|
 |
- Search
| Arch Craniofac Surg > Volume 24(3); 2023 > Article |
|
Abstract
White-eyed blowout fractures with extraocular muscle (EOM) entrapment necessitate emergency surgical intervention. However, even after surgery, diplopia or EOM motion limitations may persist due to the incomplete reduction of soft tissue herniation caused by inadequate dissection or unresolved muscle strangulation. In this report, we present a case of postoperative EOM movement limitation in a 5-year-old girl who experienced recurrent restriction in the upward gaze of her right eye 14 days after surgery. Instead of revision surgery, the patient was treated with targeted EOM exercises focusing on the inferior rectus muscle and inferior oblique muscle. The patient was instructed to slowly move her pupils from the central point to the upper and outer sides, then in a straight line from the central point to the lower and inner sides before returning to the center point. On the 28th postoperative day, 2 weeks after initiating the exercises, the patientŌĆÖs EOM motion fully recovered. This case highlights the effectiveness of EOM exercises as a non-surgical treatment approach for improving recurrent EOM movement limitations in the absence of soft tissue herniation following surgical management of blowout fractures in children.
Blowout fractures in pediatric patients account for approximately 3% to 45% of all pediatric facial fractures. Blowout fractures in children younger than 8 years are relatively uncommon, representing less than 10% of all pediatric blowout fractures [1,2]. Generally, childrenŌĆÖs bones are more pliable than those of adults, making them more susceptible to linear and trapdoor fractures. These fractures can lead to the entrapment of muscles and soft tissues in cases of blowout fractures [3]. In particular, if a white blowout fracture with extraocular muscle (EOM) entrapment is observed on computed tomography (CT) in a patient presenting with EOM movement limitation or diplopia, despite a normal ocular appearance, this is considered an emergency. Surgical intervention is indicated in such cases [4]. However, even with surgical treatment, diplopia or EOM movement limitations may persist due to incomplete reduction of soft tissue herniation resulting from inadequate dissection or incomplete resolution of muscle strangulation [2,3,5]. In such cases, the surgeon considers reoperation to identify and address the cause of persistent EOM motion restriction. However, caution is required regarding revision surgery in pediatric patients, primarily because the use of general anesthesia in children entails several risks, including tracheal damage due to a narrow airway, heightened vulnerability to hypoxia, and possible effects on the development of cognitive function [6]. Additionally, children are at a higher risk than adults for scar formation at the surgical site. We present a rare case of a pediatric patient with EOM movement limitation due to a white-eyed blowout fracture in the inferior orbital wall, which initially improved after emergency surgical management but recurred on the 14th postoperative day. The patient was treated with EOM exercises rather than revision surgery, resulting in complete recovery. This case highlights the potential benefits of EOM exercises in managing EOM movement limitation after blowout fractures in pediatric patients.
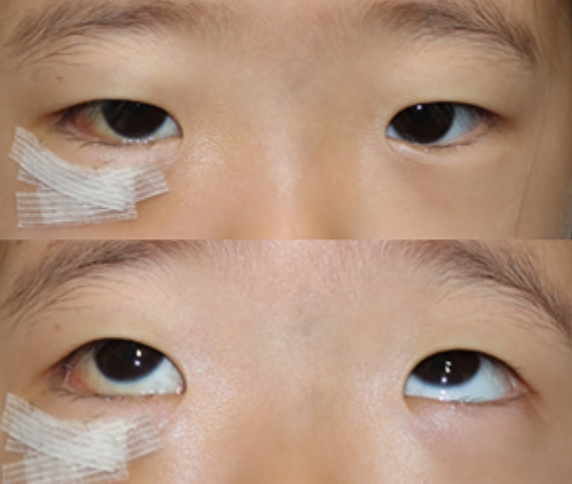
A 5-year-old girl presented with swelling in the right periorbital area due to direct trauma. The periorbital swelling was minimal, and the ocular appearance was normal. However, upon physical examination, the patient exhibited vertical diplopia and limited elevation while attempting to gaze upward. During the ophthalmic examination, visual acuity was normal, and there were no signs of enophthalmos, subconjunctival hemorrhage, hyphema, or pain during EOM motion. Symptoms suggestive of an oculocardiac reflex were absent, and sensation in the cheek area was normal. On facial CT, a trapdoor-shaped fracture measuring 7 ├Ś 7 mm was observed in the middle and posterior aspects of the right inferior orbital wall, with evidence of EOM entrapment (Fig. 1). Thus, emergency surgery was performed. Through the conjunctival approach, a fracture line starting 13 mm posteriorly from the infraorbital rim was identified, along with posterior displacement of the bone fragment. Incarceration of the EOM and soft tissue between the bone fragments was also confirmed. The entrapped muscle and herniated soft tissue were repositioned, and an 8├Ś 9 mm oval Osteomesh (Osteopore) was designed to cover the bone defect. The mesh was molded in a warm bath, inserted, and placed to fit the contour of the inferior orbital wall.
