INTRODUCTION
The nose is an important midfacial structure with social and psychological significance and complicated esthetic and functional features. For these reasons, nasal reconstruction is a challenging procedure. Facial deformities, especially nasal defects, pose problems both from a functional standpoint and for social reintegration because their appearance is likely to trigger aversion. The reconstruction of nasal defects involves the appropriate reconstruction of three separate structural layers (the inner mucosal lining, middle osseocartilaginous support, and external skin cover), which should be properly restored to maintain a functional nasal airway for ease of breathing and to ensure an acceptable appearance.
Various surgical procedures can be used for nasal reconstruction, such as skin grafting, local flaps, and distal flaps, depending on the defect’s location, extent, and condition [
1]. However, the currently available nasal reconstruction guidelines are primarily based on Caucasian physical features, and reconstructive surgery in Asian patients tends to yield less satisfactory results due to racial differences in anatomy and healing physiology [
2]. Among the available procedures, flap reconstruction requires meticulous compliance with the principle of esthetic subunits of the nose proposed by Burget and Menick [
3].
Asian skin phototypes range from Fitzpatrick types III to V and are prone to hyperpigmentation, hypertrophic scars, and keloids [
4-
6]. Compared with Caucasians, Asians generally have a small nose, wide and low radix, thick skin, abundant subcutaneous fibroadipose tissue, more sebaceous glands, and a lower quantity and poorer quality of cartilage; Asians also tend to present increased pigmentation and midfacial protrusion [
7-
9]. For this reason, Asians are also more likely to develop hypertrophic scars, hyperpigmentation, and scar contracture. Considering these anatomical and physiological features, somewhat disappointing results are expected from classical subunit reconstruction due to an underlying structure that cannot withstand the high tension caused by contracture.
According to the subunit principle introduced by Burget and Menick, the scar should be positioned along the border of the subunits to minimize its visual effect [
10,
11]. However, it has been reported that transferred flaps showed more contracture than the surrounding skin, resulting in displacement of the final scar position; therefore, a defect-adjusted flap design modifying the subunit principle was used and satisfactory surgical results were obtained [
2]. These discrepancies in nasal reconstruction surgery underscore the need for new treatment guidelines focusing on Asians.
Against this background, we considered it necessary to apply the principles of nasal reconstruction surgery in a differentiated manner for Asians and performed nasal reconstructive surgery with modified skin graft, flap, and reinforcement procedures, taking into account the differences in structural anatomy and healing physiology of Asians. This study evaluated the outcomes of a practical nasal reconstructive surgical approach that considered the specific features of Asian patients.
METHODS
A retrospective analysis was performed of the medical records of 76 patients who presented with nasal defects and underwent nasal reconstruction surgery from January 2010 to June 2020. A comprehensive evaluation was conducted on patients’ baseline demographics and clinical characteristics, including age, sex, medical history, defect size and location, type of reconstructive procedure, pathologic diagnosis, postoperative complications, and the presence or absence of recurrence. The location of each defect was classified into five subunits: Ala, lateral sidewall, nasal tip, nasal dorsum and multiple subunits.
Patients with tumors received a punch biopsy at the department of dermatology. If the punch biopsy confirmed a malignant tumor, skin tumor ablation was performed according to the safety margin determined based on the initial pathological diagnosis of the lesion. Any pathological finding of a residual tumor observed 1 mm away from the lesion excision site intraoperatively by frozen biopsy was considered to indicate insufficient resection, and additional resection was performed. Defects caused by tumor ablation were reconstructed immediately after surgery, followed by a secondary reconstructive procedure for defects caused by scarring or infection after wound stabilization. Plastic surgeons performed various surgical procedures, such as skin grafting and local flaps, depending on the defect’s location or condition. Short term follow-up was done at postoperative weeks 1, 2, 4 to and 24 to detect complications, and long-term follow-up was done every 6 or 12 months after surgery to evaluate recurrence or scar contracture. Each patient provided consent for their information (photographs) to be presented in this study. The Institutional Review Board of Inje University Busan Paik Hospital granted exemptions from anonymized data management and patient consent.
