 |
 |
- Search
| Arch Craniofac Surg > Volume 15(1); 2014 > Article |
Abstract
Sebaceous carcinoma is a rare malignant tumor differentiated from the adnexal epithelium of sebaceous glands and forms less than 1% of all cutaneous malignancies. We present a case of a 93-year-old woman with a rapidly growing mass on the right cheek. Initial histiopathologic finding was basal cell carcinoma. The mass was widely excised and superficial parotidectomy was performed while preserving the facial nerve branches. The resulting defect was covered with a transposition flap from the ipsilateral posterior auricular area and the donor site was closed primarily. However, histopathologic examination of the excised mass showed a poorly differentiated sebaceous carcinoma with a clear resection margin. The diagnosis of sebaceous carcinoma can be difficult to make at initial presentation. This report describes a rare case of a rapidly growing extraocular sebaceous carcinoma, which resulted in a good treatment outcome, and provides a review of relevant literature.
Sebaceous carcinoma is a rare malignant tumor differentiated from the adnexal epithelium of sebaceous glands and forms less than 1% of all cutaneous malignancies. It is estimated that approximately 25% of all reported cases of sebaceous carcinoma occur in extraocular site. It has been reported that more than 70% of sebaceous carcinomas are located in the head and neck regions, where sebaceous glands are most commonly located [1,2]. This is a report of our experience of a rapidly growing sebaceous carcinoma on the right cheek of an elderly woman.
A 93-year-old woman visited our hospital with a chief complaint of palpable mass over the right cheek. The mass began to appear about 1 year ago and was gradually enlarged (Fig. 1). On physical examination, a round, 2.0├Ś1.5 cm sized erythematous mass was observed on her right cheek. The patient complained of a slight itching sense, but neither pain nor tenderness was observed. The patient had no specific underlying disease, no history of operation, no history of radiation therapy and no familial history of cancer.
Punch biopsy was performed at the dermatology department and the pathological findings confirmed the diagnosis of basal cell carcinoma. The patient and her family were hesitant to undergo surgery because of her old age. About 7 months later, the patient revisited us for surgery with a significantly enlarged 5.5├Ś4.5├Ś4.0 cm sized mass (Fig. 2). It was confirmed that the mass began to grow rapidly about 2 weeks ago without trauma or any specific medical history. It showed focal ulceration with yellowish purulent discharge. The patient suffered from pain, and mild tenderness was also observed. However, there was no localized or generalized lymphadenopathy and her facial nerve function was intact.
We recommended other radiologic examinations to identify the degree of tumor invasion and metastasis, but those could not be progressed because the patient and her family wanted only a palliative treatment.
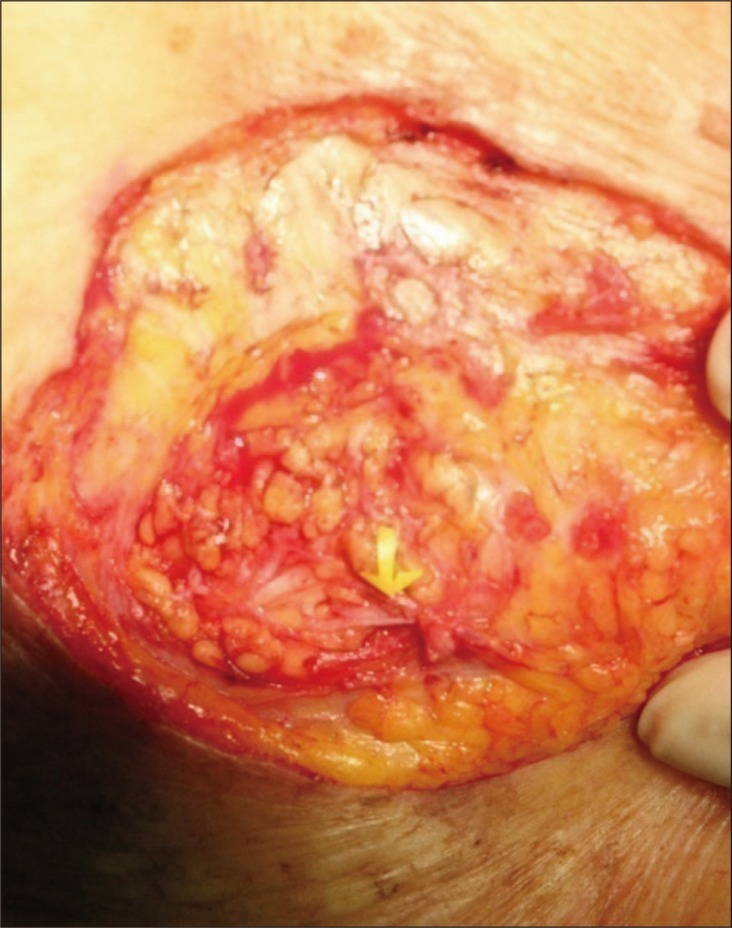
Under general anesthesia, the mass was widely excised with a safety margin of 5 mm, and superficial parotidectomy was performed because of tumor invasion to the parotid gland (Fig. 3). Based on the result of frozen biopsy, the resection margin was clear, so that we could preserve the facial nerve branches (Fig. 4). The resulting defect was covered with a transposition flap from the ipsilateral posterior auricular area (Fig. 5) and the donor site was closed primarily (Fig. 6).
A tumor of sebaceous glands usually starts as a solitary, erythematous or often pale yellow-colored, firm-to-hard, slowly growing nodule mainly in the head and neck regions. It is a rare malignant neoplasm comprising less than 1% of all cutaneous malignancies. The most common site for sebaceous carcinoma is the eyelids. Reported ocular sebaceous carcinoma was approximately three-times more common than the extraocular sebaceous carcinoma [1,2,3]. However, Dasgupta et al. [4] reported that 38.7% of sebaceous carcinomas occurred on eyelids. Dores et al. [5] reported that 45.9% of sebaceous carcinoma occurred on eyelids. This difference in the reported proportion was not only because of population-based studies of sebaceous carcinoma that have been infrequent, but also due to a small number of cases studied [5].
In general, extraocular sebaceous carcinoma is less aggressive than ocular sebaceous carcinoma [4]. However, some authors have reported that extraocular tumors preferentially show a rapid growth. This is especially true in elderly women [6]. In the present patient, the lesion was rapidly growing in just 2 weeks.
Sebaceous carcinoma may be associated with Muir-Torre syndrome, defined as an autosomal dominant genetic trait, and the presence of one or more sebaceous tumors (adenoma, epithelioma, or carcinoma) in association with at least one visceral malignancy. It is shown related to germ line mutations in the MSH2 and MLH1 genes found on chromosomes 3p and 2p, respectively [5]. In this present patient, however, it is less likely to be Muir-Torre syndrome considering her age, nonspecific familial cancer history, and symptoms that are devoid of a visceral tumor.
The primary treatment of sebaceous carcinoma is a wide excision and frozen section with a safety margin of 5 to 6 mm. Radiotherapy or chemotherapy has been the treatment of choice with postoperative care particularly when metastatis is confirmed. However, general guideline for radiotherapy and chemotherapy has not been established in this regard.
The diagnosis of sebaceous carcinoma can be difficult to make at initial presentation. Well-differentiated sebaceous carcinomas are not difficult to make a diagnosis because tumor cells have obvious cytoplasmic lipid vesicles that are characteristic of sebaceous carcinoma. But, poorly differentiated sebaceous carcinomas lack lipid vesicles and consist of predominantly basaloid tumor cells that imitate carcinomas such as basal cell carcinoma and squamous cell carcinoma [1]. Moreover, the punch biopsy only represents a small part of the lesion. It might result in a false-negative diagnosis or in missing a more severe part of the lesion. The present patient had undergone punch biopsy initially, and the result confirmed a basal cell carcinoma. However, in contrast to basal cell carcinoma, sebaceous carcinoma can be an aggressive form of cancer. Local recurrence rate after surgical excision within 5 years is found to be approximately 9% to 36% in sebaceous carcinoma and 10.1% in basal cell carcinoma. Furthermore, metastasis occurs at relatively higher rate than that observed basal cell carcinoma [1,7]. The present patient wanted only a palliative treatment so that we did not perform repetitive histological examination before the operation. Therefore, although in rare cases, if diagnosed basal cell carcinoma grows rapidly, proper evaluation is essential to assess whether sebaceous carcinoma was misdiagnosed.
This report describes a rare case of a rapidly growing extraocular sebaceous carcinoma, which resulted in a good treatment outcome of cosmetic and functional aspect, and provides a review of relevant literature.
References
1. Nelson BR, Hamlet KR, Gillard M, Railan D, Johnson TM. Sebaceous carcinoma. J Am Acad Dermatol 1995;33:1-15. PMID: 7601925.


