A Giant Keratoacanthoma Treated with Surgical Excision
Article information
Abstract
A keratoacanthoma is a rapidly growing cutaneous tumor that spontaneously involutes in most instances. A giant keratoacanthoma is a rare variant and are characterized by lesions larger than 20 mm in diameter. We report a 56-year-old man with a rapidly growing tumor of the right cheek, which was diagnosed as keratoacanthoma. The mass was excised completely under general anesthesia, followed by Limberg flap for reconstruction. Intraoperative frozen section histology suggested the lesion to be a well-differentiated squamous cell carcinoma, whereas final histopathology was consistent with keratoacanthoma. We herein report the first case of a giant keratoacanthoma treated with surgical excision in Korea and discuss the clinical and histopathological features of keratoacanthoma, with a review of the literature.
INTRODUCTION
A keratoacanthoma is a rapidly growing cutaneous tumor that spontaneously involutes in most instances. The classic lesion reaches full size of 10 to 25 mm within 6 to 10 weeks, followed by spontaneous regression within 6 months. A giant keratoacanthoma is a rare variant and are characterized by lesions larger than 20 mm in diameter [123].
To the best of our knowledge, only 5 cases of giant keratoacanthoma have been reported in Korea, all of which were treated with intralesional injection [4567]. We herein report the first case of a giant keratoacanthoma treated with surgical excision.
CASE REPORT
A previously healthy 56-year-old man presented with a rapidly growing exophytic tumor on the right cheek. The patient first noticed the lesion four weeks prior. There was no history of trauma or no significant past medical history. Physical examination revealed a well-demarcated, dome-shaped, 2.7×2.7 cm cutaneous tumor with a central crater (Fig. 1). There was no evidence of regional lymphadenopathy. The remainder of physical examination and all preoperative laboratory tests were unremarkable.

Clinical presentation. This otherwise healthy 56-year-old patient presented with the mass, which had grown over just four weeks prior to this photograph was taken.
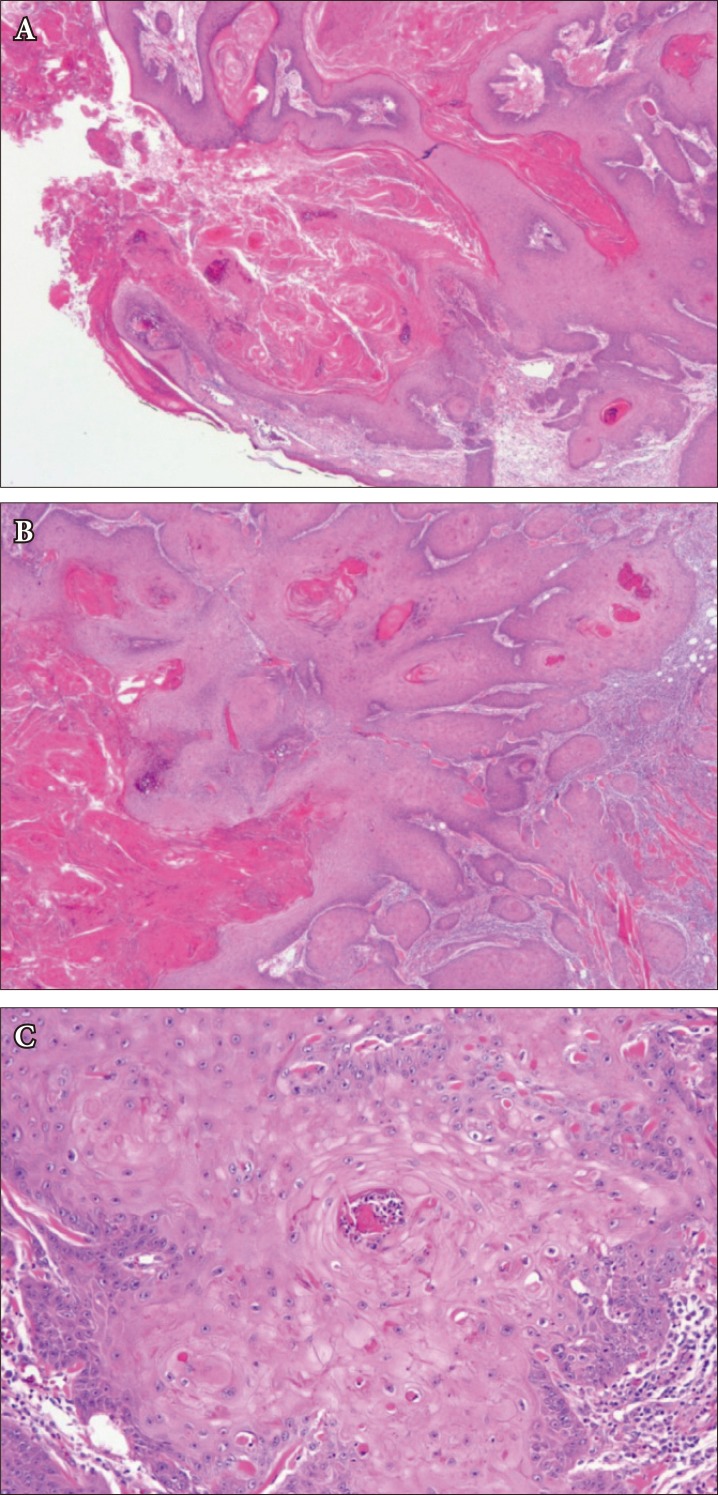
Two weeks later, the mass was excised completely under general anesthesia (Fig. 2A, C). Intraoperative frozen biopsy of the margin was suggestive of well-differentiated squamous cell carcinoma (SCC). Because of this, an additional margin of 4 mm was resected. The resulting defect was resurfaced with a Limberg flap (Fig. 2B, D). The wound healed without any significant vascular issues in the flap. However, unlike intraoperative frozen section histology, final histopathology was consistent with keratoacanthoma (Fig. 3). The patient was discharged home at 5 days. During the follow-up period, the patient showed satisfactory progress from both aesthetic and functional perspectives.