RESULTS
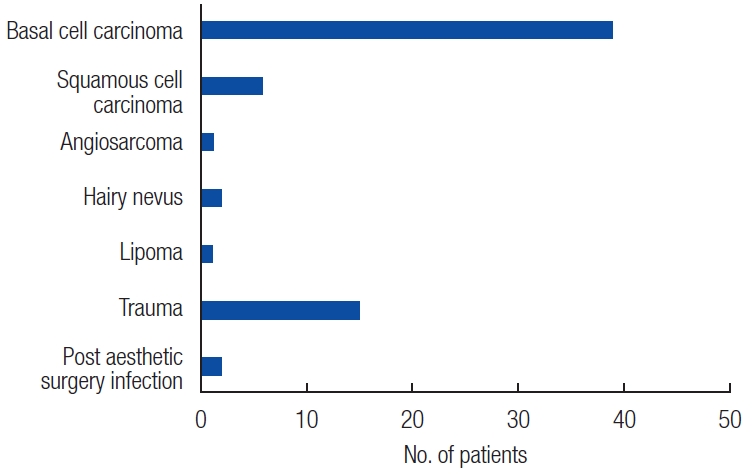
The average age of the patients was 65.2 years (range, 6–90 years), 36% of patients were male (n=35), 54% of patients were female (n=41), and the postoperative follow-up period ranged from 6 months to 8 years. Of 76 total cases of nasal defects, 59 (77%) were due to tumor ablation, while the remaining 17 cases consisted of 15 (20%) cases of post-traumatic damage and two (3%) cases of infection-induced tissue damage. The most frequent underlying nasal tumor was basal cell carcinoma (39/59, 66%), followed by squamous cell carcinoma (6/59, 10%) (
Fig. 1).
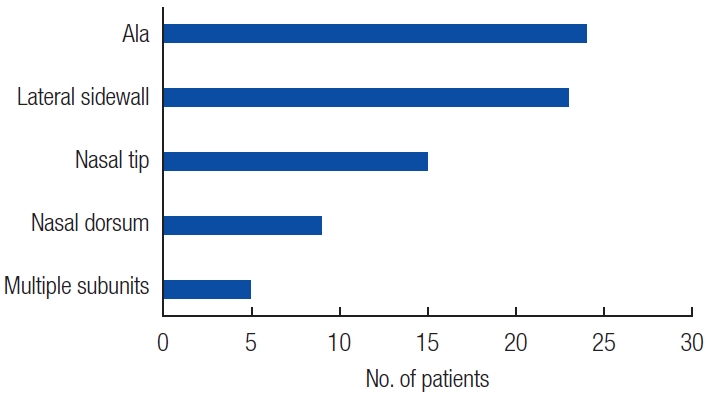
Etiologically, two cases deviated from those in previous reports. Both were nasal defects due to infection after aesthetic surgery. In one case, postoperative necrosis of nasal tip had led to a secondary infection, resulting in a nasal defect at the severity level of subtotal resection of distal nose. In another case, a nasal defect had been caused by an infection after receiving augmentation rhinoplasty with silicone nasal implant. The most common defect location was the alae (n=24, 31%), followed by the lateral sidewall (n=23, 30%), nasal tip (n=15, 20%), nasal dorsum (n=9, 12%), and multiple subunits (n=5, 7%) (
Table 1,
Fig. 2).
Forehead flaps were the most frequently used reconstruction technique (n=29, 38%), followed by nasolabial advancement flaps (n=14, 19%), rotation flaps (n=13, 17%), and skin grafts (n=11, 14%) (
Table 1,
Fig. 3). Cartilage grafting was additionally performed in 12 cases with accompanying damage to the lower lateral cartilage and upper lateral cartilage. The most frequent cartilage donor site was the auricular cartilage (n=5), followed by the costal cartilage (n=4), and nasal septal cartilage (n=2). Cartilage grafts were used primarily for reinforcing flaps and supplementing cartilage defects caused by resection. Each procedure was performed considering Asian-specific aspects of structural anatomy and healing physiology.
