Recurrent Extranodal NK/T-Cell Lymphoma Presenting as a Perforating Palatal Ulcer and Oro-Nasal Fistula
Article information
Abstract
Nasal-type extranodal natural killer/T-cell lymphoma (ENKTL) is a rare disease presenting with non-specific symptoms, typically originating in the nasal cavity, palate, or midfacial region. Oral cavity is an extremely rare site for this type of lymphoma. In this report, we present a case of palatal perforation and oro-nasal fistula as a manifestation of recurrent ENKTL. Complicated disease entity should be considered when surgeons deal with palatal perforation and oro-nasal fistula.
INTRODUCTION
Palatal perforation is a rare condition that can be caused by congenital or acquired reasons. Acquired perforations can result from multiple etiologies, including developmental disorders, infections, malignancy, and drug abuse. Extranodal natural killer/T-cell lymphoma (ENKTL) represents a rare malignant entity, characterized by progressive destruction of the affected tissues. Typically, this type of lymphoma originates in the nasal cavity, the palate, or midfacial region. As oral cavity involvement is extremely rare, ENKTL can be misdiagnosed, or the diagnosis could be delayed. Here, we present a case of palatal perforation and fistula due to nasal-type extranodal NK/T-cell lymphoma.
CASE REPORT
A 37-year-old man presented to the otolaryngology department with a 2-year history of nasal stuffiness and purulent rhinorrhea. The patient denied any systemic symptoms such as fever, chills, or weight loss. Nasal endoscopy revealed hypertrophied inferior turbinates with surface ulcerating lesion on both nasal cavity (Fig. 1). A computed tomography (CT) scan of the paranasal sinuses demonstrated mucosal thickening in the left maxillary sinus and incomplete obstructions of both nasal cavities with hypertrophied conchae (Fig. 2). Multiple biopsies of the lesions confirmed nasaltype ENKTL for both nasal cavity and maxillary sinus. Staging work-up revealed the lymphoma to be Ann Arbor stage IIE. The patient was treated with 6 cycle of weekly cisplatin and radiotherapy (5,000 cGy in total), followed by 3 cycle of etoposide, ifosfamide, cisplatin, and dexamethasone (VIPD). The lymphoma showed complete metabolic response after the completion of concomitant chemoradiation therapy (CCRT) and VIPD chemotherapy.

Computed tomography images of the midface reveals mucosal thickening in the left maxillary sinus and incomplete obstructions of both nasal cavities with hypertrophied conchae.
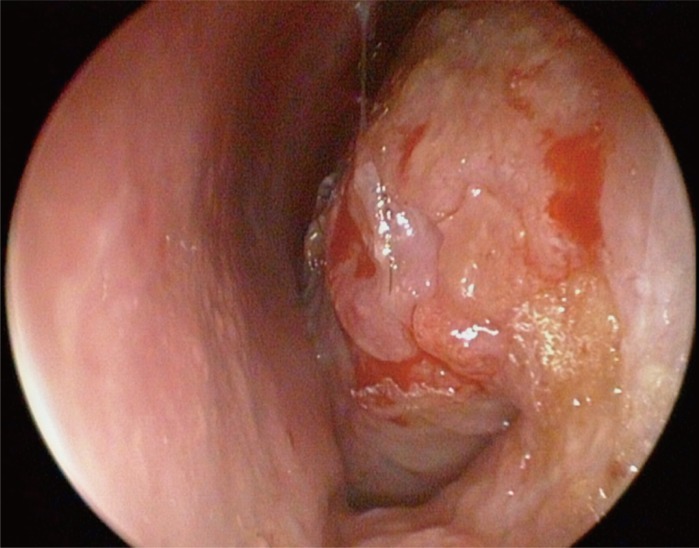
Nasal endoscopic examination reveals hypertrophic turbinate with minimal mucosa ulceration and bleeding in left nasal cavity.
Unfortunately, the patient presented again at 4 years after the initial treatment, complaining of liquid regurgitation through the nares. Physical examination revealed a 1.5 cm×1.5 cm ulcer with whitish discharge on the roof of hard palate. Nasal endoscopy showed perforation of the nasal cavity floor, demonstrating oronasal fistula and moderate perforation of the nasal septum cartilage (Fig. 3). A repeat CT scan demonstrated increased infiltrative enhancing of soft tissue at nasal vestibule and nasal septum and also increased diffuse enhancing wall thickening of nasopharynx. Biopsy of the palatal ulcer and positron emission tomography-CT revealed local relapse of ENKTL (Fig. 4). A removable partial denture with obturator was fabricated and applied to relieve the symptom of regurgitation of food and fluids into the nasal cavity caused by the oro-nasal fistula. Now, the patient is satisfied with the treatment and gets chemotherapy.
