INTRODUCTION
The primary goal of treating cleft lip and palate is to close the cleft area without developmental restrictions. Presurgical orthopedic devices and early lip adhesion are used to hold the abnormal maxillary dental arch and to facilitate the cleft lip repair. These methods are known to be effective in infants with a cleft palate and protruding premaxilla. However, only a few studies have investigated the effect of nasoalveolar molding (NAM) devices on the treatment of protruding maxilla in infants with cleft lip only. Reported herein are three cases of wide cleft lip and alveolar cleft patients with premaxilla protrusion of 1 cm or more from the lateral segment. The patients were successfully treated with lip adhesion and NAM devices, and the purpose of this study was to highlight the efficacy of the early complex correction as a way to prevent the progression of nasal deformation.
CASE REPORT
The study included three infants who had complete cleft lip with alveolar cleft and without cleft palate. All of the infants had premaxillar protrusion of 1 cm or more.
Infant 1 was born with left complete clefts of the primary palate without involvement of the secondary palate. She did not undergo any preoperative correction, and underwent primary cheiloplasty with Millard rotation at six months after birth.
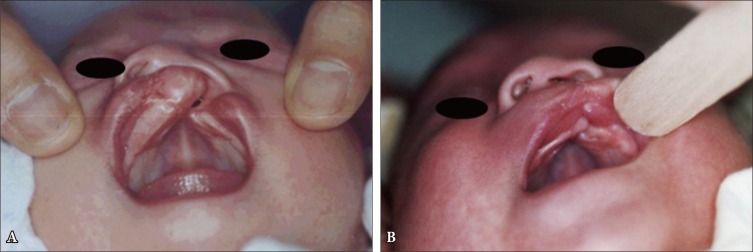
Infants 2 and 3 had bilateral cleft lip and left complete cleft lip, respectively. Alginate impressions were obtained prior to early lip adhesion at three weeks after birth. The NAM device included an intraoral molding acrylic palatal plate and nasal stent (
Fig. 1) and was used immediately after the adhesion for a total duration of 5 months. Definitive cheiloplasty was performed with Millard rotation at six months.
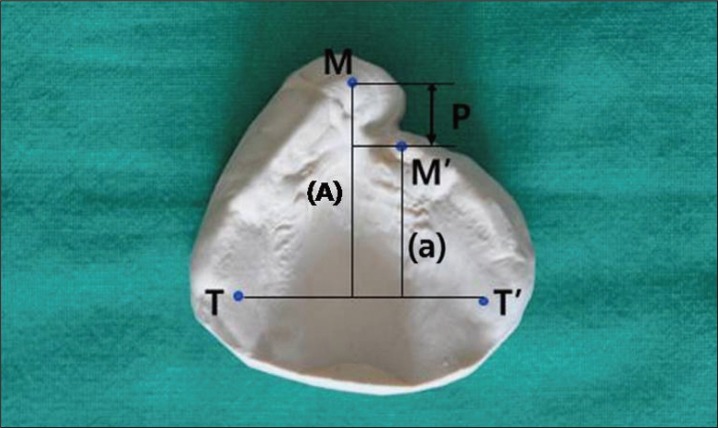
Measurements from cast models and actual measurements were obtained before and three months after chelioplasty (6 months and 9 months after birth, respectively). Protrusion was evaluated using the anterior-posterior length of the premaxilla (
Fig. 2). Columella length was measured between the superiormedial point along the inner medial surface to philtral upper margin. To prevent human error, reading were repeated and mean difference was taken to prevent bias.