After surgery, the patientŌĆÖs EOM movement improved, and she was discharged 6 days postoperatively without any other complications (Fig. 2). However, during a follow-up outpatient visit 1 week after discharge, recurrence of limited upward gaze in the right eye was observed. Upon reexamination, the CT scan revealed that the previously herniated soft tissue had been successfully restored and its contour was maintained (Fig. 3). Therefore, the possibility of under-correction was ruled out, and we decided to treat the patient with EOM exercises rather than additional surgery.
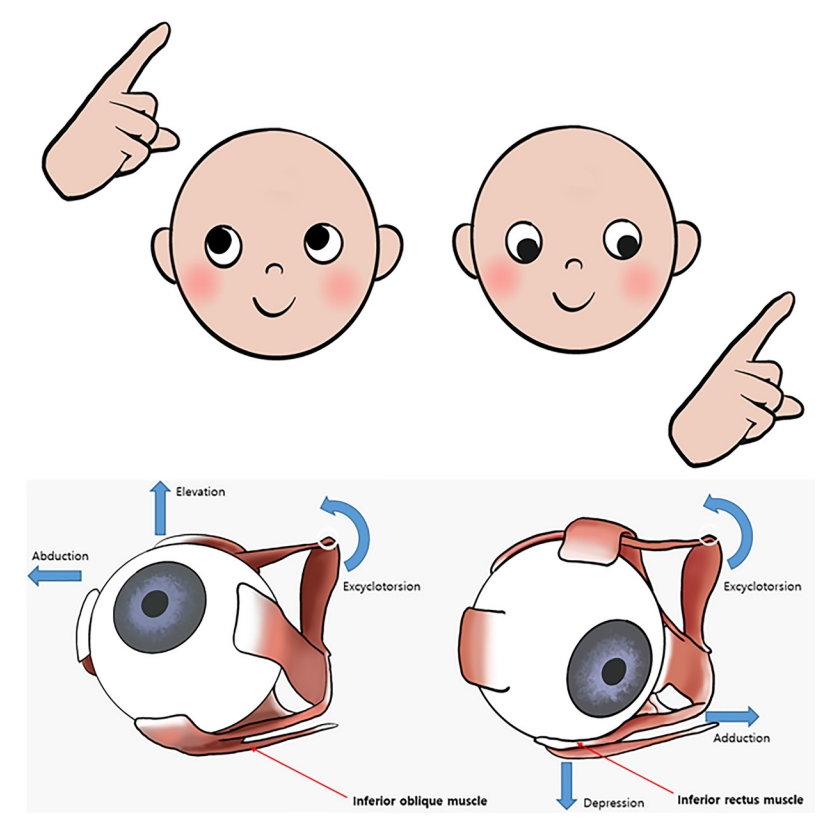
The EOMs located in the lower part of the eyeball are the inferior rectus and inferior oblique muscles. The inferior rectus is involved in depression, excyclotorsion, and adduction of the eyeball, whereas the inferior oblique is involved in excyclotorsion, elevation, and abduction.
