INTRODUCTION
The treatment of choice for orbital wall fractures includes open reduction and orbit reconstruction to restore ocular motility and prevent enophthalmos by restoring orbital anatomy and volume [
1,
2]. The author has reported an orbital wall restoration technique in which the primary orbital wall fragments were restored to their prior position using transorbital, and transantral approaches, with temporary extraorbital support maintained in the maxillary and ethmoid sinuses [
3–
5]. Using the primary bone fragments in orbital wall fractures has many advantages, such as reducing the size of orbital wall bony defects, using relatively small-sized implants, and reducing the incidence of implant reherniation with balloon extraorbital support [
3–
5]. However, in complex orbital fractures, restoration of the mid-facial buttress is required in addition to the reconstruction of the orbital wall. Complex orbital fractures are an impure type of orbital fractures because they involve the orbital walls as well as the orbital rim, maxillary and zygomatic bones. Unlike pure blow-out fractures, in complex orbital fractures, maintaining balloon support in the maxillary sinus for several days is difficult because the screw tip used to fix the mid-face buttress and sharp bony edge of the mid-facial fracture protruding into the sinus, increasing the risk of balloon rupture [
3–
5].
In 2020, the author reported a preliminary study on the surgical outcomes of 23 patients who underwent surgery using this method for complex orbital wall fractures [
5]. The balloon rupture rate could be kept as low as 13% by fixing the screw at the correct margin of the mid-face buttress, and the potential risk of balloon rupture could be avoided using several additional methods [
3–
5]. However, the previous study was a preliminary result of only 23 patients, and it was not certain that patients operated with this method would have the same results as patients with other surgical methods. Therefore, we tried to compare the surgical outcomes for complex orbital wall fractures between patients who underwent restoration with balloon support and those that did not have balloon support.
As a follow-up to a previous preliminary study, this study retrospectively reviewed the surgical results of 939 patients with facial bone fractures who underwent surgery over a 4-year period and selected 154 patients with complex orbital fractures. We compared the surgical outcomes by dividing them into groups that underwent restoration with and without balloon support. We investigated whether predictable and reliable results could be obtained by using this method.
METHODS
Participants
The medical records of 939 patients who underwent surgical reconstruction of facial bone fractures between August 2018 and August 2022 were retrospectively reviewed. Patients with nasal bone fractures (311 patients) and non-orbital fractures (208 patients) were excluded first, and then patients with simple blow orbital fractures (266 patients) were excluded. Among 154 patients with complex orbital fractures, 44 and 110 underwent reduction with and without the balloon technique. The same surgeon operated on all the patients in this study (
Fig. 1). The study was approved by the Institutional Review Board of Dankook University Hospital (IRB No., DKUH 2022-10-033-002).
Ophthalmic examination
Ophthalmic examinations of diplopia, extraocular muscle function, and enophthalmos were performed preoperatively and 6 months after surgery. The degree of enophthalmos was measured using a Naugle exophthalmometer (Good-Lite Co.). Preoperative measurements of the Naugle scales were made the day before the surgery to minimize errors due to post-traumatic swelling [
4,
5]. Postoperative measurements were performed 6 months after surgery. All patients underwent computed tomography (CT) scans preoperatively and 6 months postoperative. The orbital volume was calculated by applying integral calculus to the CT image [
2]. The orbital volume ratio (OVR) was obtained by comparing the volume of the fractured orbit with that of the uninjured orbit [
2,
6].
Surgical techniques
Surgery was performed under general anesthesia. A forced duction test of the fractured orbit was performed to evaluate the passive mobility of the globe. Open reduction of complex fractures was performed using the gingivobuccal sulcus, lateral eyebrow, and transconjunctival approaches [
5]. After reduction, screws and plates (titanium or resorbable) were used to fix the horizontal and vertical buttresses, such as the infraorbital rim, zygomaticomaxillary buttress, and nasomaxillary buttress, to obtain proper skeletal support [
5]. When fixing the plate to the mid-face buttress, the plate was placed to the margin of the buttress so that the screw tip did not touch the balloon in the maxillary sinus. Short screws with blunt tips were selected for patients scheduled to use a Foley catheter balloon for orbital restoration to prevent balloon rupture (
Figs. 2,
3).