Complications included nasal deformity, hypertrophic scarring, secondary infection, and minimal partial flap necrosis; however, no complications required additional surgery. There were two cases of tumor recurrence, but without any significant effect on flap integrity.
DISCUSSION
Nasal defects due to skin cancer, trauma, and other causes are characterized by functional impairment and problems with social reintegration due to an unaesthetic appearance that is likely to trigger aversion. However, reconstruction or restoration is highly challenging from a surgical standpoint due to the anatomical complexity and functional and esthetic importance of the nose, which consists of several three-dimensional concave and convex surfaces surrounded by the eyes, mouth, and esthetically sensitive organs. Therefore, microfine tension in this area can easily cause facial deformation. Surgeons have devised various surgical procedures to solve this challenge in light of the esthetic importance of the nose [
12-
15]. However, since these reconstructive surgical procedures were designed for Caucasian anatomical characteristics, they can result in somewhat disappointing clinical outcomes in Asians, who have different anatomical structures and physiological features relevant for wound healing.
Compared with Caucasians, the noses of Asians have a weak overall skeletal structure because of the small and weak alar cartilage. In contrast, the sebaceous glands and fibrillar adipose tissue are well-developed because the nasal dorsum is low and wide due to a less-developed nasal septal cartilage, and the nasal tip has a relatively thick dermis [
16,
17]. Asians’ skin phototypes, which are classified as Fitzpatrick types III-V, make them prone to hyperpigmentation, hypertrophic scars, keloids, and scar contracture [
18,
19]. The wound-healing process in Asians is reportedly associated with more intense fibroblast concentration and collagen deposition than in Caucasians, suggesting that scar management guidelines for Caucasians may not be appropriate for Asians [
4-
6]. To summarize, Asians have a weaker nasal skeletal structure than Caucasians but experience stronger contraction forces during wound healing, making Asians vulnerable to deformation after nasal reconstruction.
The golden rule in flap nasal reconstruction is the subunit principle of Burget and Menick. This strategy minimizes visual scarring by excising the entire subunit and reconstructing it with a flap if a nasal defect covers more than 50% of a subunit, with the closure lines positioned along the subunit borders [
3]. More recently, however, Hsiao et al. [
2] reported that strictly following this principle is suboptimal due to the intense scar and flap contracture present in Asians due to different wound healing mechanisms between Asians and Caucasians. Therefore, better surgical outcomes could be obtained by modifying the principle of the esthetic subunits of the nose. This led us to believe that it is necessary to revise the guidelines or customize their application by considering racial differences when performing nasal reconstruction in Asian patients.
The easiest method to address skin defects is primary closure, which is recommended for minor defects (≤1 cm) involving a small amount of sebaceous gland tissue in Caucasians [
20]. However, considering that Asians’ nasal tissue, which has abundant sebaceous glands, does not respond well to closure despite sufficient dissection, we lowered the criterion for primary closure to defects ≤7 mm in diameter. Although patients with nasal defects treated with primary closure were excluded from this study’s analysis, if the above criteria were met, primary closure was performed with sufficient dissection and subcutaneous closure, and the patients’ conditions were resolved without complications.
Simple reconstruction methods (e.g., secondary healing or skin grafting) could be applied to cases with superficial nasal defects due to trauma, but we minimize the application of such simple methods and reconstruct nasal defects through flap surgery in most cases. The reason for this was that Asians, with Fitzpatrick III-V skin phototypes, tend to develop hyperpigmentation, making the esthetic outcomes less satisfactory. In the 11 skin graft cases reported in this study, the method was chosen based on the patient’s preference to simplify the treatment process despite the medical staff’s recommendations.
