Relationship between midfacial fractures and maxillary sinus pathology
Article information
Abstract
Background
Midfacial fractures frequently involve the maxillary sinus, leading to maxillary sinus pathology. We aimed to examine the incidence and contributing factors of maxillary sinus pathology in patients who underwent open reduction and internal fixation (ORIF) for midfacial fractures.
Methods
A retrospective analysis was conducted on patients who underwent ORIF for midfacial fractures at our department over the past 10 years. The incidence of maxillary sinus pathology was identified clinically and/or by computed tomography findings. Factors that significantly influenced the groups with and without maxillary sinus pathology were examined.
Results
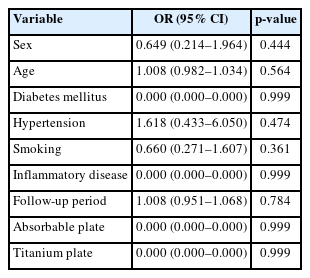
The incidence of maxillary sinus pathology in patients who underwent ORIF for midfacial fractures was found to be 11.27%, with sinusitis being the most common pathology. Maxillary sinus pathology was significantly associated with the presence of a blowout fracture involving both the medial and the inferior orbital walls. Factors such as sex, age, diabetes mellitus, hypertension, smoking, inflammatory disease, follow-up period, use of absorbable plates, and use of titanium plates did not have a significant impact on the development of maxillary sinus pathology.
Conclusion
The incidence of maxillary sinus pathology in patients who underwent ORIF for midfacial fractures was relatively low, and in most cases, it resolved without the need for specific treatment. Consequently, there may not be a significant need for concern regarding postoperative maxillary sinus pathology.
INTRODUCTION
Midfacial fractures account for 45.4% to 79.1% of all facial fractures and often involve the maxillary sinus [1]. These fractures can be caused by motor vehicle accidents, domestic disputes, falls, industrial accidents, or assaults with or without a weapon [1-5]. When a midfacial fracture is accompanied by a maxillary sinus fracture, potential complications may include orbital muscle entrapment, orbital cellulitis, orbital abscess, enophthalmos, hypophthalmos, sinusitis, sinus mucocele, pseudoaneurysm, oromaxillary fistula, dental malocclusion, epistaxis, facial asymmetry, chronic facial pain, pressure sensitivity, and infraorbital nerve paresthesia [2,3,6,7].
Sinusitis is the most common disease affecting the maxillary sinus after trauma [1]. In the majority of midfacial fracture cases, disruption of the mucosa lining the internal wall of the sinuses occurs, increasing the risk of various problematic sequelae. Nonetheless, the maxillary sinus mucosa exhibits a substantial ability to regenerate, although this potential for regeneration may not suffice, if a large defect occurs [3]. The development of maxillary sinusitis might be influenced by the disruption of sinus integrity and blood in the sinuses [4].
Numerous studies have been conducted on post-traumatic maxillary sinusitis. However, research on maxillary sinus pathology following open reduction and internal fixation (ORIF) in patients with midfacial fractures is scarce. Although Jiang et al. [1] identified risk factors for maxillary sinus pathology after surgery for a midfacial fracture, their study was limited to patients using titanium plates and focused on maxillary sinus involvement rather than the fracture type. Similarly, Ballon et al. [3] compared outcomes of anterior maxillary sinus wall reconstruction, but their study was also restricted to patients using titanium plates and concentrated on maxillary sinus involvement in the anterior wall. In this study, our objective was to examine the incidence rate and contributing factors of maxillary sinus pathology in patients who underwent ORIF for midfacial fractures with absorbable plates or titanium plates.
METHODS
Study design and patients
We conducted a retrospective review of patients who underwent ORIF for midfacial fractures at our department between 2012 and 2022. In total, 1,416 patients underwent ORIF for midfacial fractures. Patients with pre-existing maxillary sinus pathology, dental lesions, indeterminable maxillary sinus pathology due to severe blood retention on postoperative computed tomography (CT), or CT follow-up less than 2 months after surgery were excluded. After applying these exclusion criteria, 275 patients who underwent ORIF for midfacial fractures were included in this study. We reviewed the patients’ medical records, which included information on age, sex, underlying disease, fracture sites, follow-up period, and fixation materials (absorbable plate or titanium plate). Maxillary sinus pathology was determined by comparing the patients’ clinical symptoms and preoperative and postoperative CT scans, with a consensus reached by one radiologist and two plastic surgeons. Maxillary sinus pathology was classified into sinusitis, mucosal thickening, and retention cysts. Mucosal thickening was defined as a mucosal thickness of 2 mm or more. Maxillary sinusitis was considered to be present when severe mucosal thickening was observed on a CT scan and opacification of the entire maxillary sinus wall or air-fluid level was observed.
