|
 |
- Search
| Arch Craniofac Surg > Volume 18(4); 2017 > Article |
|
Abstract
Background
Lower eyelid incisions are widely used for the orbital approach in periorbital trauma and aesthetic surgery. In general, the subciliary approach is known to cause disposition of the lower eyelid by scarring the anterior lamella in some cases. On the other hand, many surgeons believe that a transconjunctival approach usually does not result in such complications and is a reliable method. We measured positional changes in the lower eyelid in blowout fracture repair since entropion is one of the most serious complications of the transconjunctival orbital approach.
Methods
To measure the positional changes in the lower eyelids, we analyzed preoperative and postoperative photographs over various time intervals. In the analysis of the photographs, marginal reflex distance 2 (MRD2) and eyelash angle were used as an index of eyelid position. Statistical analyses were performed to identify the significance in the positional changes. All patients underwent orbital reconstruction through a transconjunctival incision by a single plastic surgeon.
Lower eyelid incisions commonly used for accessing blowout fractures or lower blepharoplasty include the subciliary and transconjunctival approaches. The subciliary incision for orbital trauma is traditionally described as an incision approximately 2 mm below the lash line. This approach has been associated with anterior lamella scarring in some cases, thus making lower eyelid malposition with scleral show and a risk of ectropion. As an alternative to the subciliary approach, a transconjunctival approach to the lower eyelid was introduced for its advantages, such as a lower risk of eyelid malposition and minimal scarring. Now, it has become one of the main techniques for the management of orbital trauma and aesthetic surgery of lower eyelids.
Numerous studies have been performed to evaluate the effectiveness and safety of transconjunctival approach in lower eyelid surgery. The vast majority of those studies, however, are retrospective and noncomparative in nature, making the deduction of valuable conclusions difficult. We measured the positional changes of the lower eyelid at time intervals after surgery since entropion is one of the most serious complications in transconjunctival approach. In this study, we performed a retrospective study to quantify positional changes in the lower eyelid and to identify the reliability of the transconjunctival approach.
A retrospective database of blowout fractures requiring operative repair between January 2011 and April 2014 was reviewed. A total of 107 patients were diagnosed with isolated one-sided blowout fracture using computed tomography. Patients with eyeball movement limitation or diplopia (n=46), lower eyelid laceration (n=2), previous incision history of the lower eyelid (n=1), and symptoms of dystopia (n=1) were excluded. Additionally, fractures not requiring surgical treatment were not included. There were 3 elderly patients over 60 years old, but all of them showed a normal lid that returns to the original position immediately on release in the snap back test. The final number of followed-up patients with isolated one-sided blowout fracture was 42. A single plastic surgeon performed the operation in the same way in a single institution.
Epinephrine (1:100,000) with 0.25% lidocaine (Xylocaine) was injected into the subconjunctival space around the lower eyelid to achieve a vasoconstrictive effect. The lower eyelid was everted using two traction sutures through the tarsal plate. The conjunctiva was incised 2 to 3 mm below the tarsus in the middle part of the lower eyelid. The conjunctiva was retracted and dissected along the bloodless submuscular plane to the orbital rim. The orbital septum was protected with a malleable retractor during the dissection to the orbital rim. The periosteum was incised and elevated. The complete orbital floor was subsequently exposed, as was the caudal part of the lateral and medial wall. The herniated soft tissue through the fractured site was reduced and miniplates or microplates were inserted, if necessary. A lateral canthotomy or cantholysis was not performed. Postoperatively, the periosteum was closed with a 6-0 fast-resorbable suture material and the conjunctiva was sutured at 3 points with an 8-0 fast-resorbable suture material. Steri-strip (3M) was applied to the lower eyelid for compression and fixation.
