Treatment of Nonsyndromic Craniosynostosis Using Multi-Split Osteotomy and Rigid Fixation with Absorbable Plates
Article information
Abstract
Background
Nonsyndromic craniosynostosis is a relatively common craniofacial anomaly and various techniques were introduced to achieve its operative goals. Authors found that by using smaller bone fragments than that used in conventional cranioplasty, sufficiently rigid bone union and effective regeneration capacity could be achieved with better postoperative outcome, only if their stable fixation was ensured.
Methods
Through bicoronal incisional approach, involved synostotic cranial bone together with its surrounding areas were removed. The resected bone flap was split into as many pieces as possible. The extent of this ‘multi-split osteotomy’ depends on the degree of dysmorphology, expectative volume increment after surgery and probable dead space caused by bony gap between bone segments. Rigid interosseous fixation was performed with variable types of absorbable plate and screw. In all cases, the pre-operational three-dimensional computed tomography (3D CT) was checked and brain CT was taken immediately after the surgery. Also about 12 months after the operation, 3D CT was checked again to see postoperative morphology improvement, bone union, regeneration and intracranial volume change.
Results
The bony gaps seen in the immediate postoperative brain CT were all improved as seen in the 3D CT after 12 months from the surgery. No small bone fragment resorption was observed. Brain volume increase was found to be made gradually, leaving no case of remaining epidural dead space.
Conclusion
We conclude that it is meaningful in presenting a new possibility to be applied to not only nonsyndromic craniosynostosis but also other reconstructive cranial vault surgeries.
INTRODUCTION
Nonsyndromic craniosynostosis is a relatively common craniofacial anomaly, taking place at the ratio of 1 case out of approximately 2000 live births [1]. Generally, it involves single suture and skull characteristics vary according to the involved suture type.
The time point of its surgical correction has not been defined clearly, but given the fact that most of the craniofacial growth and development is completed in the first year of life along with brain doubling in size while tripling in size in the second year of life, respectively [2], many experts view it would be favorable to perform operation around the age of one to achieve operation goals [3].
The surgical goals of craniosynostosis operation are to release sutural fusion sufficiently, minimize osteotomy gap, fix bone fragment rigidly to induce normal brain development without intracranial pressure increase and gain esthetically acceptable cranial vault contour. To realize surgical goals, an operational method should be determined in consideration of the number of involved sutures, dysmorphology level, and a patient's age-related bone regeneration capacity.
Generally in the cases of passing 12 months of life or showing a severe deformity, bicoronal incision is conducted for open cranial vault remodeling. The process includes synostotic bone removal, asymmetric bone osteotomize, and later on, bone fragment reshaping, replacing and fixation [4]. And in this process, due to the concern over a possible postoperative bone resorption, the size of bone fragment is usually made as big as possible and fixed by various materials.
The authors of this study found that by using bone fragments smaller than the osteotomized fragments normally used in cranioplasty, sufficiently rigid bone union and effective regeneration capacity could be made in patients aged around 24 months in cranial vault remodeling, only if their stable fixation was ensured.
Inspired by this, the authors examined nonsyndromic craniosynostosis patients with a view to achieve sufficient intracranial volume expansion and excellent esthetic cranial vault contour. To this end, we performed more osteotomies, made bone fragments smaller, and fixed them to multi-point by using diverse types of absorbable plate and screws. Then, the authors sought to identify postoperative complications including the actual bone resorption levels via a follow-up study to test the performance and safety of the operational method examined in this study.