Surgical method and postoperative care
For patients with maxillary fractures or zygomaticomaxillary complex (ZMC) fractures, an incision was made along the upper gingivobuccal sulcus to access the fractured bone. Additional subciliary and lateral eyebrow incisions were performed when necessary. After reducing the fractured bone, reconstruction was carried out using either an absorbable plate or a titanium plate. Silicone Barovac drainage (Sewoon Medical Co., Ltd.) was employed to remove blood or fluid accumulation at the surgical site. The tip of the Barovac drain was placed in front of the anterior wall of the maxillary sinus. The Barovac drainage was removed when the volume of fluid drained through it was 10 cc or less, and this occurred within 3 days for all patients. All patients received postoperative antibiotics (Flomoxef sodium 1 g every 12 hours) for a duration of 2 days. For patients with blowout fractures of the medial and/or the inferior orbital wall, reconstruction was performed using an absorbable mesh plate after reduction through a transcaruncular incision and a subciliary incision, respectively. For patients with frontal bone fractures, reduction was achieved through a transcutaneous transfrontal approach [5], or fixation was performed using either an absorbable plate or a titanium plate when necessary.
Statistical analysis
Continuous variables were expressed as means with standard deviations. Categorical variables were represented by frequencies and percentages. To compare the two groups, the independent sample t-test was employed for continuous variables, while the chi-square test and the Fisher exact test were utilized for categorical variables. Logistic regression analysis was carried out to identify factors affecting the incidence of complications. A p-value of < 0.05 was deemed statistically significant. All statistical analyses were conducted using SPSS version 27.0 (IBM Corp).
RESULTS
Patients’ demographics
A total of 275 patients were divided into two groups based on the presence of postoperative maxillary sinus pathology (Table 1). Group A consisted of 244 patients without maxillary sinus pathology who underwent ORIF for midfacial fractures, while group B included 31 patients with maxillary sinus pathology. In group A, there were 196 men (80.3%) and 48 women (19.7%), and in group B, there were 26 men (83.9%) and five women (16.1%); the sex distribution between groups A and B was not statistically significant (p = 0.638). The mean age of patients was 36.19 years in group A and 38.48 years in group B, with no statistical difference between the groups (p = 0.498). The follow-up period in group A (8.93 months) was not significantly different from the follow-up period in group B (9.00 months) (p = 0.954). Groups A and B also did not show significant differences in terms of the proportion of patients with hypertension, diabetes mellitus, smoking, or inflammatory disease. The accompanying fracture sites were the frontal bone (9 cases), medial orbital wall (62 cases), inferior orbital wall (95 cases), maxilla (52 cases), and ZMC (116 cases) in group A, and the medial orbital wall (9 cases), inferior orbital wall (16 cases), maxilla (6 cases), and ZMC (14 cases) in group B. There were no significant differences in the accompanying fracture sites between groups A and B. In this context, maxillary fracture refers to a fracture confined to the maxilla, specifically the anterior wall of the maxillary sinus, and ZMC fracture refers to a maxillary fracture accompanied by a zygomatic complex fracture. In group A, absorbable plates and titanium plates were used for 231 and 16 patients, respectively. In group B, absorbable plates and titanium plates were used for 29 and two patients, respectively. No significant difference was found between the two groups regarding the plates used.