Dissection was performed until the fractured orbital wall was exposed using the transconjunctival approach. The orbital content herniated through the fracture was repositioned back into the orbital cavity. A curved freer elevator was inserted transnasally into the maxillary ostium to raise the herniated orbital floor to the original position. When the orbital wall defect was restored with primary bone fragments, sponge-type intranasal dressing agents (PosiSep X; Hemostasis LLC) were inserted into the maxillary sinus through the ostium for balloon protection [
2,
3]. A 14-Fr or 16-Fr catheter (Sewoon Medical Co., Ltd.) was inserted into the maxillary sinus through the maxillary ostium. The Foley catheter balloon was then inflated with a saline solution mixed with a radiopaque dye (Telebrix 30; Guerbet) until the fractured orbital floor was restored to prior position [
2,
7]. The inflated Foley catheter balloon can support the orbital floor superiorly as well as the anterior wall of the maxillary sinus anteriorly. If medial blow-out fracture was combined, the prolapsed orbital contents were freed from entrapment using an orbital approach. The bone fragments of the medial wall were gently mobilized out from the ethmoidal sinuses with a straight freer elevator under direct vision using a transorbital approach [
3]. Several pieces of NasoPore (Stryker Inc.) were placed in the ethmoid sinus using a transnasal approach to support the restored medial wall [
3]. Two types of implants were used to reconstruct remaining orbital wall defect depending on the size of the defect after restoring the orbital wall to its original position. In cases where the remaining defect was small, 85:15 polylactide/polyglycolide polymer (Rapidsorb; Synthes Inc.) was placed on the fracture site to bridge the defect [
8]. However, if the remaining orbital wall defect was large, it was reconstructed using a porous polyethylene (Synpor; Synthes Inc.) implant.
A forced duction test was performed to ensure the free movement of the globe. The balloon support was maintained for 7 days after surgery [
1,
2]. NasoPore (Stryker Inc.) packing, inserted to support the medial wall, was maintained, and spontaneously absorbed after several weeks. All surgical procedures were the same in the control group, except for the balloon insertion, foam insertion to the maxillary sinus, and fixation of the plate to the margin of the buttress.
Statistical analysis
The t-test was used to analyze the difference between OVR and the Naugle scale preoperatively and 6 months postoperatively in each group. SPSS version 20.0 Windows (IBM Corp.) was used for all the statistical analyses. Statistical significance was set at p<0.05.
RESULTS
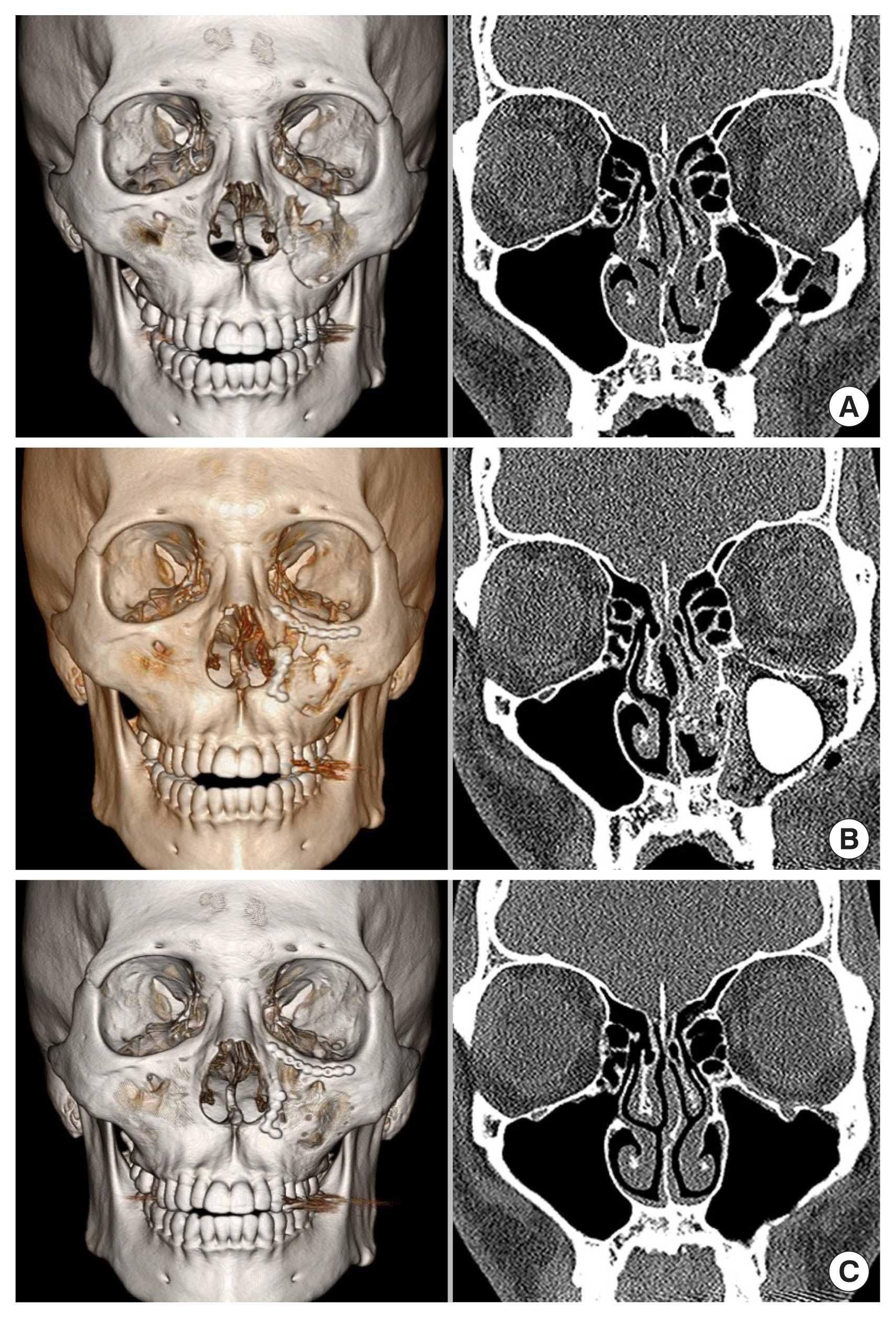