METHODS
Patients
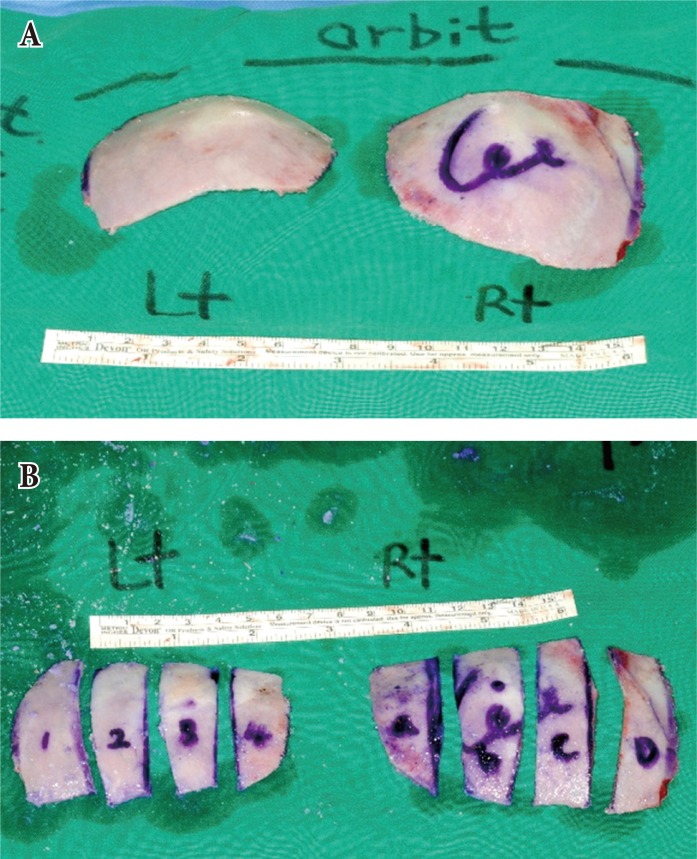
Of the entire patients receiving a cranial vault remodeling surgery for nonsyndromic craniosynostosis from July, 2011 at the authors' center, we surveyed 7 cases receiving ‘multi-split osteotomy with rigid fixation’ in this research. There were 3 plagiocephaly cases, 2 trigonocephaly cases, a brachycephaly case and scaphocephaly case each. Five were male infants and 2 were female infants aged from 7 months to 72 months at the point of operation, averaging 20.3 month with the median value of 10 months (Table 1). All of them had no special family history nor there a case suspicious of increased intracranial pressure. But there was one case of developmental delay of unknown reason.
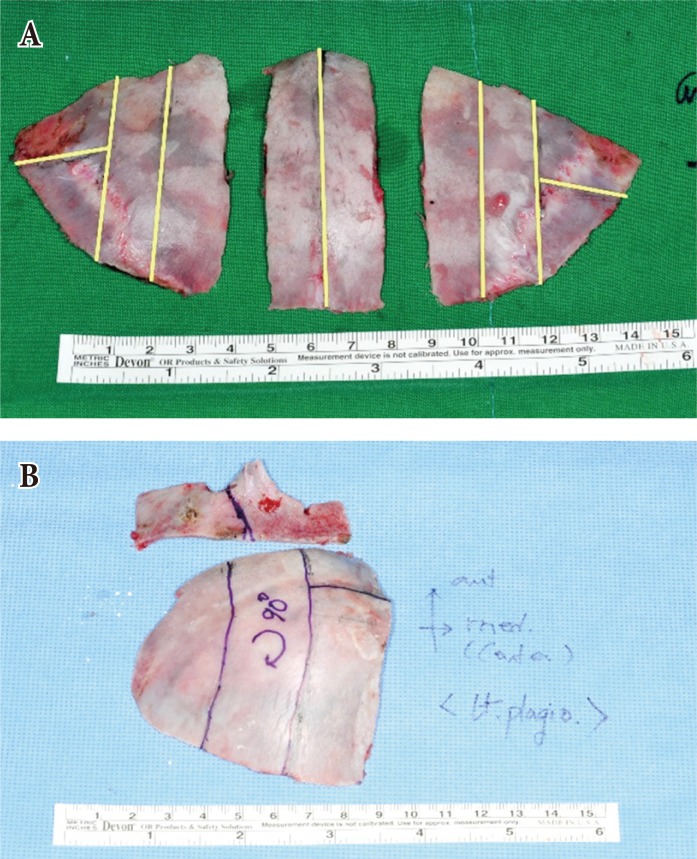
In all cases, the preoperational three-dimensional computed tomography (3D CT) was checked and brain CT was taken immediately after the surgery to see if there was any immediate postoperative complication. Also about 12 months after the operation, 3D CT was checked again to see postoperative morphology improvement, bone union and regeneration. Intracranial volume was measured in preoperative, immediate postoperative and follow-up period by multiplying the slice thickness with extent of intracranial space.