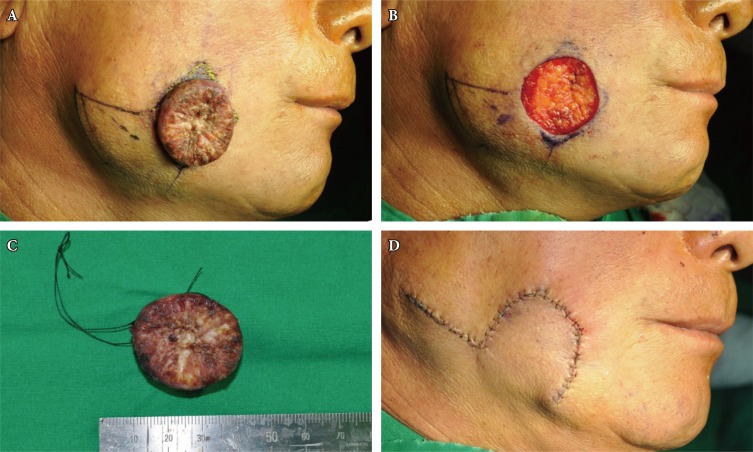
(A) Preoperative planning included excision and Limberg flap reconstruction. (B) The mass was excised, leaving a 3.0 diameter soft tissue defect. (C) Intraoperative frozen section of the wound margin was suggestive of squamous cell carcinoma, and an additional 4-mm margin was further resected. (D) The resulting defect was closed with the flap.
DISCUSSION
Keratoacanthomas are common but unique tumors with a rapid growth rate. Clinically, keratoacanthomas tend to be solitary tumors appearing mainly on sun-exposed areas in persons of light complexion, with the majority appearing on the face, forearms, or hands. Peak incidence is usually in the fifth decade of life. In general, there are three distinct stages in the natural history of a keratoacanthoma: proliferative, mature, and resolving. The classic lesion shows rapid progression and usually reaches full size within 6 to 10 weeks during the proliferating period. This is followed by an involution phase, which may occur after a few months and eventually results in a slightly depressed and often hypopigmented scar [128]. The entire cycle from proliferation to spontaneous involution usually takes about 4 to 6 months. However, certain lesions may last a year or more [2].
Multiple treatment modalities have been employed for keratoacanthoma: surgical excision, Mohs' micrographic surgery, curettage and electrodesiccation, cryosurgery, argon laser, radiotherapy, topical medication, and intralesional injection [12].
Clinically, keratoacanthomas can be recognized by the distinctive appearance of the rapidly growing, raised, non-pigmented lesion with a central keratin plug. This presentation shares similarity with rapidly growing atypical SCC, with the most significant difference in spontaneous resolution of keratoacanthoma [9]. Both keratoacanthoma and invasive SCC are common keratinocytic neoplasms. However, keratoacanthomas rarely spread via lymphatic, venous, or perineural routes [101112]. It is important to note that keratoacanthoma has been found in close proximity to SCC, which suggests that a keratoacanthoma cannot be reliably distinguished from SCC on histopathologic examination [913].
Management of keratoacanthoma leaves surgeons with a clinical dilemma. Some keratoacanthomas may show spontaneous regression within several months, which has prompted some surgeons to advocate an observational stance [2]. Furthermore, surgical excision of a giant keratoacanthoma in complicated anatomic locations may require extensive surgical reconstruction with significant morbidity [14]. Despite these factors, giant keratoacanthomas often do not spontenaeously resolve and tend not to respond to intralesional injections with cytotoxic agents. As such, surgical excisions are usually reserved for the larger lesion [15].
A major challenge in management of these tumors is the difficulty in histologic and clinical differential diagnosis with regard to SCC [1]. Macroscopic and histological examinations are very important for establishment of the proper diagnosis and management, especially for larger tumors similar to the case presented. Awareness of the possible malignant transformation of a keratoacanthoma is important, and the patient's history, clinical finding, and histopathology must be correlated to avoid further complications.
Notes
No potential conflict of interest relevant to this article was reported.