Of 939 total patients with facial bone fractures that underwent surgery during a 4-year period, we excluded patients with nasal bone fractures (311 patients), non-orbital fractures (208 patients), and pure blow-out fractures (266 patients). Of the remaining 154 patients with complex orbital wall fractures, 44 underwent orbital wall restoration using the balloon technique, and 110 patients underwent restoration without the balloon technique. The most common type of complex fracture was zygomaticomaxillary (27 cases), followed by nasomaxillary (8 cases), maxillary fractures (8 cases), and LeFort fractures (1 case) (
Table 1,
Figs. 4,
–
6). Among 110 patients treated without the balloon technique, 87 cases were zygomaticomaxillary complex fractures, 11 cases were nasomaxillary fractures, seven cases were maxillary fracture, and five cases were LeFort fractures. All patients had a follow-up period of at least 6 months.
The preoperative OVR of the balloon restoration group was 105.61, which was higher than the 103.04 of the control group. The OVR decreased by 3.32% and 2.39% in the group with and without balloon restoration and the difference in OVR in each group was significant in both groups, but the difference in OVR was greater in patients in the balloon restoration group compared with the control group significantly. Naugle scale did not differ significantly in each group (
Table 2).
The total complication rate was 22.7% (
Table 3). Complications among 44 patients using Foley were as follows: first, Foley balloon rupture was confirmed in six patients. Of these, five patients used a metal plate, and one patient used a resorbable plate. And four patients did not use protection with resorbable intranasal dressing agents (PosiSep X; Hemostasis LLC). The balloon rupture occurred 3 to 5 days after surgery in all six cases. Second, three patients experienced transient soft tissue infections that occurred within 1 month after surgery. The patients revisited the hospital with cheek or periorbital swelling. All patients were treated with intravenous antibiotics alone, and the infection resolved within a few days. One patient experienced both balloon rupture and infection. Third, malposition also occurred in two cases, where the balloon prolapsed into the posterolateral side of the maxillary sinus due to a fracture of the post wall of the maxillary sinus and was managed by direct removal of the inserted catheter. Postoperative balloon rupture occurred in six out of 44 cases (13.64%), similar to the three of 23 cases (13%) rupture rate in the paper published in 2020 [
5]. In a previous study, balloon rupture occurred on the first day after surgery in one case; however, balloon rupture occurred in all six cases 3 to 5 days after surgery. For patients with rupture, a ruptured catheter was held in place for postoperative day 7 and then removed. None of the six patients showed significant enophthalmos at 6 months of follow-ups.