Operative technique
Under general endotracheal anesthesia, depending upon the levels of the involved synostotic suture and cranial dysmorphology, the patients were made to take an appropriate sphinx position or prone position with a headrest. With a sufficient distance from the anterior hairline, zigzag wavy coronal incision was designed ear to ear and 1% lidocaine mixed 1:200,000 epinephrine was infiltrated along the design. Incision was made with scalpel and dissection in subgaleal layer was performed with needle tip monopolar electrocautery. Raney clip was used to ensure appropriate hemostasis.
The involve suture area and its surrounding areas were sufficiently exposed then, elevated carefully not to damage pericranium. Here, we made sure not to overlap the direction and location of skin incision with those of pericranial flap incision to prevent potential deep tissue infection from skin incision as much as possible.
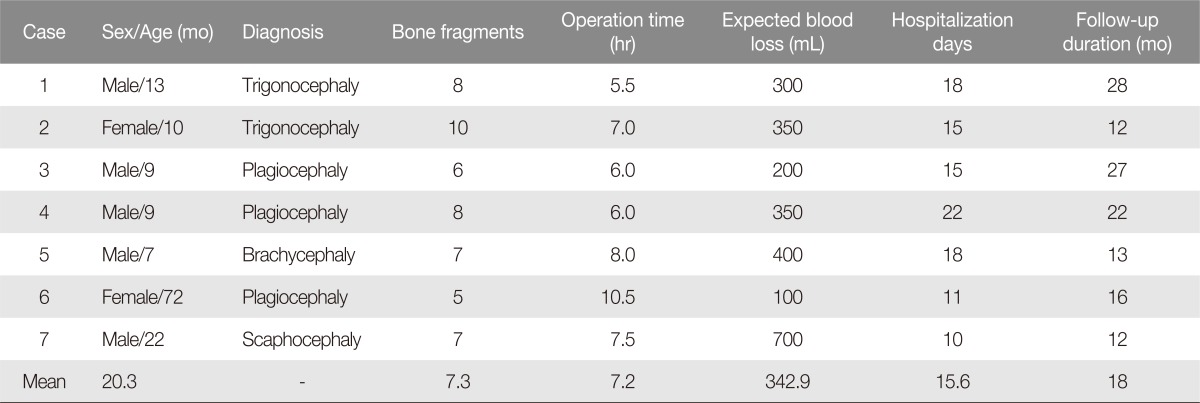
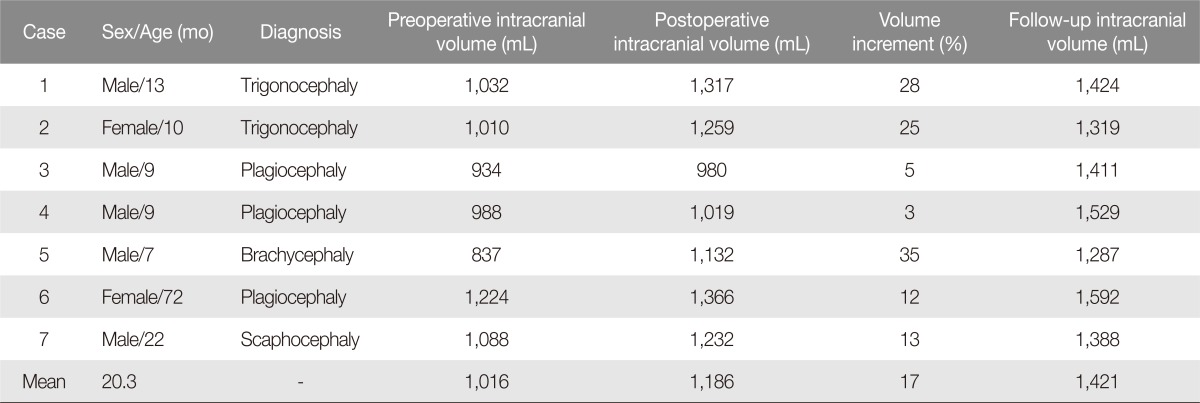
Burr holes were drilled in every expected osteotomy line corner marked with a pencil. Then, with pneumatic powered osteotome, we removed the involved synostotic cranial bone together with its surrounding areas as large as possible. Here, we ensured to include the cranial suture line already having synostosis in the osteotomized bone flap as much as possible in order to minimize the effects of prematurely-closed suture line on postoperative cranial remodeling. The resected bone flap was split into as many pieces as possible (Fig. 1). The extent of ‘multi-split osteotomy’ depends on the degree of dysmorphology, expectative volume increment after surgery and probable dead space caused by bony gap between bone segments (Fig. 2). Where necessary, we tried to move or rotate these split bone segments to find their esthetically acceptable locations. Sometimes greenstick fracture was intentionally made to induce volume expansion or reshaping was conducted through burring or rasping. In addition, if a maximum volume expansion was necessary, we employed barrel stave osteotomy partially.
