Rare Location of Castleman's Disease in the Temporal Region: A Case Report Involving a Young Korean Woman and Review of the Literature
Article information
Abstract
Castleman's disease (CD) is an uncommon benign lymphoproliferative disorder of unknown etiology. Histopathologically, it is divided into three types: hyaline-vascular, plasma cellular, and multicentric CD. The mass usually presents asymptomatically; however, it can cause non-specific symptoms such as fever and fatigue. Although CD can be found wherever lymph nodes are present, 75% of cases are reported in the mediastinum, and occurrence in the head and neck is rare. Herein, we report a rare case of CD presenting as a superficial mass in the temporal region. To the best of our knowledge, this is the first report of temporal CD in Korea involving a young patient.
INTRODUCTION
Castleman's disease (CD), also known as “giant lymph node hyperplasia”, “angiomatous lymphoid hamartoma”, and “angiofollicular lymph node hyperplasia” is a rare benign lymphoproliferative disorder of unknown etiology. It was first described in 1954 as a form of benign lymph node hyperplasia simulating thymoma [1]. Approximately 75% of all cases are found in the mediastinum; 15% are found in the abdomen, retroperitoneum, or pelvis; and 10% occur in the head and neck. A few isolated cases have also been described involving extra-lymphatic tissues, including the lung, larynx, parotid gland, pancreas, and muscle [2]. Herein, we present a rare case of CD presenting as a superficial mass in the temporal region. To the best of our knowledge, this is the first report of temporal CD in Korea involving a young patient.
CASE REPORT
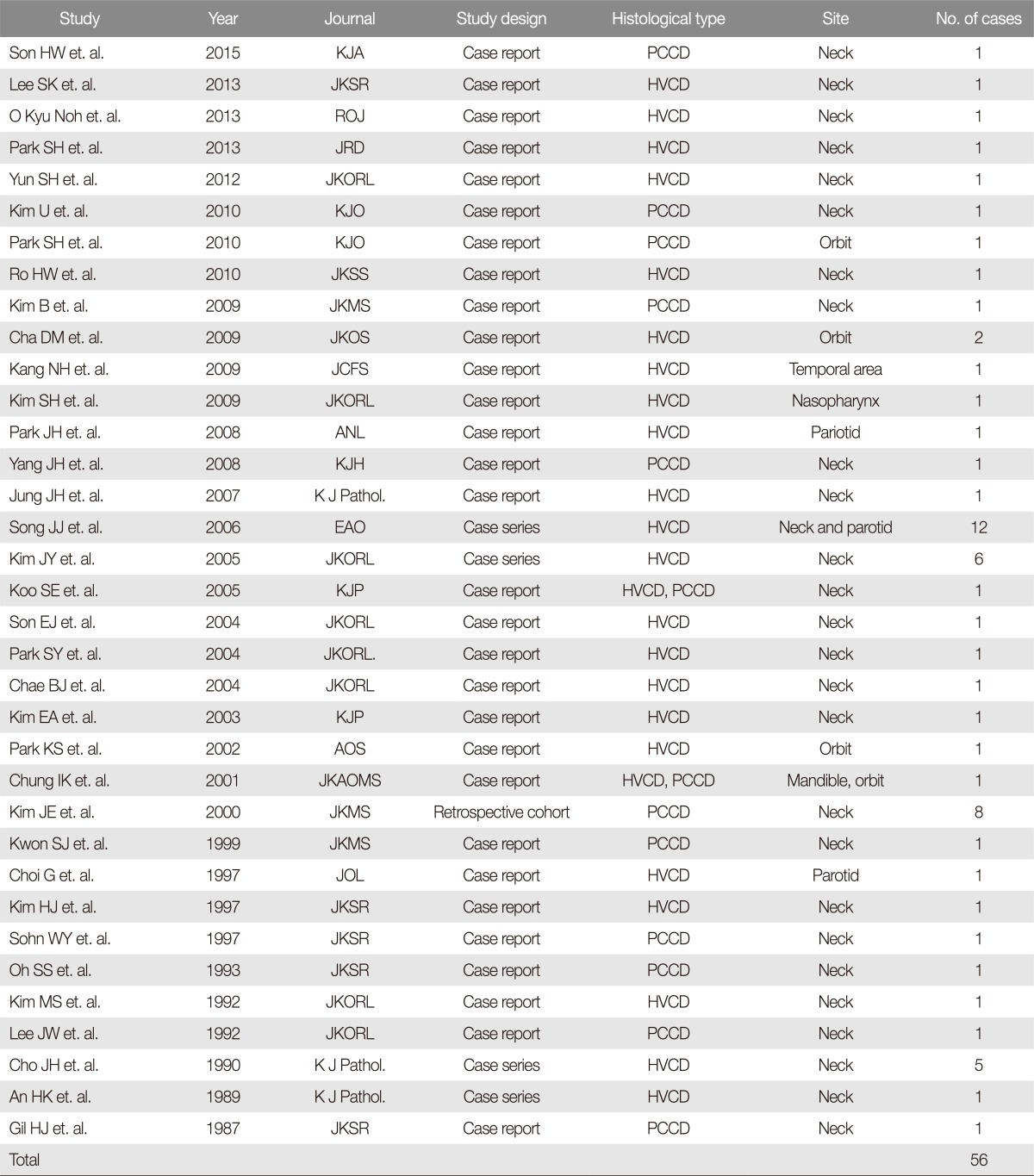
A 42-year-old Korean woman presented to our department with a slow-growing mass on her left temporal region over a duration of 1 year. The mass was approximately 2.0×1.5 cm in size, protruding, soft, and non-tender. She had no systemic symptoms such as headache, weight loss, fatigue, or fever. Contrast-enhanced computed tomography (CT) of the head and neck revealed a superficial and well-enhanced homogenous mass (Fig. 1). This lesion may be radiologically discriminated as a schwannoma, hemangioma, reactive lymph node, or lymphoma.