Local flaps are a widespread nasal reconstruction technique. In particular, surgeons often prefer proximal local flaps because their color and texture are similar to those of the defect location, the final scar is positioned near the defect, and the procedure is relatively simple. In this study, the criteria for local flap was lowered by 3mm from the criteria suggested by Zitelli and Fazio [
21]. Patients with nasal defect between 0.7 cm and 1.2 cm were treated with local flaps. Nasolabial advancement flaps were the most frequently used type of local flap, followed by rotation flaps and bilobed flaps (
Figs. 4,
5). The flap size was designed to be 10% larger than the defect size rather than accurately matching the flap size with the defect size, in anticipation of scar and flap contracture. No complications, such as flap necrosis, infection, or wound dehiscence, were observed, but additional flap reduction was required in three of the 35 cases.
If local flaps and grafts are insufficient, a forehead flap can be an excellent option for nasal reconstruction due to the reliability of the pedicle and the similarity of the skin [
22,
23]. When reconstructing large defects or reinforcing skeletal structures such as cartilage, a distant flap (e.g., a forehead flap) was used to avoid the risk of deformation of the perinasal structures (e.g., the inner canthus and nasal alae) (
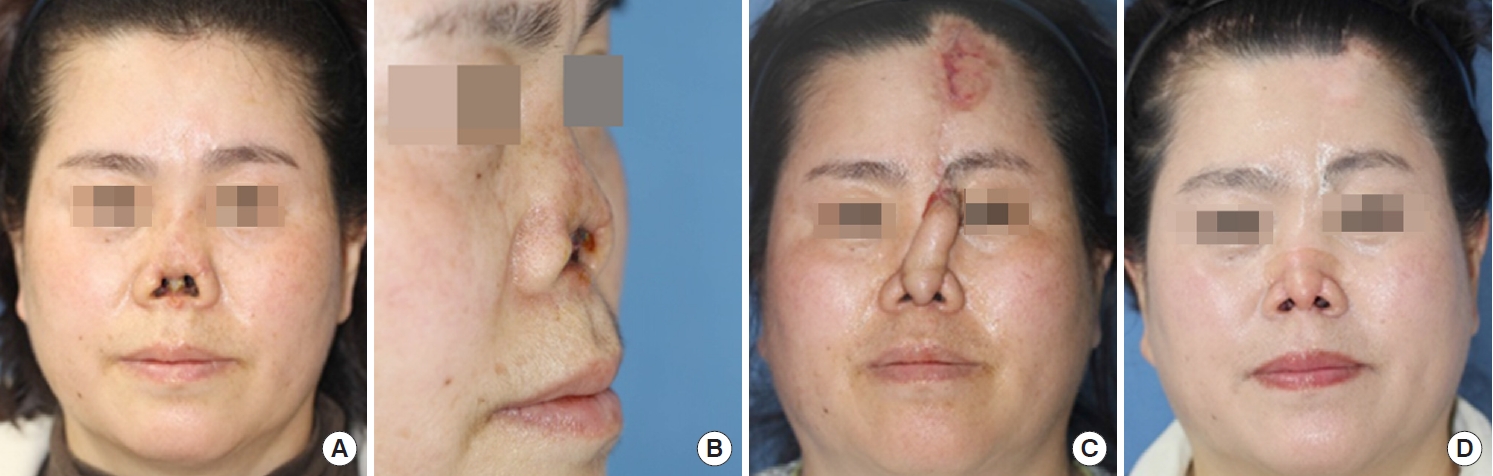
Figs. 6,
7).