‘Multi-split osteotomy’ technique applied to the anterior plagiocephaly case. (A) Involved synostotic cranial bone together with its surrounding areas were removed. (B) Bone flaps were osteotomized into 8 pieces for appropriate cranial contour.
Osteotomy design for trigonocephaly and plagiocephaly cases. (A) Trigonocephaly. Bone flaps were osteotomized into 10 pieces. (B) Posterior plagiocephaly. Bone flaps were osteotomized into 6 pieces.
Rigid interosseous fixation was performed with variable types of absorbable plate and screw including straight type, double-Y type, 5×5 square type and 5×10 rectangular type plates (Lactosorb, Biome, Inc., Warsaw, IN, USA) (Fig. 3). In this case, principally, each and every bone segment was made to have multi-point fixation with their adjacent bones in at least 3 points for more rigid and stable fixation. Also we tried to use almost all of the remaining bones to minimize the bone deficient area but did not use bone dust.

Rigid interosseous fixation was performed with variable types of absorbable plate and screw including straight type, double-Y type, 5×5 square type and 5×10 rectangular type plates (Lactosorb, Biomet Inc., Warsaw, IN, USA). Each and every bone segment was made to have multi-point fixation with their adjacent bones in at least 3 points for more rigid and stable fixation.
The elevated pericranial flap was primarily applied for the coverage of the bone defect area and area with interosseous fixation. The negative suction drain was kept then wound closure was finished layer by layer. Mild compressive dressing followed.
After the operation, the patients were monitored in intensive care unit (ICU) for 3 days. If no signs of immediate postoperative complications regarding hemorrhage, wound infection, meningitis and wound dehiscence were observed, they were moved to the general ward. For their long term results, we focused on if there was any occurrence of morphologic changes, incomplete ossification and growth disturbances in the follow-up. Normally we took 3D CT in 12 months from the operation to check the recovery status, but if there was any abnormality in physical examination, brain CT was immediately taken, regardless of the follow-up period, to check the status.
RESULTS
The number of split bone segments ranged from 5 to 10, averaging 7.3. The average operation duration was 7.2 hours. The patients' average expected blood loss was 342.9 mL (Table 1). Every patient received the transfusion of average 221.1 mL packed RBC and fresh frozen plasma.
Their hospitalization period related to the surgery was 10 to 18 days and postoperative follow-up period ranged widely from 12 to 28 months.
In one case of the patients, operative wound dehiscence was observed so debridement and local advancement flap was performed on the 14th day of the operation. The patient successfully recovered without a special problem. In 1 other case, the epidural hemorrhage was observed in the immediate postoperative brain CT first, then again in the ICU with small increase in amount. In the 2nd day of the operation, its removal was performed. The patient showed no further complication including hemorrhage since then and completely recovered. Other than these case, there was no case of wound infection, meningitis, transient or permanent neurologic deficit in this research.
The bony gaps seen in the immediate postoperative brain CT were all improved as seen in the 3D CT after 12 months from the surgery. No small bone fragment resorption was observed. The bony gaps tended to decrease thanks to the regeneration of adjacent bones (Fig. 4).