Preoperative computed tomography image showing an approximately 1.8×0.8 cm in size, well-demarcated mass involving the left temporal region. A well-enhanced homogenous mass in the subcutaneous area (white arrows). (A) Axial view. (B) Coronal view.
We performed an excisional biopsy based on the clinical impression of a benign superficial soft tissue mass. Following excision, a 2.1×1.5 cm-sized cavity formed. To obliterate the expected dead space, we performed a marginal de-epithelialized buried flap. The wound was closed primarily with subcutaneous and skin sutures without tension. A silastic drain was inserted to prevent hematoma; it was removed one day after the surgery (Fig. 2). No postoperative complications such as hematoma, seroma, infection, or dehiscence was reported.

Clinical photographs showing. (A) A well-circumscribed, firm, ovoid mass measuring 19×8×7 mm in dimensions. (B) The marginal de-epithelialized buried flap, which was performed to obliterate the expected dead space. (C) Tension-free primary closure with a silastic drain inserted. (D) Postoperative photograph at 3 weeks follow-up.
Histopathological examination revealed a lymph node with relatively well-preserved lymphoid architecture, showing follicles of varying sizes with atrophic and often vascularized germinal centers. The germinal centers appeared to be atrophic, with penetrating blood vessels and surrounded by a cup of small lymphocytes that were arranged in a concentric “onion skin” layer. The follicular tissues were composed of a network of vessels on a thick collagenous scaffold; sinus structures were not identified. Immunohistochemistry revealed the follicles to be positive for CD20. The mantle zone was negative for CD3 but positive for CD5. These histopathological findings corresponded with hyaline-vascular CD, which was confirmed by our senior pathologist (M.H.P.) (Fig. 3). The patient experienced no lesion recurrence at 6 months' follow-up, and reported satisfaction with the appearance of her surgical site contour and scar.

Microscopic features of Castleman's disease of the hyaline-vascular type. (A) The interfollicular areas are composed of a network of vessels (H&E, ×100). (B) Small regressed germinal centers with penetrating vessels (arrow with a tail) and onion-skin layering of the mantle cells (arrow without a tail) (H&E, ×200). (C) The germinal centers appear to be atrophic (arrow) (H&E, ×200). (D) The follicles are positive for CD20 (arrow) (immunohistochemical staining, ×100). (E) The mantle zone is negative for CD3 (arrow) (immunohistochemical staining, ×200). (F) Positivity for CD5 (arrow) (immunohistochemical staining ×100).
DISCUSSION
In 1956, Castleman et al. [1] first reported a case of “localized mediastinal lymph node hyperplasia resembling thymoma”. These lesions occur within the mediastinum, neck, axilla, pelvis, and retroperitoneum [3]. According to recent literature, the incidence rate of CD is approximately 21 persons per one million. Localized CD occurs in 15.9 persons per one million, while multicentric CD occurs in 5.1 persons per one million [4].
CD is divided into 3 subtypes: hyaline-vascular CD (HVCD), plasma cell CD (PCCD), and multicentric CD. The pathogenesis of CD is still unclear. One theory suggests that it is a result of chronic antigenic stimulation, like virus antigen, while other theories focus on nodal developmental growth disturbances. Excessive production of interleukin 6 (IL-6) by lymph node hyperplasia has been implicated in the pathogenesis of this disease. Additionally, CD has relevant human herpes virus 8 (HHV-8) or Kaposi sarcoma-associated virus, especially the multicentric type [5]. Interestingly, recent evidence indicates that excessive release of IL-6 may not only be evident in CD, but may actually underlie the pathophysiology of both localized and multicentric CDs. In earlier studies, patients with systemic symptoms and localized CD were shown to have a reduction in symptoms associated with decreased IL-6 levels following excision of the abnormal node [46].
