INTRODUCTION
Temporal hollowing commonly occurs after coronal approach craniofacial surgery. This deformity may be caused by lateral displacement of the zygoma, disinsertion or volume decrease of the temporalis muscle, or displacement and atrophy of the superficial temporal fat pad [1]. However, cryptogenic temporal hollowing unrelated to nerve damage or traumaŌĆöincluding surgeryŌĆöhas not been reported in medical literature. We encountered a case of cryptogenic temporal hollowing in a patient without a history of trauma in the temple region or of craniofacial surgery. Herein we report our case and provide a relevant literature review.
CASE REPORT
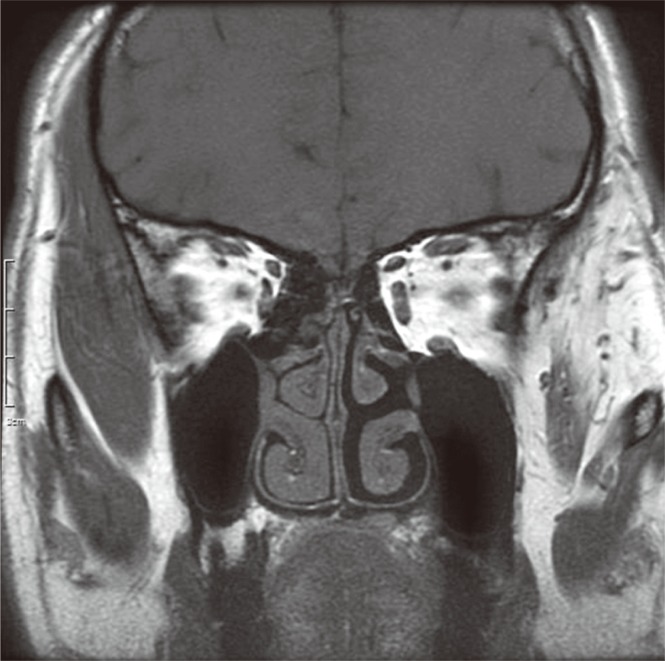
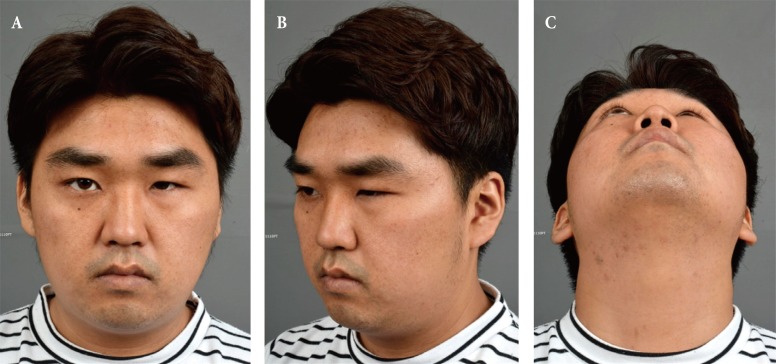
A 22-year-old man presented with a chief complaint of a one-year history of left temporal depression (Fig. 1). The patient had no history of craniofacial interventions or trauma. On physical examination, the patient had hollowing confined to the left temporal fossa. He did not exhibit facial expression and sensory abnormalities. Magnetic resonance imaging revealed fatty degeneration of the left temporalis muscle (Fig. 2). Other bony or soft tissue abnormalities were not reported. Electromyography of the facial nerve and nerve conduction studies on the trigeminal nerve performed to investigate the cause of fatty degeneration did not reveal any abnormalities. An autologous fat injection was planned to correct the hollowing deformity. The contour lines were marked to define the concavity of the left temple (Fig. 3). Autologous fat was harvested from the left thigh using the modified Coleman technique. Through two slit incisions on hair-bearing scalp, the harvested fat was injected into the subcutaneous fat layer using 1 mL syringes. Multiple injections and vigorous massage were performed to avoid bump or nodule formation. To compensate for the expected absorption, a total of 30 mL fat was injected as overcorrection and temporal hollowing was well corrected during the four-month follow-up (Figs. 4, 5).
DISCUSSION
Temporal hollowing is defined as a depression in the temporal region, an area confined superior to the zygomatic arch and immediately posterior to the lateral orbital rim [2]. Atrophy of the superficial temporal fat padŌĆöcaused by ischemia, denervation, or displacement through dissection, disinsertion, or atrophy of the temporalis muscle caused by injury to the frontal branch of the facial nerveŌĆömay result in temporal hollowing. Disruption of the suspensory ligament of the superficial temporal fat pad, the middle and deep temporal arteries, or the zygomaticotemporal nerve can also cause temporal fat pad atrophy and temporal hollowing [2]. Coronal approach surgery is the most common cause of temporal hollowing, with a reported incidence of up to 6% [3]. Lipopenia, which results from certain medications or diseases, and zygomaticotemporal fracture can also lead to temporal hollowing. The incidence of traumatic temporal hollowing without coronal approach surgery was reported to be 6.1% [4].
Augmentation using porous hydroxyapatite or titanium mesh can be a treatment option for temporal hollowing [4,5]. It has been reported that an aesthetically improved outcome can be obtained with artificial materials, without major complications such as recurrence of hollowing, infection, and protrusion through skin. However, some patients complain about the excessive rigidity of the temporal area. Autologous fat grafts can be an option for mild to moderate temporal hollowing, which obviates the need for long incisions, longer operative times, and postoperative palpable rigidity. Although it should be repeated and overcorrected because of fat absorption, it can be done under local or general anesthesia.
In the current case, the patient developed temporal hollowing but did not have a history of trauma, surgery, or myogenic disease. Little is known about the exact pathophysiology of cryptogenic temporal hollowing, which deserves further study.