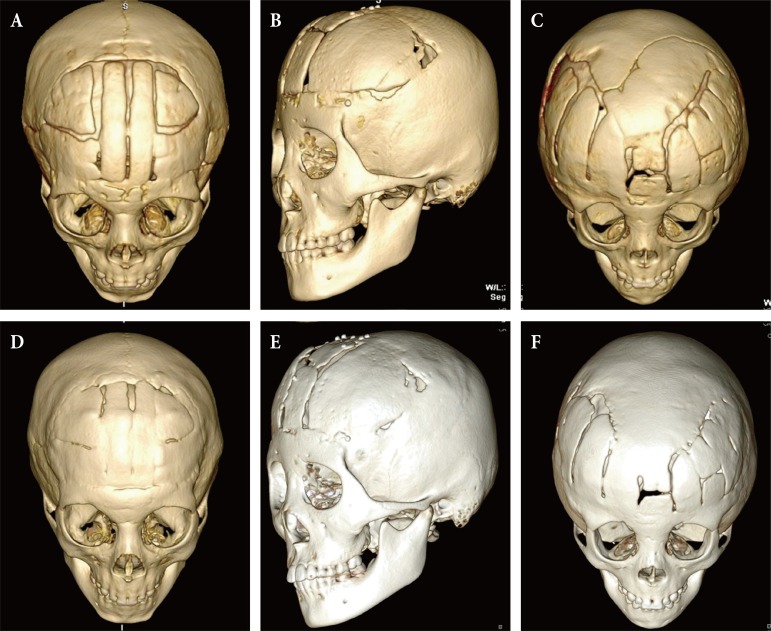
Postoperative three-dimensional computed tomography image. (A-C) Postoperative 4 months, (D-F) postoperative 12 months. The bony gaps were all improved with no small bone fragment resorption observed.
In addition, brain volume increase was found to be made gradually, leaving no case of remaining epidural dead space. Mean volume increment at immediate postoperative phase was 17%, range from 3% to 35% (Table 2). During the follow-up period up until now, there has been no case in physical examination of esthetically problematic morphological deformation, relapse diagnosis, or instability requiring the use of a protective helmet or other extra treatment.
In one of the cases, the plate was found palpable over the thin skin area of temporal region after 12 months and it disappeared in 20 months.
One patient showed preoperative developmental delay due to an unknown reason showed no big postoperative change as well but all other patients, excluding the case, displayed normal-range social interaction with the medical staff and no suspicious symptom of increased intracranial pressure.
DISCUSSION
Modern scientific description including the etiopathogenic mechanism of craniosynostosis was first made by Sömering around 1800. Since then for a long time, lots of operation methods were introduced such as complete calvarial remodeling, the pi procedure, extended vertex craniectomy for sagittal synostosis, orbitofrontal advancement for the correction of metopic, unicoronal or bicoronal synostosis, etc. [5]. Many surgeons published modifications thereof in order to reduce postoperative complication and produce better results.
Clayman et al. [5] reported useful results on sagittal suture, metopic synostosis, coronal synostosis and many others by using solely the minimally invasive endoscopic technique. Their average operation duration was 97 minutes and average estimated blood loss was 39mL, far more efficient than those of the authors of this research. However, their experiment was for patients aged younger than 4 months and performed without bone fixation, showing the difference that it need a helmet therapy for postoperative skull molding and protection. Also, it is a critical weakness that the endoscopic technique, as known widely, is difficult to apply to more aged patients.
Seruya et al. [6] analyzed postoperative outcomes of three surgical patterns regarding operative metopic synostosis correction. Depending upon coronal osteotomy line locations, they performed operation in three patterns of retrocoronal, partial coronal and precoronal procedures and analyzed pattern-specific improvement in head circumference and cranial length respectively through a long term follow-up. They reported that the retrocoronal pattern including all of the synostotic sutures in bone flaps produced the best results of them. However, since all three patterns could not completely avoid a certain level of relapse, they mentioned the need for overcorrection but admitted that such overcorrection could not guarantee long term maintenance.
In the two trigonocephaly cases under the suggested method herein, the ‘retrocoronal pattern’ was basically employed for all of the bone flaps. However, during the operation, unlike the method of Seruya et al. [6], which used three bone flaps and greensticked supraorbital bar, the authors of the present study used 8–10 bone fragments to perform the corrective operation of metopic synostosis. By doing so, this research could achieve more dramatic volume expansion.