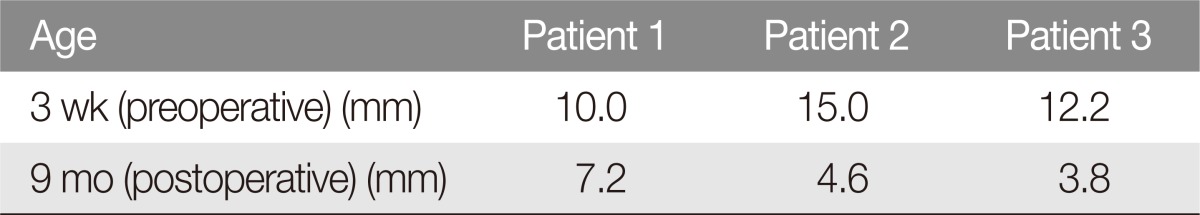
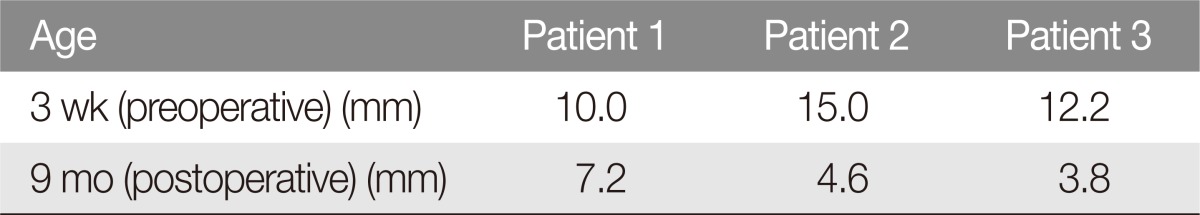
The preoperative premaxillar protrusion were 10.0 mm, 15 mm, and 12.2 mm for infant 1, 2, and 3 (mean 12.4 mm). Repeat measurements revealed 7.2 mm, 4.6 mm, and 3.8 mm of protrusion for the three infants, respectively, at 3 months after chelioplasty (mean 5.2 mm) (Table 1).
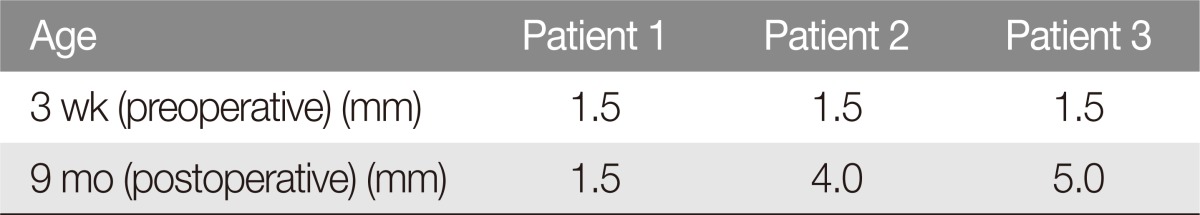
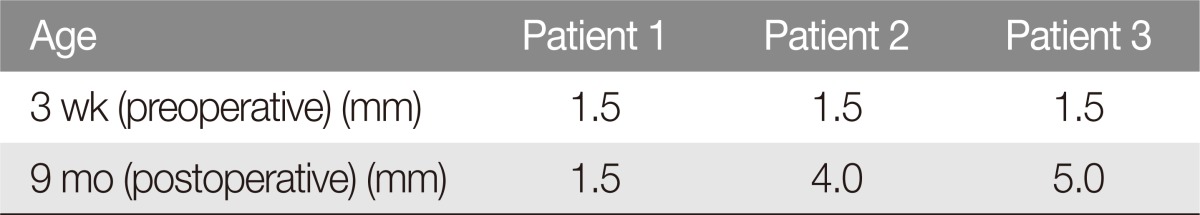
For infant 1, columella length was 1.5 mm at both preoperative and postoperative measurements. For infant 2 and infant 3, the columella length increased from 1.5 mm for both to 4 mm and 5 mm, respectively (Table 2).