2. Shields JA, Demirci H, Marr BP, Eagle RC Jr, Shields CL. Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol 2005;50:103-122. PMID: 15749305.


4. Dasgupta T, Wilson LD, Yu JB. A retrospective review of 1349 cases of sebaceous carcinoma. Cancer 2009;115:158-165. PMID: 18988294.


5. Dores GM, Curtis RE, Toro JR, Devesa SS, Fraumeni JF Jr. Incidence of cutaneous sebaceous carcinoma and risk of associated neoplasms: insight into Muir-Torre syndrome. Cancer 2008;113:3372-3381. PMID: 18932259.



6. King DT, Hirose FM, Gurevitch AW. Sebaceous carcinoma of the skin with visceral metastases. Arch Dermatol 1979;115:862-863. PMID: 453897.


7. Levi F, Randimbison L, Maspoli M, Te VC, La Vecchia C. High incidence of second basal cell skin cancers. Int J Cancer 2006;119:1505-1507. PMID: 16642479.


Fig.┬Ā2
Enlarged mass with focal ulceration and yellowish discharge, 7 months after the first visit.

Fig.┬Ā4
Resulting defect after wide excision. Note the preserved facial nerve branch (yellow arrow).
- TOOLS
-
METRICS

-
- 4 Crossref
- Scopus
- 3,740 View
- 59 Download
- Related articles in ACFS
-
A recurrent case of extraocular sebaceous carcinoma with distant organ metastasis2021 February;22(1)
A Case of Scalp Angiosarcoma.2002 April;3(1)
A Case of Malignant Proliferating Trichilemmal Tumor with Spindle Cell Carcinoma.2005 April;6(1)