Distribution of maxillary sinus pathology
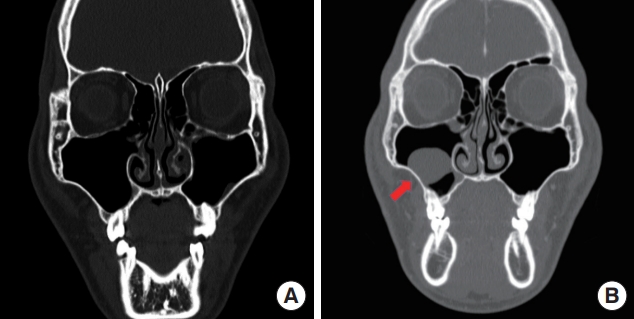
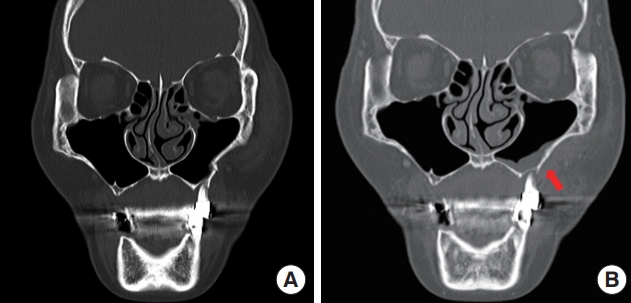
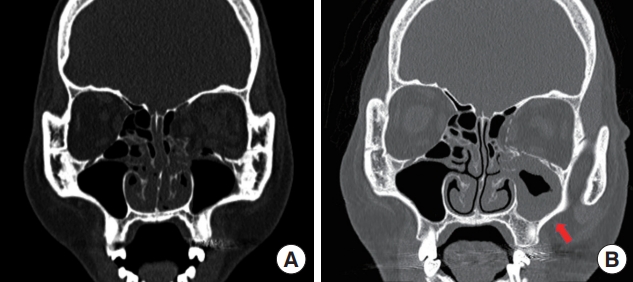
Sinus pathology was categorized into sinus mucosal thickening, sinusitis, and retention cysts (Fig. 1). The most common type was maxillary sinusitis (21 cases, 66.74%), followed by retention cysts (7 cases, 22.58%) and mucosal thickening (3 cases, 9.67%) (Figs. 2-4).

Maxillary sinus pathology classification with the number of cases and their percentage in parentheses.
A 66-year-old woman with a left zygomaticomaxillary complex fracture. (A) Preoperative coronal facial computed tomography. (B) Coronal computed tomography 5 months after surgery revealing mucosal thickening after open reduction and internal fixation with absorbable plates and screws (red arrow).
A 48-year-old woman with a left blowout fracture of both the medial and the inferior orbital walls. (A) Preoperative coronal computed tomography. (B) Coronal computed tomography 18 months after surgery revealing maxillary sinusitis after reconstruction of both the medial and the inferior orbital walls with absorbable plates and screws (red arrow).
Distribution of maxillary sinus pathology according to fracture types
Out of 275 patients, only six patients experienced frontal bone fractures, and none of these patients developed sinus pathology. The remaining 269 patients were categorized into nine groups based on the fracture site: patients with medial orbital wall blowout fractures, inferior orbital wall blowout fractures, maxilla fractures, ZMC fractures, combined medial and inferior orbital wall blowout fractures, combined maxilla and inferior orbital wall blowout fractures, combined ZMC and inferior orbital wall blowout fractures, medial and inferior orbital wall blowout fractures accompanied by either maxilla or ZMC fracture, and medial orbital wall blowout fractures accompanied by either maxilla or ZMC fracture (Table 2).
Among the 35 patients with blowout fractures of the medial orbital wall, three developed maxillary sinusitis, while mucosal thickening and retention cysts were not observed. In the group of 27 patients with blowout fractures involving the inferior orbital wall, one patient each developed mucosal thickening, maxillary sinusitis, and retention cysts. Of the 80 patients with ZMC fractures, seven patients experienced maxillary sinusitis, one had a retention cyst, and none exhibited mucosal thickening.
In the 19 patients with blowout fractures involving both the medial and the inferior orbital walls, five developed maxillary sinusitis, but mucosal thickening and retention cysts were not observed. Among the 15 patients with combined maxilla and inferior orbital wall blowout fractures, one patient each experienced maxillary sinusitis and retention cysts, while mucosal thickening was not observed. In the group of 39 patients with combined ZMC and inferior orbital wall blowout fractures, two patients each developed mucosal thickening and maxillary sinusitis, and one had a retention cyst.
For the 12 patients with blowout fractures of the medial and the inferior orbital wall accompanied by either maxilla or ZMC fractures, one developed maxillary sinusitis, but mucosal thickening and retention cysts were not observed. Lastly, among the five patients with medial orbital wall blowout fractures accompanied by either maxilla or ZMC fractures, none experienced mucosal thickening, maxillary sinusitis, or retention cysts.