Our EOM exercise protocol was designed to improve EOM movement limitations and reduce diplopia in pediatric patients following orbital fracture surgery. The exercise, which was performed with the right eye, involved looking from the upper lateral direction to the lower medial direction.
Given the patientŌĆÖs young age, voluntary eye movement might have been challenging; hence, the guardian assisted in inducing eye motion by placing their index finger 30 cm in front of the child. The patient was instructed to move the pupil slowly from the central point to a position 20 cm away from the upper and outer sides, and then move in a straight line from the central point to a position 20 cm away from the lower and inner sides before returning to the center point. Each pattern took approximately 10 seconds to complete and the exercise was performed at a consistent point (Fig. 4). Three sets were performed, each consisting of 100 repetitions at fixed times in the morning, noon, and evening, with one gaze in each direction. The patient also engaged in additional practice during spare moments.
Weekly outpatient clinic visits demonstrated that the EOM motion completely recovered on the 28th postoperative day, which was 2 weeks after the patient started performing the EOM exercises. Furthermore, follow-up CT showed that the previously repositioned herniated tissue and the contour of the inferior orbital wall were well maintained (Fig. 5).
Numerous reports have described blowout fractures in adult patients; however, few studies have focused on such fractures in pediatric patients, particularly in cases where the maxillary sinus is not fully developed [7]. Conservative treatment may be considered in pediatric patients with blowout fractures if no clinical symptoms are present, because the fracture site of the orbital floor can regenerate on its own [7,8]. However, if EOM entrapment causes symptoms, early exploration is necessary to prevent ischemic necrosis of the entrapped muscles, which can lead to muscle scarring and fibrotic changes [3,9]. Despite appropriate correction of soft tissue and muscle entrapment, some patients continue to experience diplopia or EOM motion restriction, with incidence rates ranging from 0% to 55% [2,3,5,10]. Research on additional procedures or rehabilitation treatments to address persistent symptoms in such cases is very limited.
In this case, although the limitation of EOM movement was resolved, the symptom recurred on the 14th day after surgery. This case differs from prior reports regarding the recurrence of EOM limitation after blowout fracture surgery. In this situation, conservative treatment was attempted due to the successful repositioning of the entrapped soft tissue, as observed on the CT scan. Consequently, EOM-specific exercises that took into account the function of the EOM muscle were conducted to address the symptoms of EOM movement limitation and diplopia.
A previous study showed that passive forced duction training and voluntary functional training for 2 weeks after surgery improved EOM motion restriction in pediatric patients. However, that study only evaluated improvement after surgery and during follow-up, and it did not present any cases that improved immediately after surgery but recurred later. Additionally, that study did not provide a detailed protocol for EOM exercises [11]. Contrastingly, we provided a detailed protocol for recurrent EOM movement limitation and demonstrated its effectiveness based on the observed results.
Prior research showed oculomotor training to be effective in preventing extraocular adhesions and alleviating postoperative diplopia in adult patients with blowout fractures who had undergone surgery [12]. However, the training method involved movements in four directions (upward, downward, left, and right), and the effectiveness of progression from 10 to 50 sets, four times per day, was compared. In contrast, our exercise method focused on specific directions (superolateral and inferomedial), targeting the inferiorly positioned inferior oblique and inferior rectus muscles in the right eye of a pediatric patient with an inferior orbital wall fracture. Since bone and soft tissue heal faster in pediatric patients than in adults, the exercise was performed with a higher number of sets.
We conducted the training with the assistance of a guardian who used their index finger to facilitate the EOM exercises. Each exercise was performed for 10 seconds, and the guardian was tasked with assisting the patient to perform the EOM exercises three times a day for 100 repetitions. Rapid recovery of symptoms was observed.
