INTRODUCTION
Cutaneous adnexal tumors are caused by the morphologic differentiation of primary adnexal structures in the hair follicles, sebaceous glands, apocrine glands, and eccrine glands. Among these, trichoblastic carcinoma is a rare malignant follicular neoplasm. It involves malignant transformation of the trichoblastoma. We report a rare case of giant trichoblastic carcinoma that developed after excision of a trichoblastoma in the nuchal area of a 25-year-old man.
CASE REPORT
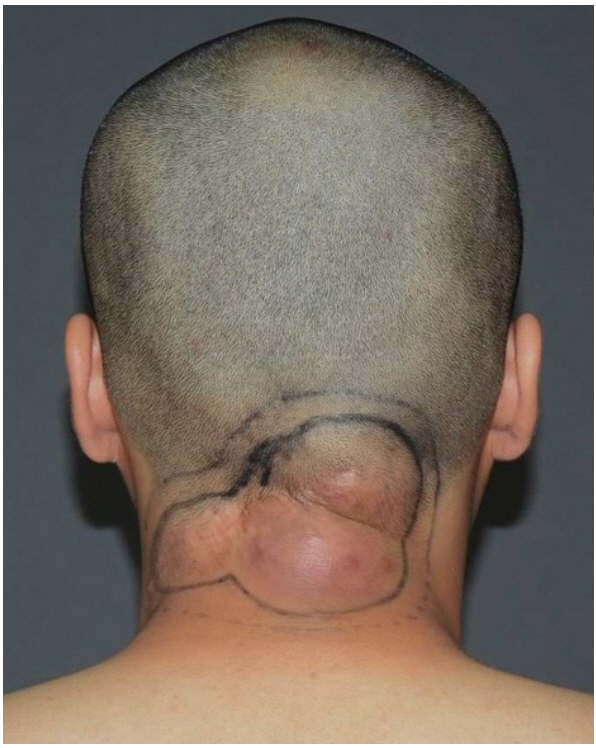
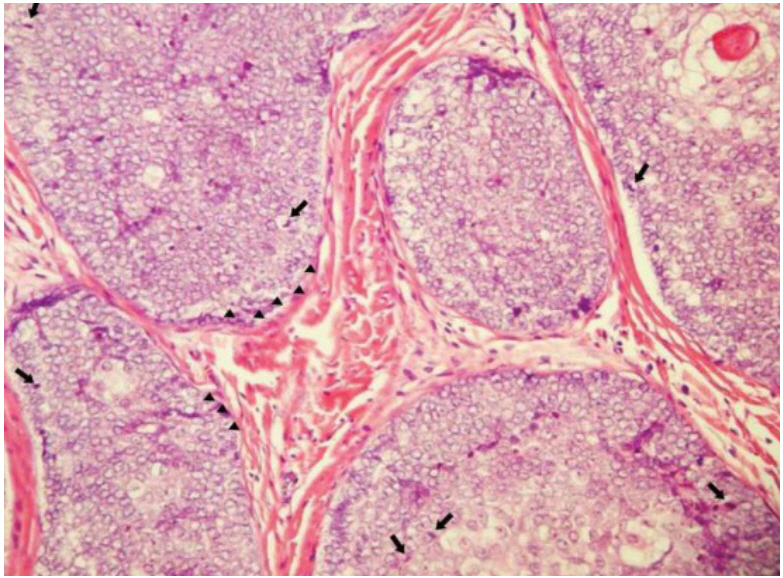
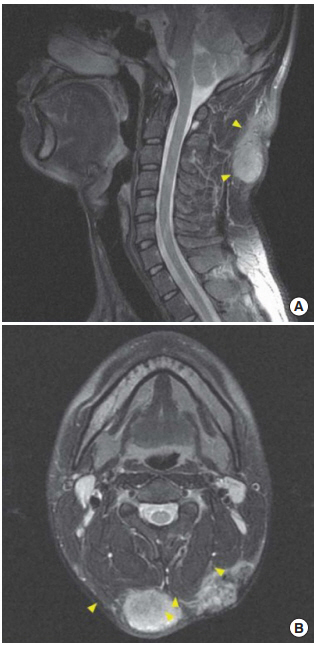
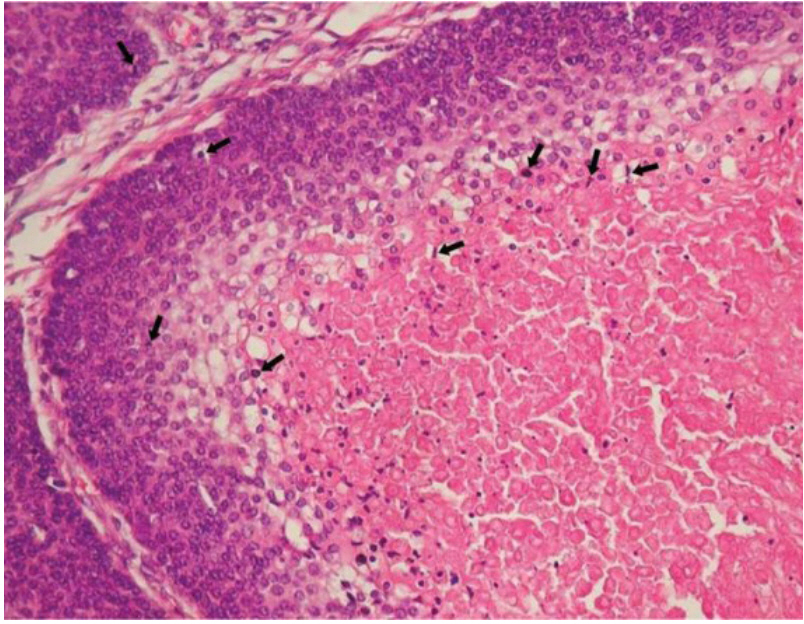
A 25-year-old man was admitted with trichoblastoma in the nuchal area with frequent recurrences since birth. The mass gradually increased to walnut-size, and the first excision surgery was performed in a local medical center (LMC) 3 years ago. The mass recurred at the same location and the patient underwent a second excision surgery at the LMC and was diagnosed with trichoblastoma after biopsy. After excision, the mass recurred with an increased size, and a third excision was performed in the LMC. However, when the mass recurred at the same site for the fourth time, the patient was transferred to our department (Fig. 1). The patient’s history, family history, and results of the laboratory study were unremarkable. A palpable lymph node was found in both, the internal jugular and popliteal cervical areas, and ultrasonography-guided aspiration was performed, but no metastasis was observed. The pathological diagnosis after the third excision surgery in the LMC was adnexal tumor with hair follicle differentiation with nonmalignant potential with involvement of the base. Immunohistochemistry results were positive for cytokeratin (+), p53 (−), and Ki-67 (1+). For accurate diagnosis, we requested for the specimen to be examined again in our pathology department. The specimen was identified as a skin adnexal carcinoma, of hair follicle origin and lowgrade malignancy (Fig. 2). The preoperative neck magnetic resonance image (MRI) revealed lobulated soft tissue lesions involving superficial fascia and infiltrating into both proximal trapezius muscles (Fig. 3). Positron emission tomography-computed tomography (PET-CT) revealed three hypermetabolic mass lesions about 4 cm in size on the subcutaneous layer of the posterior neck, and no distant metastases was observed. In the plastic surgery department, wide