Variables related to maxillary sinus pathology
In the univariable logistic regression analysis examining the impact of fracture type, only patients with a blowout fracture that involved both the medial and the inferior orbital walls demonstrated a significant influence on the development of sinus pathology, while other types did not show a significant effect (Table 3). Multivariable logistic regression analysis was conducted to identify factors influencing sinus pathology. Sex, age, diabetes mellitus, hypertension, smoking, inflammatory disease, follow-up period, use of absorbable plates, and use of titanium plates were not found to significantly influence the occurrence of sinus pathology (Table 4).
DISCUSSION
The paranasal sinuses consist of the maxillary, ethmoid, frontal, and sphenoid sinuses. Mucociliary clearance in the paranasal sinuses serves as a primary defense mechanism for the respiratory tract, protecting against inhaled pollutants, allergens, and pathogens [8]. Among the paranasal sinuses, the maxillary sinus is the largest and the first to develop embryologically. The anterior wall of the maxillary sinus is composed of the bony maxilla. On the posterior aspect, the infratemporal surface of the maxilla forms the anterior border of the pterygopalatine fossa. The superior aspect is composed of the thin orbital floor, where the infraorbital nerve runs through the infraorbital canal. The medial border comprises the delicate bones of the lateral wall of the nasal cavity. The floor of the sinus consists of the palatine and alveolar processes of the maxillary bone, while the zygoma forms the lateral aspect. The maxillary sinus is primarily supplied with blood through branches of the maxillary artery, including the posterior lateral nasal artery, the infraorbital artery, and the posterior superior alveolar artery. The maxillary sinus and its mucosa are primarily innervated by the maxillary division of the trigeminal nerve [9]. The maxillary sinus is one of the frequently injured anatomical sites in midfacial fractures.
Numerous studies have discussed the complications of midfacial fractures, such as epiphora, anosmia, malocclusion, and diplopia. Other complications after midfacial fractures involving the maxillary sinus include loose bone in the sinus cavities, retained foreign bodies, maxillary sinus wall defects, and sinusitis. Loose bone, foreign bodies, and wall defects can be treated during primary fracture surgery, whereas maxillary sinusitis is a late complication. Therefore, it cannot be treated during initial treatment. Despite the removal of all foreign bodies and the repair of displaced sinus walls during surgery, sinusitis may still develop in the maxillary sinus following a midfacial fracture.
In the United States, the prevalence of maxillary sinusitis in the general population is 13.6% [4]. However, very few studies have reported the incidence of maxillary sinusitis in large samples of patients with maxillofacial injuries. In a study by Jiang et al. [1], maxillary sinus pathology was present in 218 of the 372 imaged maxillary sinuses (58.60%), indicating that maxillary sinus pathology was common following ORIF of a midfacial fractures. In contrast, our study revealed an 11.27% incidence of maxillary sinus pathology. This discrepancy may be due to the fact that most patients in our study underwent surgery using absorbable plates and had a longer follow-up period, unlike the study by Jiang et al. [2]. This suggests that maxillary sinus pathology may resolve over time.
In this study, we found that blowout fractures involving both the medial and the inferior orbital walls were factors that increased the occurrence of maxillary sinus pathology. Anatomically, the orbital wall is located adjacent to the nasal cavity and paranasal sinuses and is thinner and more fragile than other bones [10]. The inner wall of the orbit is adjacent to the ethmoid sinus through a thin ethmoid paper template, while the floor forms the superior aspect of the maxillary sinus. When a medial orbital wall fracture occurs, the orifices of the paranasal sinuses can be blocked by the formation of fracture fragments, deformation of the orbital bone, and preexisting-intraorbital mucocele [11]. Similarly, inferior orbital wall fractures can lead to sinus pathology. When a medial orbital wall fracture is accompanied by an inferior orbital wall fracture, several paranasal sinuses are simultaneously involved, resulting in severer mucus retention and sinus drainage obstruction than in other cases. This is believed to have a significant influence on the occurrence of sinus pathology. When a blowout fracture with involvement of both the medial and the inferior walls was accompanied by a maxilla fracture or a ZMC fracture, sinus pathology occurred in only one out of 12 cases. The low incidence may be due to the smaller number of cases.