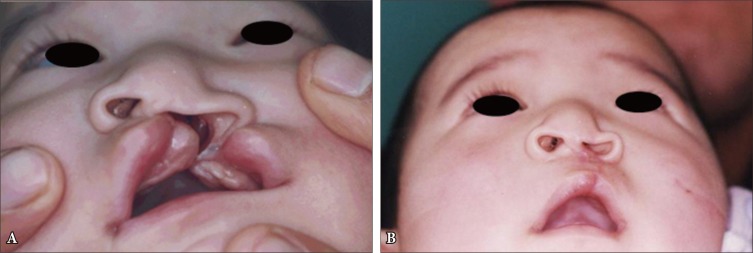
This result indicates that the combination treatment decreased the gap between alveolar cleft and the protrusion level and increased columella length. infant 1 did not show any improvement in nostril asymmetry nor alar dome depression during the followup period (
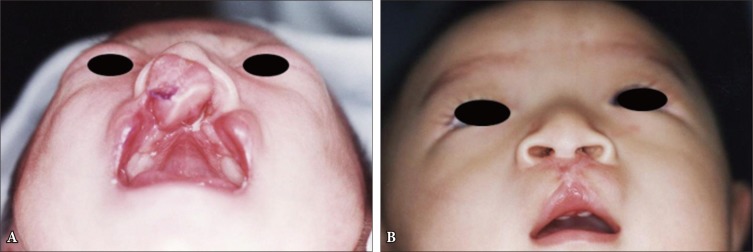
Fig. 3). In contrast, infant 2 and 3 showed alar dome elevation and improved nostril symmetry (
Figs. 4,
5).
DISCUSSION
Despite the efforts of plastic surgeons, no satisfactory postoperative result has been reported in cases of a wide cleft lip width, bilateral clefts, and non-horizontal alveolar bone ends [
1]. Samuel and Melvin [
2] defined a wide cleft lip as a cleft lip that is at least 10 mm wide. Hurwitz [
3] defined alveolar bone collapse as 3 mm-wide or wider alveolar ends, or depression of the lateral alveolar bone compared with the medial alveolar bone. Regarding the methods of treating wide cleft lip, Millard et al. [
4] performed lip adhesion to transform complete cleft lip to incomplete form and reported positive outcome during definitive cheiloplasty. This procedure can reduce lip tension and alleviate the extent of lip and nasal deformation. By suturing abnormally positioned orbicularis oris muscle and upper cleft lip back to the normal position, the uneffected maxillary lateral segment is prevented from protruding in unilateral cleft cases and checks progression of premaxilla protrusion in bilateral cases. When lip adhesion is performed for severe premaxillar protrusion, however, the lateral small segment is not addressed, and can collapse due to buccinator activity. In addition, a normal alveolar ridge contour may not be formed, and this can adversely affect dental development in growing children and increase the risk for anterior fistula [
5].
The NAM devices used in this study were introduced by Grayson et al. [
6] and have been used for cleft lip and palate cases as presurgical adjuncts. These devices are known to induce a more normal alignment of the three palate segments and lengthen the columella [
6,
7,
8]. The combination of columellar lengthening and repositioning with nostril lengthening helps to improve the nasal symmetry [
9]. However, the use of this device alone was insufficient for molding when the normal-side maxillary alveolar segment was severely displaced anteriolaterally. Although lip adhesion requires additional surgery and leaves untoward scarring, it may be needed to rearrange the orbicularis oris muscle and compress displaced alveolar segment for better outcome [
10,
11]. Many studies have reported synergic effects between NAM device and lip adhesion in complete primary and secondary cleft patients [
11,
12,
13].
In this study, we used the combination of NAM devices and lip adhesion prior to lip closure in patients with wide cleft lip without a secondary cleft palate. When compared with definitive cheiloplasty only, the combination treatment was associated with improved columella length and general nasal contour. Our observation is consistent with prior reports on outcomes following the combination treatment in patients with complete primary and secondary cleft palate. Nevertheless, additional studies are needed to obtain a sample population large enough to demonstrate any statistical differences in outcome.
Fig.┬Ā1
The device for presurgical nasoalveolar molding. It included an intraoral molding acrylic palatal plate and nasal stent. The stent had a spherical soft resin molding ball attached to the intraoral palatal plate with 0.036 inch diameter wire.

Fig.┬Ā2
Measurement of dental cast: M, most anterior point of the noncleft side maxilla on the gingival ridge of the cleft; M', most anterior point of the cleft side maxilla on the gingival ridge of the cleft; T, maxillary tuberosity of the major segment; T', maxillary tuberosity of the minor segment. The degree of protruding premaxilla (P)=distance (A) of point M and line TT'-distance (a) of point M' and line TT'.