Various speculative explanations can be proposed regarding the reappearance of the EOM movement limitation 14 days post-surgery, despite its immediate improvement following the procedure. One possibility is that the entrapped EOM muscle and surrounding soft tissue experienced fibrotic changes during the healing process, resulting in restricted motion despite restoration [13]. Another potential explanation is that the absorbable plate used in the surgery may have interfered with the EOM motion.
We conclude that EOM exercise rehabilitation may be effective in pediatric blowout patients when two conditions are met: first, immediate recovery of EOM movement limitation after surgery, followed by recurrence of the limitation several days later without any traumatic event; and second, the absence of herniation recurrence according to radiologic imaging tests such as CT. Therefore, if these conditions are satisfied, favorable results can be achieved through the proposed protocol for EOM exercise rehabilitation. However, further research is necessary to investigate the effectiveness of EOM exercises by applying these results to various cases.
In conclusion, our EOM exercise regimen demonstrated favorable results in improving EOM movement limitations that recurred despite appropriate surgical repair in a pediatric patient.
Notes
Ethical approval
The study was approved by the Institutional Review Board of Soonchunhyang University Hospital (IRB No. 2023-09).
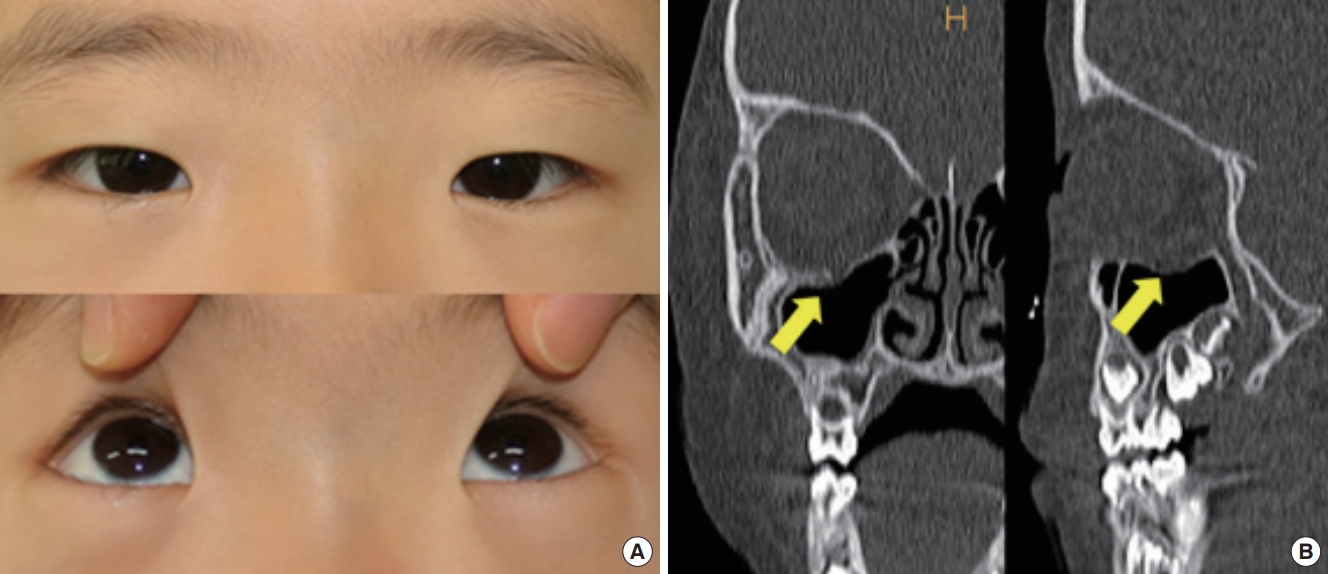
Fig.┬Ā1.
A 5-year-old girl with extraocular muscle movement limitation in the right eye. (A) Preoperative photograph showing extraocular muscle movement limitation in the right eyeŌĆÖs upper gaze and complained of diplopia. (B) Computed tomography revealed a 7├Ś7-mm fracture in the inferior orbital wall, with entrapment of the inferior rectus muscle and surrounding soft tissue (arrow).