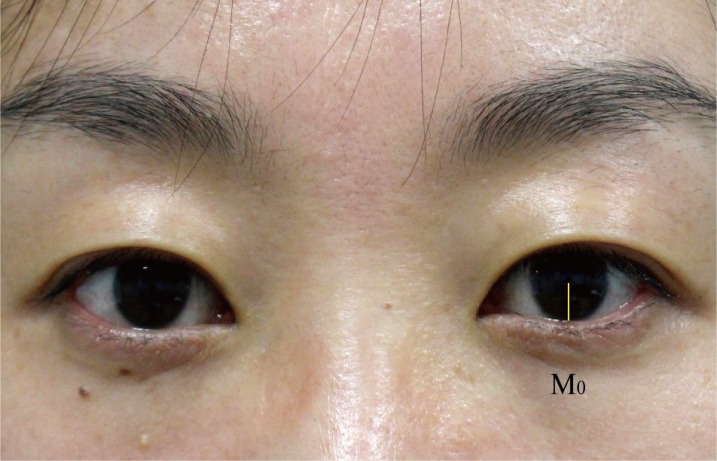
Preoperative and postoperative photographs at one week, one month, and three months follow-up were analyzed. All photographs were obtained using a Canon EOS 700D camera under same lighting conditions, with the patient in the upright-sitting position and with the eyes in primary gaze. ImageJ software (National Institutes of Health, Bethesda, Maryland, USA) was used to measure the distance (pixels) from the center of the pupil to the lower eyelid margin (marginal reflex distance 2, MRD2) and the corneal diameter (Fig. 1). We standardized the MRD2 to an arbitrary horizontal corneal diameter of 11 mm by multiplying the ratio of MRD2 to corneal diameter in pixels by 11. The preoperative MRD2 (M0) was measured on the contralateral side, while the postoperative MRD2 was measured on trauma side at 1 week (M1), 1 month (M2), and 3 months postoperatively (M3). We used the contralateral globe and lower eyelid as preoperative measurements because of swelling of the affected eyelid and periorbital region.
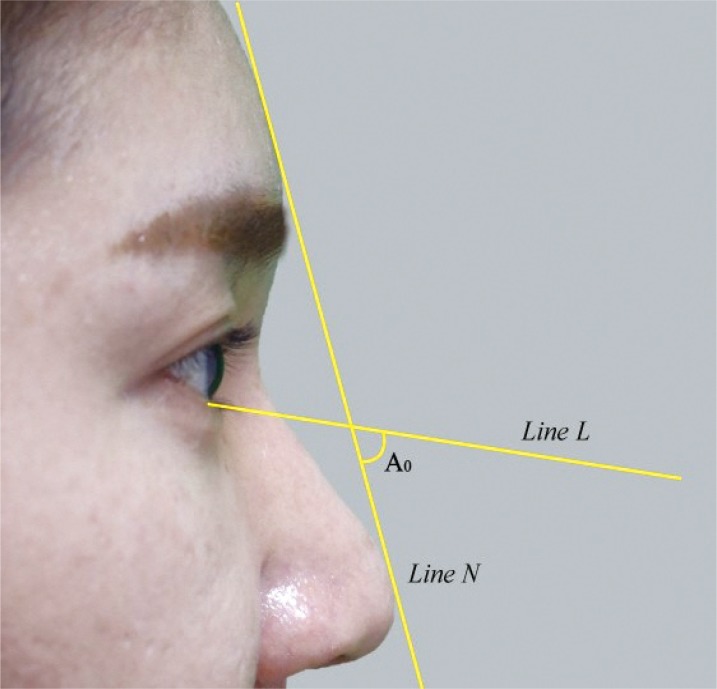
In addition, the angle at which Line L crossed Line N was measured in the preoperative and postoperative state, with L being the straight line from the root of the lower eyelid lash to the end of the lash and N being the straight line from the nasal tip to the frontal eminence. There are two reasons for which the straight line from the nasal tip to the frontal eminence was used for the eyelash angle. First, the vertical plane or horizontal plane varies according to the patient's position; however, the straight line from the nasal tip to the frontal eminence cannot vary in a person even if the straight line from the root of the lower eyelid lash to end of the lash changes; second, the line is easily affected by periorbital swelling, making it a reliable standard. The preoperative angle was measured on the contralateral side (A0) and postoperative angles were also measured on trauma side at 1 week (A1), 1 month (A2), and 3 months (A3), postoperatively (Fig. 2). All measurements were conducted three times by one person.
Statistical analyses were performed using R software ver. 2.8.1 (http://cran.r-project.org/). R packages of lme4 and lmerTest were used to fit the linear mixed effect model. Statistical hypothesis tests with p<0.05 were considered significant.
The 42 patients included 25 men and 17 women. The average patient age was 41.3 years (range, 21–72 years) and the duration from the day of trauma to the operation day was 6.07±1.16 days. There were 10 cases of medial wall fractures, 13 cases of inferior wall fractures, and the rest were combined fractures. A lateral canthotomy or cantholysis for more exposure was not done. We could not find any clinical complications such as infection, hematoma and bleeding during the follow-up period.
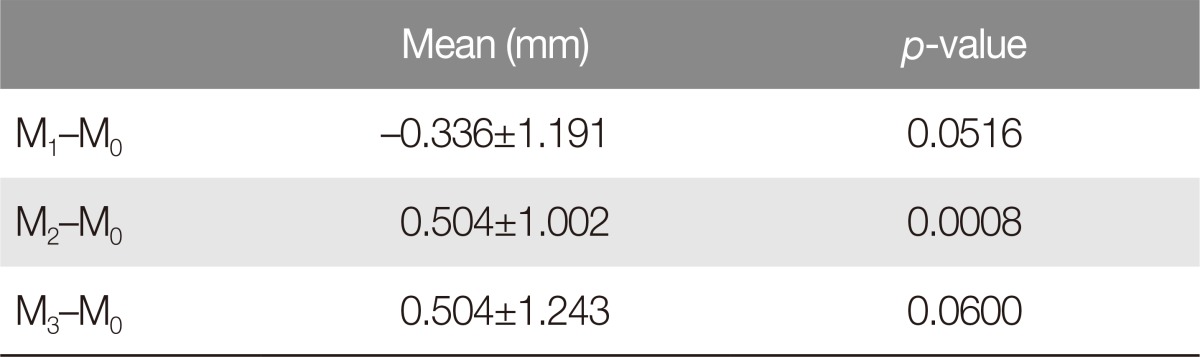
The mean M0 was 4.200±0.601 mm; mean M1, 4.168±0.608 mm; mean M2, 4.248±0.595 mm; and mean M3, 4.248±0.587 mm. The difference between M0 and M1 was −0.336±1.191 (p=0.052), between M0 and M2 was 0.504±1.002 (p=0.001), and between M0 and M3 was 0.504±1.243 (p=0.06) (Table 1). There was a significant difference between M0 and M2, but there was no statistically significant difference between the other intervals.
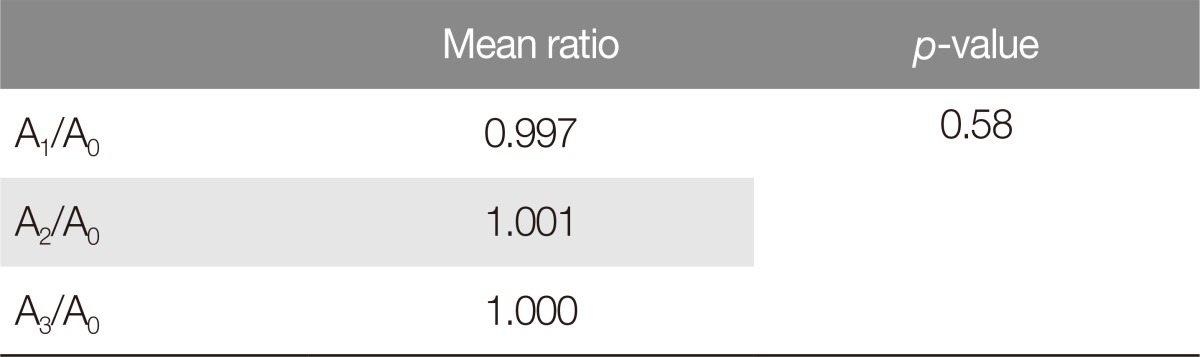
The mean ratio of the change in postoperative eyelash angle was 0.997 (1 week), 1.001 (1 month), and 1.000 (3 months), postoperatively (Table 2). At 1 week post-surgery, the lower eyelid was slightly everted but had returned to its normal position at 1 month post-surgery. There was no statistical significance in the change of the postoperative eyelash angle (p=0.58).
