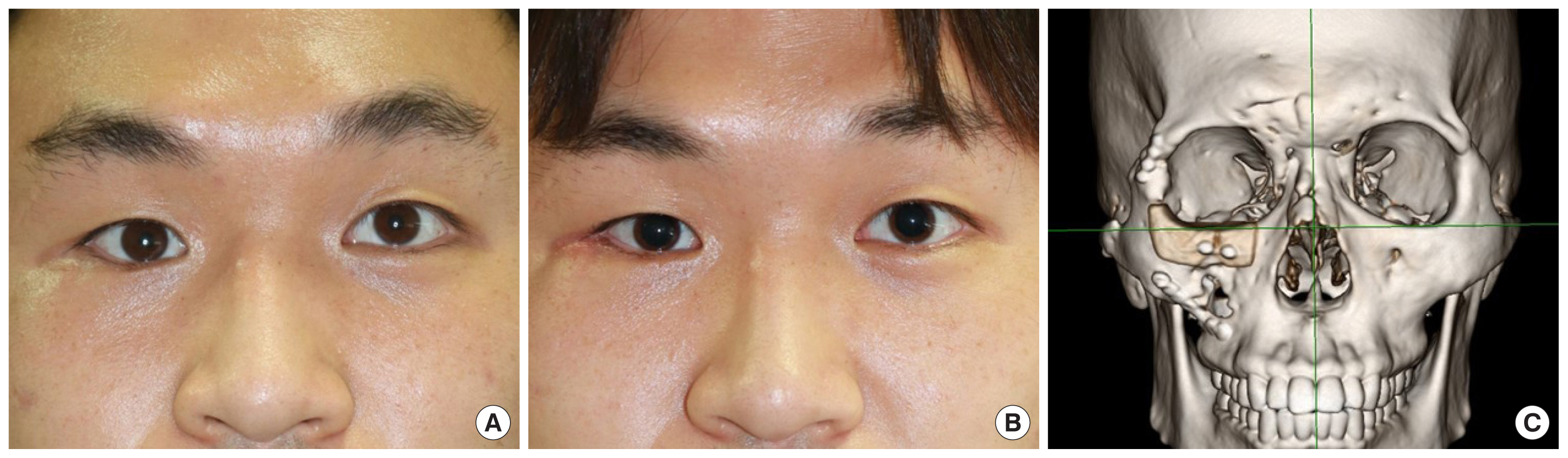
A 21-year-old male experienced a fall accident, resulting in a fracture involving the anterior table of the frontal sinus, right medial orbital wall, zygomaticomaxillary complex, and nasal bone. Open reduction with internal fixation and medial wall reconstruction with an absorbable mesh was performed 8 days after the accident. Five months later, the patient visited our outpatient department with severe enophthalmos on the right side but did not require additional surgery. The patient revisited our hospital with the same complaint 3 years later. The preoperative difference in the exophthalmometry values was 4 mm, the CT showed a 4 mm difference in the height of the globes, and the patient showed no signs of diplopia.
A non-absorbable bioceramic and polycaprolactone 3D implant was manufactured and inserted into the infraorbital rim through a subciliary incision, and the patient was discharged after 5 days. The surgery was performed 3 years and 1 month after the accident. Six months after the surgery, the difference in the exophthalmometry values had improved to 3 mm, the difference in the height of the globes improved to 2 mm, and the patient exhibited no postoperative diplopia. 3D CT showed improved symmetry of the infraorbital rim contour and the difference in height had decreased from 2 mm to nearly 0 mm. The implant was well maintained. There were no complications, and the patient was satisfied with the esthetic results (
Fig. 2).
Case 3
A 37-year-old male experienced a traffic accident, resulting in a Lefort II fracture and fracture of the right orbital floor and nasal bone. Open reduction with internal fixation was performed at another hospital. The patient visited our outpatient department 3 years after the accident. He exhibited enophthalmos on the right side, with a difference of 5 mm in the preoperative exophthalmometry values. CT showed a 3 mm difference in the height of the globes.
A non-absorbable bioceramic and polycaprolactone 3D implant was manufactured and inserted into the infraorbital rim through a subciliary incision and the patient was discharged after 4 days. Surgery was performed 4 years and 4 months after the accident. Six months after the surgery, the difference in the exophthalmometry values improved to 4 mm and the difference in the height of the globes had improved to 2 mm. There were no major complications, but medial epicanthoplasty was needed after 3 months due to scarring. The patient was satisfied with the esthetic results (
Fig. 3).
DISCUSSION
In the case of facial bone fractures, surgery within 2 weeks of the injury is generally expected to provide acceptable results [
9]. However, enophthalmos and hypoglobus are common sequelae even after surgery, especially among those with medial orbital wall and orbital floor fractures. Even after bone reduction and reconstructive surgery, these patients may experience functional or esthetic deformities, leading to stress in daily life.
Several techniques have been used to address these problems. The basic approach involves restoration of the orbital rim anatomy through osteotomy and repositioning. In cases of extensive displacement, autogenous or onlay grafting can also be performed [
10]. Zhang et al. [
11] suggested using a CT-based anatomic titanium mesh that resulted in a 65% increase in the orbital volume and a 50% correction of severe late enophthalmos. Nishi et al. [
12] used a sliced costal cartilage chip graft in a step-like configuration from a location posterior to the equatorial plane of the eyeball to the subperiosteum, in five cases, with esthetically satisfactory results. Choi et al. [
13] used an anatomically absorbable implant with iliac bone grafting. They demonstrated a decrease in the difference in exophthalmometry values from 4 mm to 1.71 mm and a 16.24% decrease in the rate of orbital volume on the injured side, compared to the normal side.
In the present cases, the timing of the surgery was approximately 2 to 4 years after the accidents and none of the patients had exhibited functional problems preoperatively. Their chief complaints were esthetic concerns due to enophthalmos and hypoglobus. Existing absorbable plate or bone graft techniques are limited by difficulties with the implementation of accurate patient-specific shapes. On the other hand, patient-customized 3D printing produces shapes that match the required anatomical shapes, thereby shortening the operation time, making it convenient, producing more satisfactory results, and improving the esthetic satisfaction of the patient. Therefore, inferior orbital rim reconstruction and soft tissue augmentation were planned using 3D implants. Absorbable implants are widely used for orbital wall fractures and have shown satisfactory results [
14]. They have also shown good results when compared with those of titanium plates [
15]. Thus, a correction with an absorbable mesh was planned initially.
In the first case, a completely absorbable polycaprolactone implant was used. There was improvement at first, but the patient complained of worsening esthetic outcomes at 1 year and 9 months after surgery. Since polycaprolactone biodegrades in 2 to 3 years, its absorption might have resulted in the worsening of the esthetic outcome, and the CT scan taken 2 years after the surgery confirmed that the implant had been absorbed into a small ingrowth of the surrounding tissue and bone. However, it is difficult to derive conclusions from a single case and further research is required.
In the second and third cases, a recently developed non-absorbable implant, made from a combination of a bioceramic material and polycaprolactone, was used. After the first case, the authors decided to use a non-absorbable implant in the hope of maintaining postoperative results for a longer period of time. Although the longest follow-up period was 6 months, satisfactory results were noted and long-term results are believed to be stable. Longer follow-up periods are required for confirmation.
In cases of post-traumatic enophthalmos and hypoglobus, although functional adaptation is possible, correction of esthetics may not be achieved, even after an extended duration. Correction with 3D implants has shown satisfactory results with no complications, and non-absorbable implants are recommended over completely absorbable implants.