excision including a 1.5-cm safe margin and reconstruction with a free anterolateral thigh flap were performed. After extensive excision, histological examination revealed skin adnexal carcinoma, originating from the hair follicles, and low granular malignancy, consistent with trichoblastic carcinoma, with clear resection margin (Fig. 4). Even though partial flap necrosis had occurred, it was treated with debridement and split thickness skin graft. Neck MRI performed at 6 months postoperatively and PET-CT at 1 year postoperatively showed no remnant mass, recurrence, or distant metastasis. There was no palpable mass 5 years postoperatively, and there was no recurrence on follow-up of 5-year neck CT and PET-CT (Fig. 5).
DISCUSSION
Trichoblastic carcinoma is a malignant type of trichoblastoma that occurs in the adnexal structures. Headington and French [1] first described it as a primary neoplasm of the hair matrix in 1962. Trichoblastic carcinoma usually occurs as a malignant transformation of the trichoblastoma, but is very rare. Thus far, only 13 cases have been reported in the literature [2]. The pathogenesis of trichoblastic carcinoma is unknown [3]. It occurs mainly in patients younger than those with basal cell carcinoma. Unlike other skin cancers, it occurs in non–sun-exposed areas. It is a solitary, poorly circumscribed, large, asymmetric, dermal or subcutaneous mass. Trichoblastic carcinomas are rare and difficult to diagnose, but histopathological findings include atypical basaloid keratinocytes with crowded, hyperchromatic nuclei, and increased mitotic activity. The presence of hypercellular stroma is a criterion for distinguishing trichoblastic carcinoma from basal cell carcinoma [4]. A standard treatment has not yet been established, but most cases have been treated with surgical excision similar to the treatment for other skin cancers. When local or systemic metastasis is present, chemotherapy or radiotherapy can be performed, but this has not yet been defined [5].
In our department, the mass was excised with a safety margin of 1.5 cm and there have been no recurrences till date. Hence, wide excision with regular follow-up should be conducted in cases of trichoblastoma due to the possibility of malignant transformation. In conclusion, trichoblastic carcinoma is a rare skin adenocarcinoma; thus, the lack of definitive diagnosis and treatment is challenging. We report the biggest giant trichoblastic carcinoma in the literature.