 |
 |
- Search
| Arch Craniofac Surg > Epub ahead of print |
|
Abstract
Ethmoid myoepithelial carcinoma is a rare tumor, with only 14 cases reported to date. This report discusses the largest tumor of this type ever recorded in the ethmoid region. The tumor caused extensive damage to facial structures, complicating treatment. The patient’s age and comorbidities increased the risk of intraoperative bleeding, presenting challenges to the complete removal of the tumor and the reconstruction of the damaged structures. To reduce the risk of intraoperative hemorrhage, shorten the surgery time, and manage potential heartrelated complications, arterial embolization was performed using gelatin sponges and coils. Definitive surgery was then carried out using a skin flap and mucosal flap to successfully reconstruct the defect. Postoperative radiotherapy was deemed unnecessary. The patient recovered well, with a satisfactory aesthetic outcome. No recurrence was observed during a 3-year follow-up period.
Myoepithelial carcinoma (MC) is a rare condition, typically involving the salivary or parotid glands. As of early 2022, approximately 100 cases have been reported [1-3]. The sinonasal region is an uncommon location for MC, with only 14 cases reported to date [4]. Most of these tumors are small, with the largest recorded dimension not exceeding 8 cm [4,5]. In this report, we aim to present a case of ethmoid MC more complex than those previously reported in the literature. In this case, the patient had severe comorbidities, as well as a larger mass that invaded and destroyed her right eye and the maxillary region. This resulted in a challenging removal and reconstruction following surgical resection. The tumor size in our case is the largest recorded among MCs in the ethmoid sinus. This report shares our experience with a treatment strategy that combines tumor excision and reconstruction in a single stage.
In 2019, a 74-year-old female patient was admitted to our hospital due to a tumor measuring 11.5× 8.8× 13.3 cm, which occupied nearly half of her right face (Fig. 1). The tumor invaded and compressed surrounding structures such as the right eye, maxilla, and nose, leading to vision loss and nasal obstruction. The skin overlying the tumor was well-vascularized, showing no signs of inflammation or ulceration.
On computed tomography scans, the tumor was found in the ethmoid sinus. It had a significant diameter, compressed the right cheek, and invaded the right maxilla, resulting in bone destruction (Fig. 2). Histological findings and immunohistochemistry revealed that the epithelial cells were positive for CK AE1/AE3, EMA, CD117, Bcl2, S100, P63, and SMA. This confirmed the diagnosis of a low-grade epithelial-MC, with fewer than 2 mitoses per 10 high-power fields (Fig. 3). Prior to admission, the patient had developed hypertension and atrial fibrillation, neither of which had been treated.
During the patient’s hospital stay, embolization of the right facial and maxillary arteries was carried out using a gelatin sponge and coil. This was done to reduce intraoperative bleeding and surgical time, as well as to manage heart-related complications. Two days post-embolization, the patient’s cardiac conditions had stabilized, allowing for the surgical resection to be performed. The tumor was encapsulated and had clear boundaries, which facilitated its complete removal. Initially, an H-shaped incision was made on the surface of the tumor, and the skin was dissected in four directions. The skin was conserved as much as possible for reconstructive purposes following the resection. Subsequently, the fascia was cut to fully expose the tumor. During this process, the right facial and maxillary vessels that were encountered were ligated, and hemostasis of minor vessels was achieved. We then methodically resected all tumor segments and removed necrotic tissues from the right orbit, nose, cheek, and maxillary sinus, while striving to preserve the right globe and the skin overlying the tumor (Fig. 4A). An immediate biopsy was deemed unnecessary at this stage due to the clean intraoperative removal of the tumor and its low-grade histology.