We measured the positional changes in the lower eyelids in blowout fracture repair using transconjunctival incision. The lower eyelid was slightly displaced at 1 week post-surgery due to periorbital swelling, but later returned to the original position. In this result, we found the statistical significance in the difference between M0 and M2, but there was no meaningful finding in the other intervals. In other words, minimal displacement in the lower eyelid at 1 month post-surgery was seen as an ectropion about 0.5 mm, but it improved and returned to normal later. So, the temporal displacement at 1 month post-surgery was thought to be clinically meaningless. In conclusion, it was found that the positional changes in the lower eyelids in the blowout fracture surgery via transconjunctival approach were not significant.
The subciliary approach has been widely used for many years in lower eyelid surgery. The skin-muscle flap usually ends with the incision of the orbicularis oculi muscle in order to expose the orbital septum. This approach enables the easy exposure of anatomical structures and makes them more visible and accessible to the surgeon for the reconstruction of the fractured site. However, this results in the inevitable injury of the anterior lamella leading to cosmetic complications such as lid retraction and pretarsal flattening in some cases. Moreover, there are buccal branches of the facial nerve on the medial pretarsal orbicularis and these may be easily damaged when the orbicularis oculi muscle is cut medially. Therefore, technical expertise, conservation of the buccal nerve branches, and meticulous hemostasis are essential for the prevention of complications [1].
As an alternative to the subciliary approach, a transconjunctival approach was first introduced due to its advantages, such as a lower risk of eyelid malposition and minimal scarring [2]. According to the literatures, the transconjunctival incision was originally described by Bourget for the removal of lower eyelid fat in 1924 [3]. It was first advocated by Tessier for the exposure of the orbit and maxilla for the treatment of trauma and congenital disease in 1973. Now, transconjunctival incisions are widely used in lower eyelid surgery by many plastic surgeons.
The transconjunctival approach for repairing orbital fractures has been noted by several authors as having a lower risk of postoperative complications, such as lid retraction, ectropion, and hematoma formation. In reality, however, this approach can also result in entropion and trichiasis due to scar formation of the posterior lamella. Ridgway reported that the transconjunctival incision was most commonly associated with entropion among the approaches used to treat combined orbital floor or zygomaticomaxillary complex fractures. Furthermore, Novelli et al. [4] and Korchia et al. [5] noted that the transconjunctival approach may cause temporary entropion and trichiasis in rare cases, but does not result in permanent complications despite the incision of palpebral retractile tissues [4,5,6,7].
In spite of these concerns, many studies suggested that the transconjunctival approach was considerably safe and reliable. Zarem and Resnick [8] reported an extensive 10-year follow-up study, which demonstrated that transconjunctival lower blepharoplasty was a superior procedure in terms of the avoidance of retracted lower eyelids and dry eyes. He could not find any lower eyelid malposition among the 104 subjects. Baumann and Ewers [9] reported that preseptal transconjunctival incision without lateral canthotomy provides good exposure of the orbital floor and the caudal parts of the lateral and medial wall, and no complications were observed in the study. Moreover, Ho et al. [10] reported the absence of eyelid malposition, including retraction, ectropion, or a scleral show, and that no other complications, such as infection, hematoma formation, and implant protrusion, were noted in any of the 26 blowout fracture patients in the study.