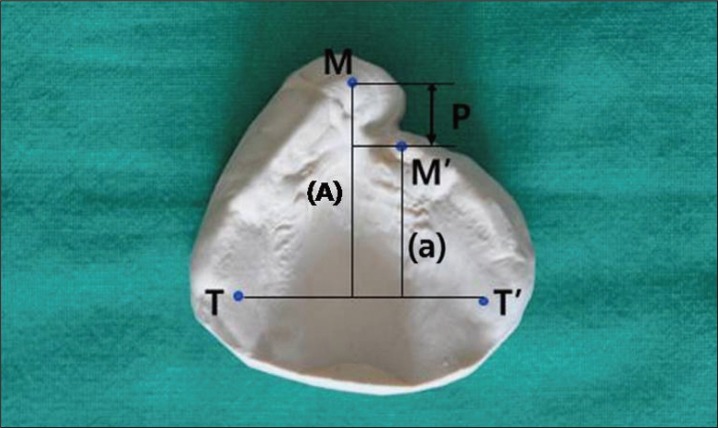
Fig.┬Ā3
Case 1. Photographs of unilateral cleft lip infant. (A) Preoperative view of 87-day-old baby. Protruding premaxilla and slightly deviated columella were seen. (B) Postoperative view on 9 month-old baby following cheiloplasty. There is no columella lengthening and asymmetric nostril and depressed alar contour was seen.
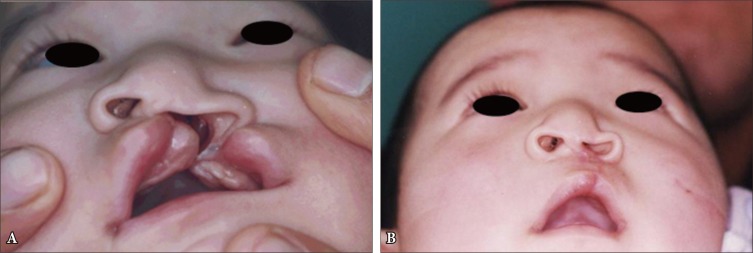
Fig.┬Ā4
Case 2. Photographs of bilateral cleft lip infant. (A) Three weeks of age prior to lip adhesion and nasoalveolar molding appliance therapy. (B) At 12 month of age of the same patient. Realigngment of premaxilla to lateral segments, columellar lengthening and improved alar dome contour was noted.
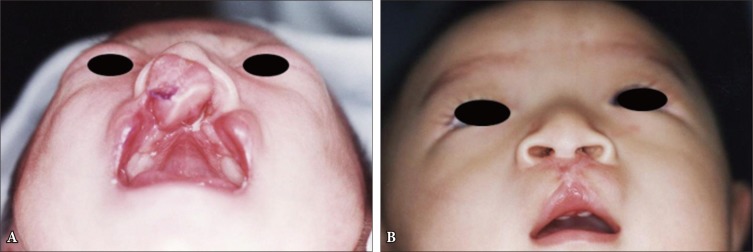
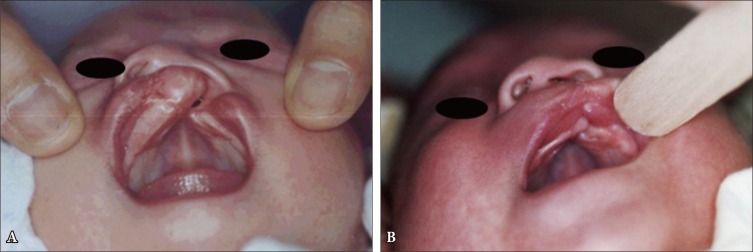
Fig.┬Ā5
Case 3. (A) Preoperative view of 20-day-old baby with complete unilateral cleft lip and protruding premaxilla, which presents outward rotation of the major segment and a posterior positioning of the minor segment. (B) Postoperative view on 168 days following the nasoalveolar molding device and lip adhesion. The alignment of maxillary alveolar arch is improved.
Table┬Ā1
Results: dental cast measurement of the degree of protruding premaxilla
Table┬Ā2
Results: actual measurement of columella length