The reconstruction of the overlying tissues was carried out using the right zygomatic bone as a foundational framework. We utilized a Ginestet hook elevator to relocate, align, and reshape the cheekbone. A Foley balloon catheter was inserted into the sinus and subsequently inflated to secure the bone (Fig. 4B). Following this, we scraped the epithelial portion of the local flap in the right cheek and nose area. A mucosal flap was then transferred to seal the right posterior nasal aperture. The preserved skin was employed as an advancement flap to close the defect, eliminating the need for further tissue harvesting (Fig. 4C). Three years post-surgery, no complications were reported, and the aesthetic outcomes were satisfactory (Fig. 5). Postoperative ectropion was observed, but the patient declined adequate correction due to the associated treatment costs.
This case report details a rare instance of an ethmoid MC, the largest of its kind recorded to date. This massive tumor extended across half of the patient’s face, compressing the right eyeball and right nostril, and resulting in severe facial deformities. The size of the tumor presented a significant challenge for complete removal and subsequent reconstruction of the damaged structures. Moreover, the extensive and profuse network of feeding vessels could lead to increased intraoperative hemorrhage, blood loss, and extended surgery time. Consequently, the removal of such a large mass would inevitably result in a substantial defect that would be difficult to reconstruct postoperatively. The preoperative embolization of the tumor’s nutritional sources was aimed at reducing intraoperative hemorrhage and total blood volume loss. This procedure also improved tumor visualization and helped manage cardiovascular diseases both during and after surgery. After embolizing the facial and maxillary arteries, if there had been a need for a recipient site for a free flap following surgical excision, the ipsilateral superficial temporal artery could have been a viable option.
Both open surgery and endoscopic resection have been successful in completely removing sinonasal MCs [4]. In this particular case, we created an H-shaped incision at the center of the tumor. This approach allowed for a smooth dissection in all directions while preserving the overlying skin structures (skin and subcutaneous tissues) as much as possible. Given the large volume of the tumor, which had invaded the right nasal cavity and maxillary bone and was compressing the right eye, it was crucial to completely remove the tumor and surrounding necrotic tissues before proceeding with any plastic surgery. To reconstruct the significant defect in the right half of the face, we performed a partial zygomatic arch osteotomy. This created a framework for the overlying soft tissues, which originated from the skin and its subcutaneous structures over the tumor, to cover. We inserted a 3-way Foley balloon catheter into the maxillary sinus and inflated it. This provided additional support to the overlying tissues, prevented the accumulation of blood and fluid, and facilitated proper drainage of any excess fluid. We also closed the right posterior nasal aperture due to its loss of function. The right lower eyelid and lips were reconstructed, resulting in a satisfactory cosmetic outcome.
The use of postoperative radiotherapy remains a topic of debate among authors, but it is often employed in cases with a high risk of distant metastasis [4]. The longest reported follow-up time was 40 months without relapse in a patient with a small tumor (3 cm in size) treated by partial resection and radiotherapy, as reported by Lee et al. [6]. In our case, we did not utilize radiotherapy because the tumor was completely removed and there was a low likelihood of metastasis due to the low-grade histology and reduced vascular supply to the tumor. No relapse occurred 3 years postoperatively in this patient, demonstrating the success of our treatment strategy. This study also adds to the existing knowledge about this rare tumor, providing insights into its histology, disease progression, treatment, and long-term clinical outcomes.
Notes
Author contribution
Conceptualization: Quang Vinh Vu. Methodology: Quang Vinh Vu, Thanh Tuan Hoang. Project administration: Quang Vinh Vu. Visualization: Van Anh Tran, Thanh Hai Tong, Hong Ha Nguyen. Writing - original draft: Thanh Tuan Hoang, Van Anh Tran, Thanh Hai Tong. Writing - review & editing: Quang Vinh Vu. Investigation: Quang Vinh Vu, Thanh Tuan Hoang, Van Anh Tran, Thanh Hai Tong, Hong Ha Nguyen. Supervision: Quang Vinh Vu. Validation: Quang Vinh Vu, Thanh Tuan Hoang.
Fig. 1.
A 74-year-old female patient with an 11.5×8.8×13.3 cm tumor occupying nearly half of the right face.