There are some studies based on MRD2 change between the preoperative and postoperative state of transconjunctival blepharoplasty. The mean lower eyelid position measured using MRD2 increased by 0.05 mm after transconjunctival blepharoplasty. However, there was no significant difference in lower eyelid position after either technique (p>0.5) [11]. Segal et al. [12] reported that transconjunctival blepharoplasty did not induce lid retraction but rather elevated the lower eyelid in a majority of patients using MRD2 measurement. Elevation of the lower eyelid can reduce or eliminate scleral show inferiorly, providing further cosmetic advantages.
In our study, we measured and quantified the positional changes of the lower eyelids in blowout fracture repairing via transconjunctival incision but there was no statistically significant difference between the time intervals. Moreover, there were no clinical complications, such as infection, hematoma, or bleeding. Based on these results, we suggest this approach as a safe and reliable method.
We believe that the reason for the lower rates of eyelid displacement by scar contracture on the posterior lamella is that mucosa has some advantages in terms of biological processes in wound healing. Many studies have shown that wound healing of the mucosa layer is distinct from other skin layers. Wong et al. [13] reported that scar formation was less facilitated in the oral mucosal layer than in the skin layer of humans and the Red Duroc pig. The study indicated that wound healing in the oral mucosa resulted in significantly reduced scar formation as compared with other skin layers. This was associated with the distinct molecular composition of the wound connective tissue in mucosa and other skin layers. Szpaderska et al. [14] also suggested that the higher speeds of wound healing exhibited by the mucosal layer compared to other skin layers was due to a reduced inflammatory response. The study found fewer inflammatory cells in oral mucosal wounds than other cutaneous wounds. It was supported by the measurement of decreased cytokine production in the oral mucosa. Diminished production of cytokines might be responsible for the reduced recruitment of neutrophils and macrophages. Hence, decreased intrinsic inflammatory response in mucosal wounds allowed for more rapid healing and less scar formation.
Furthermore, our findings can be explained by the microbiology and molecular activity of this type of tissue. Defensin is a small cysteine-rich cationic protein that consists of 18–45 amino acids and acts as antimicrobial peptides in the immune system as well as has a central role in wound healing and tissue remodeling [15]. Zhou et al. [16] found that human neutrophil defensing (HNP) maintained a high concentration on ocular surfaces until 3 days after ocular surgery. Furthermore, Li et al. [17] also reported that defensin contributed to the wound healing process via the modulation of conjunctival fibroblast. As a result, we can say that the high concentration of HNP on the ocular surface stimulates the proliferation and activation of conjunctival fibroblasts, which can promote conjunctival wound healing and less scarring.
There were some limitations to our study. First, the preoperative parameters were measured in non-traumatized lesions. This was inevitable because, in the presence of swelling or hematoma, the authors could not have discerned the normal lower eyelid position. Second, there were no data of a control group such as the transcutaneous approach. The author is currently collecting data of other approaches used in reconstructions to evaluate the reliability of the transconjunctival approach.
In conclusion, the advantages of the transconjunctival approach for the orbital access are minimal scarring and a lower risk of eyelid displacement compared with other methods. Additionally, other complications, such as infection, hematoma, and bleeding, are very rare. Based on our results, we recommend the transconjunctival approach for orbital exposure as a safe and reliable method.
References
1. Kim YK, Kim JW. Evaluation of subciliary incision used in blowout fracture treatment: pretarsal flattening after lower eyelid surgery. Plast Reconstr Surg 2010;125:1479-1484. PMID: 20134363.