DISCUSSION
The authors previously reported an orbital wall restoration technique that restored the orbital floor to its prior position. This restoration technique significantly decreased the extent of orbital wall bone defects and increased bony continuity due to the anatomical restoration of the primary orbital wall because the fractured fragments were restored to their prior position [
1,
2]. In addition, temporary extraorbital support could reduce the postoperative displacement of the orbital implant, and the orbital wall fragments could heal in their primary position, reducing the risk of orbital volume change [
1,
7].
Pure orbital floor fractures had a low rupture rate when the balloon was inserted into the maxillary sinus to support the inferior orbital wall restored to its original position. The orbital wall restoration technique has many advantages; however, applying this method to complex orbital wall fractures takes a lot of work. Patients with complex orbital wall fractures require restoration of the displaced orbital wall as well as reconstruction of the adjacent mid-face buttresses, which is technically demanding [
5,
9]. Maintaining the balloon in place for several days after surgery is difficult because the sharp screw tip used for buttress fixation and the bony edge of the mid-face fracture increases the risk of balloon rupture in complex orbital fractures. The author obtained stable results and reported orbital wall restoration surgery using balloon extraorbital support for the maxillary sinus in pure inferior and large inferior medial blow-out fractures in 2015 [
3,
7]. However, reliable surgical results could not be obtained using this method due to balloon rupture in complex orbital fractures. Additional ways to prevent balloon rupture were required for successful outcomes.
First, balloon rupture was prevented by fixing the screw at the margin of the mid-facial buttress. The maxillary sinus is pyramidal and comprises four walls: anterior, posterior, superior (inferior orbital wall), and mid-facial buttresses located at the edge of the pyramidal-shaped maxillary sinus [
10]. Suppose the screws are fixed at the correct margin of the maxillary sinus. In that case, there might be a space between the tip of the screw and the balloon, preventing the balloon from touching the screw (
Fig. 3) [
5]. Second, short (4 mm) blunt-tip screws were used to fix the mid-facial buttress to protect the balloon from touching the screw (
Figs. 2,
3). Third, the sharp bone edge of the mid-facial fracture fragments and surgical instruments could have caused balloon rupture. This risk could be reduced by inserting sponge-type resorbable intranasal dressing agents (PosiSep X; Hemostasis LLC) into the sinus before balloon insertion (
Fig. 3) and made the operation easier. In addition, an average of 12 to 15 cc of radiopaque dye had to be injected into the balloon to restore the orbital floor; however, when the maxillary sinus was prefilled with this dressing agent, the floor was restored with a small amount (6–9 cc) of saline injection, which was effective in preventing balloon rupture.
The balloon rupture rate could be kept as low as 13.64% (6/44 cases) with marginal screw fixation, 4 mm blunt tip screws, and extra sponge protection, which is similar to the 13% (3/23 cases) rupture rate in a paper published in 2020 [
5]. All six cases of balloon rupture occurred 3 to 5 days after surgery, and they did not show orbital floor depression at the 6-month CT follow-up or significant enophthalmos on exophthalmometry. In this study, the Naugle scale decreased by 0.07 after surgery in balloon using group, but it did not show statistically significant difference and was considered to be an error due to preoperative periorbital swelling.
The preoperative OVR of the balloon restoration group was higher than that of the control group. This means that the orbital fractures were larger and more severe in patients in the balloon restoration group. Postoperatively, the difference in OVR in each group was significant in both groups, but the difference in OVR was greater in patients in the balloon restoration group compared with the control group, meaning that the orbital volume recovery was higher in patients in the balloon restoration group.
Transient soft tissue infection occurred in three patients, with all three patients visiting the hospital with cheek or periorbital swelling within 1 month after surgery. After hospitalization, they were treated with intravenous antibiotics and recovered within a few days. In general, there is no risk of balloon malposition when the balloon is placed in the maxillary sinus through the maxillary ostium in a pure orbital wall fracture. However, if the posterior wall of the maxillary sinus is fractured in a complex orbital fracture, the balloon may escape through the fractured outer wall, resulting in malposition. In this study, the balloon was misplaced posterolaterally of the maxillary sinus and was removed during surgery in two patients. Therefore, the position of the balloon must be checked with a portable X-ray in patients with complex orbital fractures.