If relatively larger-sized bone flaps are used, the original bone shape may disturb to produce fine postoperative esthetic bony contour, despite burring or other contouring treatments. But the multi-split osteotomy method herein could fundamentally reduce such a limitation, enabling more acceptable cranial vault contour production. Together with this, just as the conventional operation methods, the authors induced greenstick fracture in supraorbital bandeau midpoint and expanded outward. For its long-term maintenance, we employed a square shaped absorbable plate to reinforce the greenstick while inducing bone union with the nasal vault.
The multi-split osteotomy technique in metopic synostosis operation as mentioned above, can be applied to all of the surgical nonsyndromic craniosynostosis remedies such as plagiocephaly, brachycephaly, scaphocephaly, etc. In all cases, the technique allows an operator to perform remodeling as intended, providing easier volume expansion and more smooth esthetic contour.
As diverse shapes of absorbable plates had been used to fix rigidly, none of the research cases showed suspicious abnormality in cranial vault stability to the extent of requiring a protective helmet therapy. Average cranial volume increment was 17% at immediate postoperative phase, and cranial volume was successfully increased during follow-up period.
The time point of its surgical correction has not been defined clearly, many experts view it would be favorable to perform operation around the age of one to achieve operation goals [37]. Some craniosynostosis cases have been reported to produce a good result through the minimally invasive endoscopic approach if detected early enough [58]. But if increased intracranial pressure symptom is not observed or minor in the physical examination, such an endoscopic approach may not be operated at an appropriate time. Or if such a symptom may be initially minor but aggravate progressively, such a minimal invasive technique might also be limited in being operated at a proper time.
If neurologic deficit including increased intracranial pressure symptom is observed, immediate surgical correction is necessary. But regarding nonsyndromic craniosynostosis, such a case is only rarely seen. Thus, the authors' method can earn more time to prepare for patients' general condition or other matters of surgical operation.
Of the cases operated through the suggested method herein, 2 cases showed complications. In one case, wound dehiscence was observed due to the excessive tension in the scalp flap after cranial volume expansion. The patient recovered successfully after a simple procedure. This issue does not seem to be a big problem of the surgery method aiming at sufficient volume expansion. The other case was epidural hemorrhage. Although it needed a secondary operation, its hemorrhage amount was not large and was recovered without leaving a neurologic deficit. So it was also not deemed a problem of the multi-split osteotomy or absorbable plate itself.
The absorbable plates utilized in this research are known to maintain about 70% strength for over 8 weeks. They are consisted of 82% poly L-lactic acid and 18% poly glycolic acid for complete hydrolysis in 1 year after operation. This plate composition provides chemical parameters capable of supplement the mechanical strength of multiply osteotomized skull, which could weaken given the nature of the authors' operation, saving the use of a protective helmet. Although many plates were used, no special problem was found other than one palpable case.
Compared with the conventional surgical methods, the suggested method involved more osteotomies and its bony fragments were smaller, causing concerns over possible bone resorption. But none of the cases displayed such an unexpected bone resorption. Also, from the CT taken in 12 months after the operation, bony gaps were remarkably reduced to prove the regeneration capacity was well maintained despite smaller bone fragment sizes. This excellent finding is deemed thanks to the younger operation ages of the authors, full bony gap coverage for effective pericranium preservation and stable and rigid interosseous fixation based on various absorbable plates.
As the present research was conducted for various types of craniosynostosis cases, no objective indices such as cranial index could be used in its postoperative improvement degrees or the maintenance period thereof, and recurrence detection. Statistical demonstration was also impossible while allowing only 3D CT-based analysis. To check the development of recurrence, the follow-up period should be slightly longer. Thus, the research is being continued.
Though limited, this present research is meaningful in presenting a new possibility to be applied to not only nonsyndromic craniosynostosis but also other reconstructive cranial vault surgeries such as growing skull fracture, traumatic skull bone defect or tumor resection.
Notes
No potential conflict of interest relevant to this article was reported.