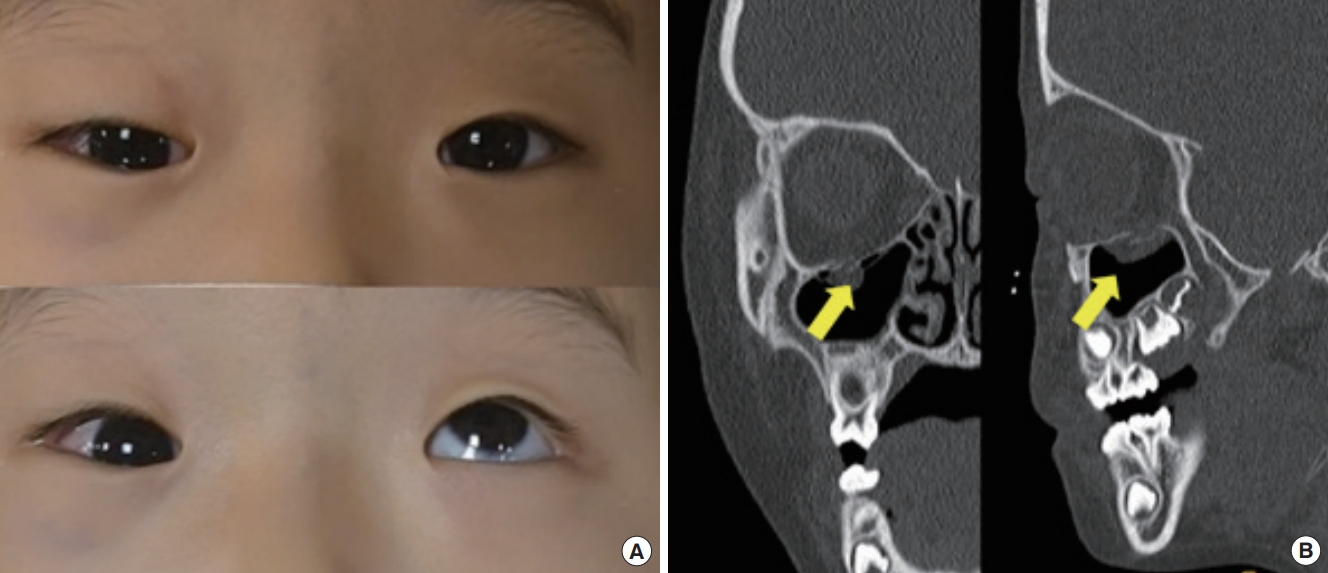
Fig.┬Ā3.
Fourteen days after surgery. (A) Photograph showing limitation in an upward gaze of the right eye. (B) Computed tomography revealed no evidence of re-entrapment of the inferior rectus musde and soft tissue (arrow).
