INTRODUCTION
Reconstruction of the scalp and forehead area is clinically complicated owing to the immobility of the skin and galea. For coverage of large defects, split-thickness skin graft (STSG) is the most cost-effective and reliable method, although it requires a vascularized wound bed.Subsequently, to perform an STSG over the calvarium, outer table removal is required, which can increase surgical complexity and risk.
We will describe a successful experience with single-stage reconstruction of a large defect using artificial dermis, STSG, and full-thickness skin graft (FTSG) after wide excision of a cutaneous angiosarcoma in the scalp and forehead area.
CASE REPORT
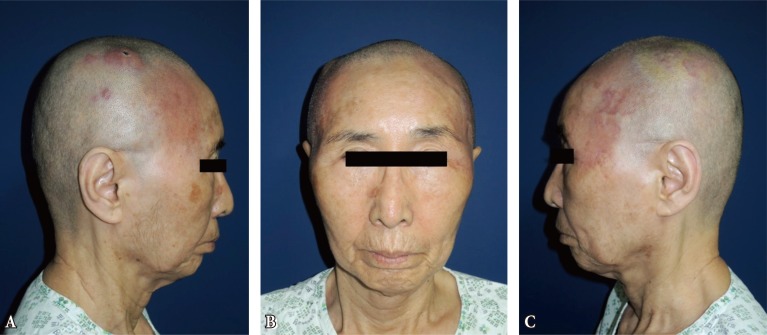
A 78-year-old woman presented with a superficial red lesion throughout the left forehead, scalp, and periorbital area (Fig. 1). She was diagnosed with angiosarcoma on biopsy. No distant metastases were identified on chest computed tomography (CT), brain magnetic resonance imaging, or positron emission tomography (PET)-CT.
Under general anesthesia, wide surgical excision was performed, including the pericranium, resulting in a near total defect of 25×20 cm (Fig. 2). First, a FTSG was applied over the periorbital area and lower forehead area. Then, micro-burring of the cortical bone was performed followed by the application of Matriderm (Medskin Solution Dr Suwelack AG, Billerbeck, Germany) and afterward, STSG coverage was applied to the remaining defect (Fig. 3). The patient was discharged from the hospital in a tumor-free state 2 weeks postoperatively with no wound complications (Fig. 4). She received radiotherapy and was seen for follow-up in the outpatient department 13 months postoperatively, at which time she reported no other complications. Much to our regret, we lost her so that we could not follow upher wound after that time.
DISCUSSION
Surgical coverage of a large scalp defect by local flap is challenging because of the inelasticity of scalp and forehead tissue [1,2]. Several types of free flaps have been used for scalp reconstruction, such as latissimus dorsi (LD), anterolateral thigh (ALT), radial forearm, rectus abdominis, or omental flap. Overall, LD or ALT flaps are preferred secondary to the large surface area and long vascular pedicle [3,4]. However, free tissue transfers require microvascular expertise and are associated with the possibility of postoperative muscle atrophy and contracture as well as the attend and risk of donor site morbidity or abnormality [2,4].
Alternatively, FTSG is associated with lower risk of contracture, but is not appropriate for large defect coverage [1]. STSG is effective for large defect coverage due to minimal donor site morbidity, but again requires a well-vascularized wound bed, and cannot be applied over bone without intact periosteum [5,6]. Therefore, two-stage reconstruction is needed. The first step involves burring the bone until there is sufficient bleeding for granulation, followed by subsequent STSG. Ultimately, STSG over bare bone requires vascularized neodermis. In these cases, artificial dermis is the preferred grafting tool [6].
Biosynthetic composites have been used in complicated wounds such as burns, and one of the popular dermal substitutes is acellular dermal matrix. Matriderm is a highly porous membrane composed of three-dimensional-coupled collagen and elastin. The collagen matrix is derived from bovine dermis, and the elastinis derived from the hydrolysis of bovine nuchal ligament. Matriderm acts as a platform for skin regeneration, assisting the dermal wound bed and supporting the development of rete ridges and capillary loops in the regenerated skin [6,7,8,9].
Over bony prominences and calvarium with an intact periosteal layer, STSG can be unstable, resulting in breakdown in these areas. Oncologic surgical defects require stable coverage because of the possibility of ulceration following radiation therapy [1,5]. In those cases, the use of artificial dermis provides stability and can reduce ulcer formation.
Angiosarcoma is a rare vascular tumor involving the endothelial cells, and cutaneous angiosarcoma is known to occur in the face and scalp area. This tumor has highly aggressive malignant characteristics including early metastasis and local regional recurrence. Standard treatment involves wide excision and radiation therapy, and typically, the periosteum is stripped to reduce local recurrence [10].
For patients with extensive angiosarcomas, wide excision and primary reconstruction alone is a burden. Furthermore, tumor margins that appear free in frozen section biopsy during surgery may in fact be revealed to be close or positive on definitive permanent section analysis, in which case, the patient will possibly require a second operation and further resection.
We propose that one-step reconstruction of an oncologic surgical scalp defect with artificial dermis and skin grafting is an excellent option over free tissue surgery or a two-stage skin graft for older patients with co-morbidities.