DISCUSSION
There are a variety of causes for destruction of palate and adjacent areas including multiple inflammatory and infective agents, collagen vascular diseases, malignant lymphoma, carcinoma, and drug abuse [1]. Diagnosing the underlying cause could be very challenging and requires consideration of several factors as well as gram stain, fungal stain, culture, histopathologic, and immunophenotypic examination of biopsy specimen.
Nasal type extranodal NK/T-cell lymphoma is a very rare kind of lymphoma characterized by strong association with Epstein-Barr virus (EBV) infection, with very aggressive clinical entity, high relapse rate and poor prognosis. Infections by EBV has been associated with a variety of lymphoproliferative disorders including B-cell, T-cell neoplasms, Hodgkin lymphoma, and NK-cell lymphomas [2]. Also characterized by ethnic preponderance, ENKTL is very rare in North America and Europe but rather common in East Asia and South America. A possible explanation for this geographic variation is the exposure to EBV at an early age in parts of the world where nasal NK/T-cell lymphoma is more prevalent. ENKTL affects males more commonly than females and has a median age of onset of 53 years [34].
The specifying description of 'nasal-type' is used to emphasize the predominant but not exclusive site of involvement. Other sites of spreading include maxillary sinus, nasopharynx, oropharynx, palate, oral cavity, hypopharynx and tonsils; however, ENKTL may also affect other sites, such as skin, gastrointestinal tract, larynx, testicles, liver, and spleen [5].
Presenting symptoms of ENKTL are non-specific and include pain, nasal stuffiness, discharge, foul smelling and bleeding, which can be misdiagnosed as sinusitis [6]. These symptoms usually predate ulceration and local destruction by months to years [6], as was the case in our patient. These tumors often present intranasally, and progression of the disease may lead to septal perforation and result in destruction of the hard palate. Whenever a male patient of Asian ethnicity presents with a persistent ulcerative and necrotic lesion involving the nasal and oropharyngeal mucosa, multiple biopsies are necessary for immunohistochemical typing, preferably performed on unfixed, fresh tissue of adequate sample size.
Previously, Wu et al. [3] reported a misdiagnosis rate of 44% in a clinical study of 115 patients with extranodal NK/T cell lymphomas. In 22.5% of these cases, three or more biopsies were needed to reach the correct diagnosis. Possible explanations for the difficulties in obtaining the microscopic diagnosis include the lymphoma's tendency for angioinvasion and angiodestruction, causing vascular occlusion, massive tissue necrosis and secondary infections, such that collection of adequate tumor tissue becomes challenging [7]. Therefore, multiple biopsies are advised for confirmation when a neoplastic process is clinically suspected.
Staging of the disease is similar to non-Hodgkin's lymphomas and is based on peripheral blood count and smear, liver function test, chest radiography, and CT scans of the skull, chest and abdomen. Renal ultrasound, bone marrow biopsy, and bone scan may also be needed [8].
Today, there is a lack of consensus regarding the optimal treatment for extranodal nasal-type NK/T-cell lymphoma. Treatments for this type of lymphoma include chemotherapy and radiotherapy, either alone or in combination, depending on the extent of disease. The main stay of treatment is the combination of locoregional radiotherapy and CHOP chemotherapy. The reported 5-year overall survival figures range from 10% to 60%, and the majority of the progression, presenting as locoregional and distant relapse, occurs within 2 years [9]. Recurrent NK/T-cell lymphoma presents higher locoregional failure and poorer prognosis, compared with localized lymphoma [10].
Therefore, the role of surgery is limited in the provision of biopsy material and tumor debulking for functional purposes [3]. In the case of oro-nasal fistulas/defects, an obturator can be fabricated and inserted to relieve the problem of regurgitation of food and fluids into the nasal cavity, improving speech, food intake, and quality of life. Coverage of the palatal defect could be considered in the early stage patient with relatively small oro-nasal fistula. The timing of palatal fistula coverage should be determined with careful consideration of wound healing failure and remission status.
Notes
No potential conflict of interest relevant to this article was reported.