Fig. 2.
Computed tomography showing a huge mass in the ethmoid region occupying half of the midface of a patient.

Fig. 3.
Histological findings showing myoepithelial cells with cystic structures. (A) Hematoxylin and eosin stain (×200). (B) CK AE1/AE3 immunohistochemistry image (×200).
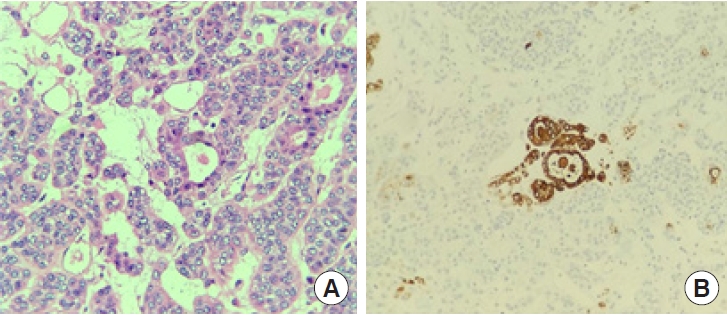
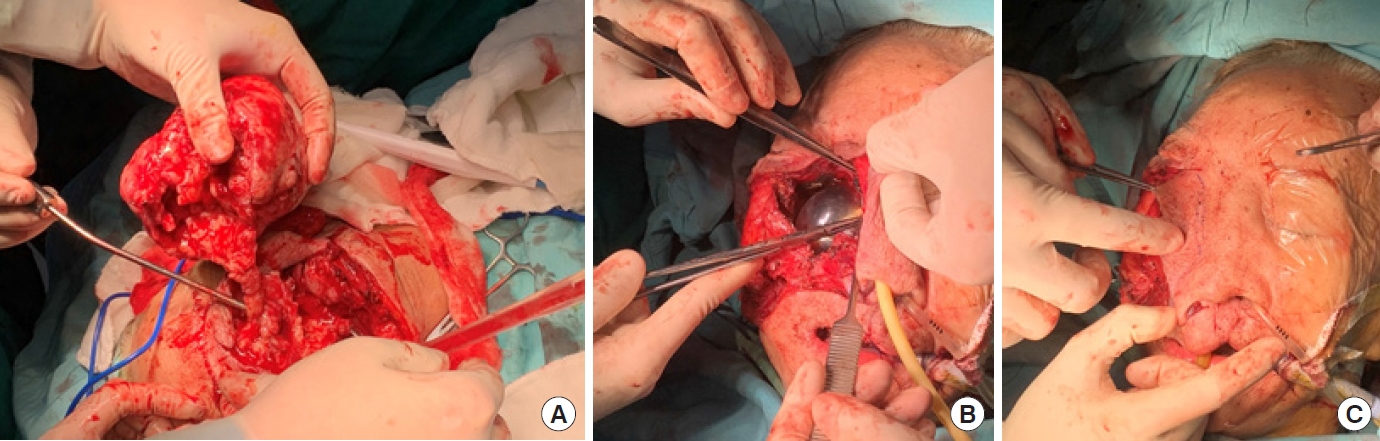
Fig. 4.
Intraoperative photographs. (A) Removal of the tumor. (B) The insertion and inflation of a Foley balloon catheter into the sinus to fix the bone. (C) Closure of the right posterior nasal aperture via mucosal flap transfer, along with an advancement flap using the preserved skin to close the defect without further harvesting any tissue.
REFERENCES
1. Politi M, Toro C, Zerman N, Mariuzzi L, Robiony M. Myoepithelioma of the parotid gland: case report and review of literature. Oral Oncol Extra 2005;41:104-8.

2. Vilar-Gonzalez S, Bradley K, Rico-Perez J, Vogiatzis P, Golka D, Nigam A, et al. Salivary gland myoepithelial carcinoma. Clin Transl Oncol 2015;17:847-55.



3. Wockner RS, Seethala RR, Emeto TI, McCaul JA, Subramaniam SS. Epithelial-myoepithelial carcinoma of the maxillofacial and sinonasal region: a systematic review of presenting characteristics, treatment modalities, and associated outcomes. Int J Oral Maxillofac Surg 2023;52:1-12.


4. Schuman TA, Kimple AJ, Edgerly CH, Ebert CS, Zanation AM, Thorp BD. Sinonasal epithelial-myoepithelial carcinoma: report of a novel subsite and review of the literature. Allergy Rhinol (Providence) 2018;9:2152656718764229.