2. Appling WD, Patrinely JR, Salzer TA. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg 1993;119:1000-1007. PMID: 8357580.


3. Lorenz HP, Longaker MT, Kawamoto HK Jr. Primary and secondary orbit surgery: the transconjunctival approach. Plast Reconstr Surg 1999;103:1124-1128. PMID: 10088496.


4. Novelli G, Ferrari L, Sozzi D, Mazzoleni F, Bozzetti A. Transconjunctival approach in orbital traumatology: a review of 56 cases. J Craniomaxillofac Surg 2011;39:266-270. PMID: 20650644.


5. Korchia D, Braccini F, Paris J, Thomassin J. Transconjunctival approach in lower eyelid blepharoplasty. Can J Plast Surg 2003;11:166-170. PMID: 24115863.



6. Mullins JB, Holds JB, Branham GH, Thomas JR. Complications of the transconjunctival approach: a review of 400 cases. Arch Otolaryngol Head Neck Surg 1997;123:385-388. PMID: 9109784.


7. Westfall CT, Shore JW, Nunery WR, Hawes MJ, Yaremchuk MJ. Operative complications of the transconjunctival inferior fornix approach. Ophthalmology 1991;98:1525-1528. PMID: 1961638.


8. Zarem HA, Resnick JI. Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg 1991;88:215-220. PMID: 1852813.


9. Baumann A, Ewers R. Use of the preseptal transconjunctival approach in orbit reconstruction surgery. J Oral Maxillofac Surg 2001;59:287-291. PMID: 11243611.


10. Ho VH, Rowland JP Jr, Linder JS. Sutureless transconjunctival repair of orbital blowout fractures. Ophthal Plast Reconstr Surg 2004;20:458-460.


11. Taban M, Taban M, Perry JD. Lower eyelid position after transconjunctival lower blepharoplasty with versus without a skin pinch. Ophthal Plast Reconstr Surg 2008;24:7-9.


12. Segal KL, Patel P, Levine B, Lisman RD, Lelli GJ Jr. The effect of transconjunctival blepharoplasty on margin reflex distance 2. Aesthetic Plast Surg 2016;40:13-18. PMID: 26537512.



13. Wong JW, Gallant-Behm C, Wiebe C, Mak K, Hart DA, Larjava H, et al. Wound healing in oral mucosa results in reduced scar formation as compared with skin: evidence from the red Duroc pig model and humans. Wound Repair Regen 2009;17:717-729. PMID: 19769724.


14. Szpaderska AM, Zuckerman JD, DiPietro LA. Differential injury responses in oral mucosal and cutaneous wounds. J Dent Res 2003;82:621-626. PMID: 12885847.


15. Lai Y, Gallo RL. AMPed up immunity: how antimicrobial peptides have multiple roles in immune defense. Trends Immunol 2009;30:131-141. PMID: 19217824.



16. Zhou L, Huang LQ, Beuerman RW, Grigg ME, Li SF, Chew FT, et al. Proteomic analysis of human tears: defensin expression after ocular surface surgery. J Proteome Res 2004;3:410-416. PMID: 15253421.


17. Li J, Raghunath M, Tan D, Lareu RR, Chen Z, Beuerman RW. Defensins HNP1 and HBD2 stimulation of wound-associated responses in human conjunctival fibroblasts. Invest Ophthalmol Vis Sci 2006;47:3811-3819. PMID: 16936092.


- TOOLS
-
METRICS

-
- 5 Crossref
- Scopus
- 4,533 View
- 102 Download
- Related articles in ACFS