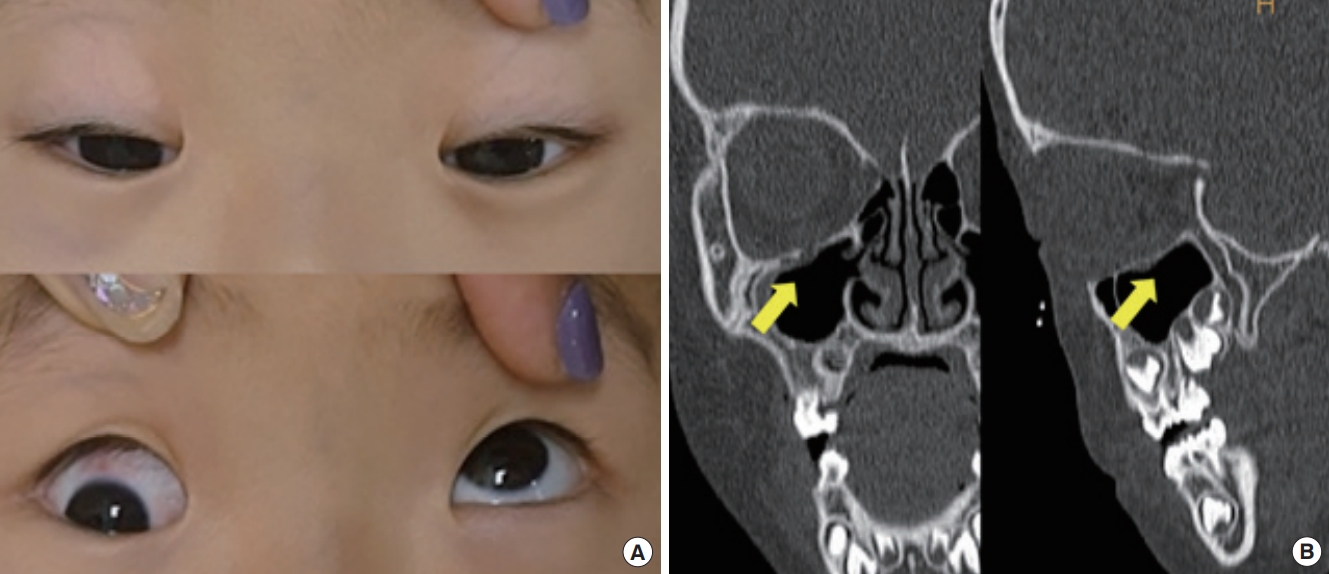
Fig.┬Ā5.
One month after surgery. (A) Photograph showing improvement in extraocular muscle movement upon an upward gaze of the right eye after consistent extraocular muscle exercise rehabilitation. (B) Computed tomography revealed no evidence of re-entrapment of the inferior rectus musde and soft tissue (arrow), as well as restored continuity through bone regeneration.
REFERENCES
1. Klenk G, Kovacs A. Blow-out fracture of the orbital floor in early childhood. J Craniofac Surg 2003;14:666-71.


2. Wang NC, Ma L, Wu SY, Yang FR, Tsai YJ. Orbital blow-out fractures in children: characterization and surgical outcome. Chang Gung Med J 2010;33:313-20.

3. Takabayashi K, Maeda Y, Kataoka N, Kagokawad H, Nagaminea M, Otad I, et al. Algorithm for pediatric orbital blowout fractures: a 20-year retrospective cohort study. Braz J Otorhinolaryngol 2023;89:447-55.



4. Hammond D, Grew N, Khan Z. The white-eyed blowout fracture in the child: beware of distractions. J Surg Case Rep 2013;2013:rjt054.



5. Lane K, Penne RB, Bilyk JR. Evaluation and management of pediatric orbital fractures in a primary care setting. Orbit 2007;26:183-91.


6. Butterworth JF, Mackey DC, Wasnick JD. Morgan & MikhailŌĆÖs clinical anesthesiology. 6th ed. McGraw Hill; 2018.
7. Sugamata A, Yoshizawa N. A case of blowout fracture of the orbital floor in early childhood. Int Med Case Rep J 2015;8:155-8.



8. Pluijmers BI, Koudstaal MJ, Paridaens D, van der Wal KG. Blowout fracture in a 3-year-old. Craniomaxillofac Trauma Reconstr 2013;6:133-6.




9. Grant JH 3rd, Patrinely JR, Weiss AH, Kierney PC, Gruss JS. Trapdoor fracture of the orbit in a pediatric population. Plast Reconstr Surg 2002;109:482-9.


10. Lee YJ. Orbital floor fracture repair with implants: a retrospective study. Arch Craniofac Surg 2021;22:177-82.




11. Li Y, Song X, Li L, Fan X, Lin M. Forced duction training: a potential key point for recovery in pediatric patients with trapdoor fracture. Medicine (Baltimore) 2016;95:e5121.


- TOOLS