We used forehead flaps in 29 of 65 cases of flap reconstruction, a higher proportion than was reported in an earlier study [
15,
23]. A template of the defects was made from the aluminum suture packaging and used to trace the forehead donor site. A pedicle width of 1.5 cm was designed and elevated along the ipsilateral forehead. Pedicle division was performed approximately 3 weeks after the initial surgery. We considered using forehead flaps for nasal defects >1.2 cm, 3 mm lower than the criteria suggested by Zitelli and Fazio [
21] This discrepancy reflects the flap design customized for Asian patients, taking into account the racial difference in anatomical contracture (i.e., the fact that Asians exhibit stronger scar and flap contracture during the healing process due to the structural fragility of their smaller noses and lower quantity of nasal septal cartilage, resulting in nasal asymmetry).
Zitelli and Fazio [
21] recommended primary closure, delayed full-thickness skin grafting, or a rotating flap for defects <1.5 cm with intact cartilage; a two-stage nasolabial flap or and forehead flap for shallow and deep (involving the cartilage) defects between 1.5 and 2.5 cm, respectively; and a forehead flap for deep and large defects (≥2 cm) [
24]. The criteria for nasal reconstruction in this study deviates from previous recommendations; therefore, based on our results, the nasal reconstruction guidelines need to be modified and customized for Asians. Thus, we developed a simple algorithm of nasal reconstruction suitable for Asians according to the location and size of the nasal defects (
Fig. 8).
Considering the variable results of nasal reconstruction caused by scar and flap contracture in Asian patients due to the differences in their healing mechanisms from those of Caucasians, we applied the principle of minimum resection and maximum restoration, rather than strictly adhering to the subunit principle, and obtained satisfactory surgical outcomes. We expanded the available range of forehead flaps by lowering the criteria for the size of nasal defects to prepare scar and flap contracture.
Hsiao et al. [
2] pointed out the difficulties associated with nasal reconstruction in Asians, arguing that the Asian nose is prone to collapse and deformation due to structural weakness, apart from the relatively strong scar and flap contracture at the defect location. In agreement with this opinion, we attempted reconstruction procedures that focused on reinforcement beyond the scope of replacing the defect with a flap or skin graft, with the goal of reinforcing the weaker cartilage structure of Asian patients compared to their Caucasian counterparts. The most frequently used type of cartilage was auricular cartilage, which was used primarily in alar reconstruction as a stiffener to prevent scar depression or deformation when the nasal cartilage at the defect site was damaged or excessively exposed. The septal cartilage was also reinforced with costal cartilage fragments to maintain the central skeletal structure when it was difficult to maintain symmetry with a flap alone due to damage to skeletal structures such as cartilage.
Complications included minimal flap margin necrosis (n=2), nasal obstruction (n=2), and nasal alar deformity (n=3). However, none required additional surgical procedures (
Fig. 9). This complication rate is lower than has been previously reported [
25], which further justifies a new evaluation of modified approaches to nasal reconstructive surgery that reflect the specific features of Asians.
Furthermore, unlike previous reports, the two cases of infection- induced nasal defects reported in this study were secondary infections after esthetic surgery [
26]. In both cases, nasal defects were caused by infection after undergoing rhinoplasty at another plastic surgery clinic. One case was associated with infection after open rhinoplasty resulting subtotal necrosis of distal nose. Another patient was a case of 1.5 cm defect in nasal dorsum after augmentation rhinoplasty via closed approach using a silicone nasal implant. In these patients, severe scar contracture occurred, and important delineation points of the nose were lost. In the reconstructive procedures for these patients, it was essential to determine the scope of the defect itself, excluding the effects of scar contracture. In these cases, we faithfully applied the principle of esthetic subunits of the nose or that of symmetry to ensure sufficient relaxation of the contracture effect. At the same time, reinforcement work such as cartilage grafting was actively applied to prevent the expected postoperative secondary contracture. In light of the increasing popularity of aesthetic plastic surgery, similar nasal defect cases are expected to become more common, further underscoring the importance of establishing related treatment guidelines.
In conclusion, we performed reconstruction of nasal defects in Asian patients by modifying the existing reconstruction principles, taking into account the racial characteristics of Asians. This customized application of basic principles enabled a low complication rate with esthetically and functionally satisfactory surgical outcomes.