Localized CD is often diagnosed incidentally via radiographical examination due to its asymptomatic feature. The most common histopathological type is HVCD, while 10%–20% are PCCD. The latter appears to be more closely-linked with systemic signs and symptoms such as fever, arthralgia, fatigue, anemia, thrombocytosis, and hypergammaglobulinemia [7]. The treatment of choice for localized CD is surgical excision, with a combination of radiotherapy, as required. Surgery is curative when resection is complete, yielding a 5-year survival rate close to 100%, with recurrences being infrequent. Patients without systemic involvement should have an additional radiological assessment six to twelve months after the initial therapy, to verify that there is no recurrence. Localized CD's prognosis is good [8].
Multicentric CD usually occurs as a systemic lesion. The clinical manifestations are very diverse; some rapidly-progress to death within a few weeks, while others grow relatively slowly over several years. Therefore, it is clinically important to discriminate between localized CD and multicentric CD, given the distinction in both their treatment and prognoses. Localized CD has a generally good prognosis as it can be treated with surgery and radiotherapy, with a reported 5-year overall survival of 91% [9]. Multicentric CD has a relatively worse prognosis than localized CD; its primary treatment consists of a combination of immunotherapy and chemotherapy. Recently, treatment combinations of chemotherapy with therapy targeted to CD20 (rituximab) or IL-6 receptor (tocilizumab) have been attempted [10]. The 5-year survival rate of patients with multicentric CD was reported to be 65%. Patients who present with negative prognostic factors (e.g., HIV, HHV-8, or Kaposi sarcoma-associated herpes virus) have a reported median survival of approximately 20% [9].
Furthermore, although CD is considered a benign disease of the lymph nodes, it could be associated with other disease processes. According to one literature, eight patients with localized CD were shown to have associated malignant lymphoma, six with B-cell non-Hodgkin lymphoma, and two with Hodgkin lymphoma. In addition, a minority of localized CD patients (approximately 15%) developed paraneoplastic pemphigus [11].
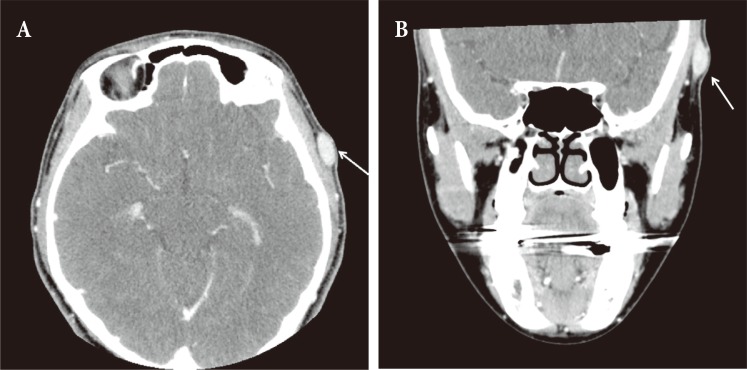
We conducted a literature review using PubMed and KoreaMed from their inception to December 31st, 2016. The search terms included “giant lymph node hyperplasia” OR “Castleman disease” AND “face” OR “neck” AND “Korea”. A total of 35 articles and 56 cases of head and neck CD were reported in Korea. Of these, 46, 4, and 3 cases involved the neck, orbit, and parotid areas, respectively, while the nasopharynx, mandible, and temporal areas were represented by 1 case each. According to our literature review, Kang et. al. [12] was the first to report a case of CD occurring in the temporal region, in a 69-year-old man. Compared to their report, our patient was a relatively young woman. In addition, we shared the gross macroscopic appearance of the specimen (Fig. 2A), and we also closed the wound with a marginal de-epithelialized buried flap, in order to obliterate the expected dead space, thus achieving a satisfactory aesthetic outcome. As mentioned earlier, while there have been several reports of CD involving the neck area in Korea, only one case of CD involving the temporal region has been reported previously. We thus believe that our report is significant in terms of CD occurring in an uncommon anatomical area, whereby the patient presented with a superficial mass in the temporal region (Table 1).
As demonstrated in our case, the diagnosis of CD may be difficult through initial clinical evaluation and imaging work-up. Therefore, plastic surgeons and pathologists should be aware of CD when presented with an asymptomatic mass. It is necessary to confirm CD through excisional biopsy and histopathological examination. Additionally, proper medical work-up and follow-up of the patient should be conducted after excision.
Notes
No potential conflict of interest relevant to this article was reported.