Frontal sinusitis is a relatively common condition, affecting 15% of the adult population [12]. However, no research has reported the incidence of frontal sinusitis following frontal sinus fractures. We hypothesized that the involvement of the frontal sinus in patients with a frontal bone fracture might contribute to the development of frontal sinus pathology or other paranasal sinus pathologies; however, this was not observed in our study. The anterior wall of the frontal sinus is much stronger than the other facial bones, resisting up to 400 to 1,000 kg before fracturing. The cancellous bone between the inner and outer cortical plates of the anterior wall and the air cavity between the anterior and posterior walls of the sinus are the major determinants of this structure’s strength [13]. In this study, no patient developed frontal sinusitis after surgery for a frontal sinus fracture. This may be because the number of cases was small (9 cases), and only the patients with fractures in the anterior wall of the frontal sinus underwent surgery.
Treatment for acute sinusitis primarily focuses on managing symptoms and does not involve antibiotics unless patients complain of clinical symptoms or exhibit signs of infection. Topical nasal decongestants and saline irrigation of the nasal cavity are the main treatments used. Similarly, for chronic sinusitis, nasal irrigation and decongestants are initially employed. Chronic or recurrent acute conditions that do not respond to conventional medical therapy may necessitate surgery [8]. In a study by Schmidt et al. [14], prophylactic antibiotics for sinusitis following maxillary sinus fractures showed no significant effect. In this study, the majority of sinusitis patients were asymptomatic. When symptoms did arise, they were effectively treated with antibiotics through consultation with the otorhinolaryngology department, and patients were subsequently followed up in the outpatient department.
Retention cysts are caused by the obstruction of ducts in the seromucous glands of the sinus lining. These cysts are commonly found in the maxillary sinus and may be incidentally discovered in imaging studies for 9% to 22% of the general population [15]. Maxillary retention cysts are typically asymptomatic and do not necessitate treatment. However, they can sometimes cause headaches, facial pain near the sinus, nasal obstruction, postnasal drip, and nasal discharge. In the past, symptomatic maxillary retention cysts were completely removed through the Caldwell-Luc procedure. Endoscopic sinus surgery has recently become the preferred surgical procedure [15]. In this study, none of the patients with retention cysts reported any specific symptoms, and they are currently being monitored.
One limitation of this study was the small sample size. In our department, patients were instructed to visit the outpatient department at 1 month, 6 months, and 1 year after surgery for midfacial fractures. Although many patients adhered to the follow-up schedule up to 1 month postoperatively, some were not followed up due to a lack of specific symptoms, while others refused to undergo CT scans for personal reasons. Furthermore, the follow-up of some patients with symptomatic sinusitis was lost because they sought treatment in the otorhinolaryngology department or at other hospitals closer to their residences. A second limitation was the classification of sinus pathology. Since the classification was based on clinical symptoms and CT scans, it may be less accurate than determining sinus pathology through endoscopy. Lastly, it was challenging to accurately determine the severity of the fracture. There may be differences in incidence depending on severity, such as the presence or absence of a bony defect and the degree of misalignment, but it was difficult to establish an objective classification criterion.
In this study, the incidence of maxillary sinus pathology following surgery for midfacial fractures was only 11.27%, with all patients demonstrating improvement through conservative treatment. Consequently, when ORIF is performed in patients with midfacial fractures, there may not be a significant need for concern regarding sinus pathology.
Abbreviations
CT
computed tomography
ORIF
open reduction and internal fixation
ZMC
zygomaticomaxillary complex
Notes
Conflict of interest
Jae Ha Hwang and Kwang Seog Kim serving as editorial board members of the journal were not involved in the following: selection of the peer reviewer, evaluation of the article, and decision process of acceptance of this article. No other potential conflicts of interest relevant to this article were reported.
Funding
None.
Ethical approval
The study was approved by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUH-2023-171) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and use of their images.
Author contributions
Conceptualization: Kwang Seog Kim. Data curation: Jun Ho Choi, Dong Wan Kim, Soo Hyuk Lee. Formal analysis: Jae Ha Hwang, Sam Yong Lee. Investigation: Dong Wan Kim, Soo Hyuk Lee. Methodology: Jun Ho Choi, Sam Yong Lee. Project administration: Kwang Seog Kim. Writing - original draft: Jun Ho Choi, Dong Wan Kim, Soo Hyuk Lee. Writing - review and editing: Kwang Seog Kim.