INTRODUCTION
Because Frey's syndrome or infra-auricular depressed deformities occurs well after total parotidectomy, the studies on the effective prevention measures for it have been actively conducted. The author obtained good results from using acellular dermal matrix (ADM) after total parotidectomy in order to prevent such complications as 1 case of pleomorphic adenoma occurred in the deep lobe and we report it with the literature review.
CASE REPORT
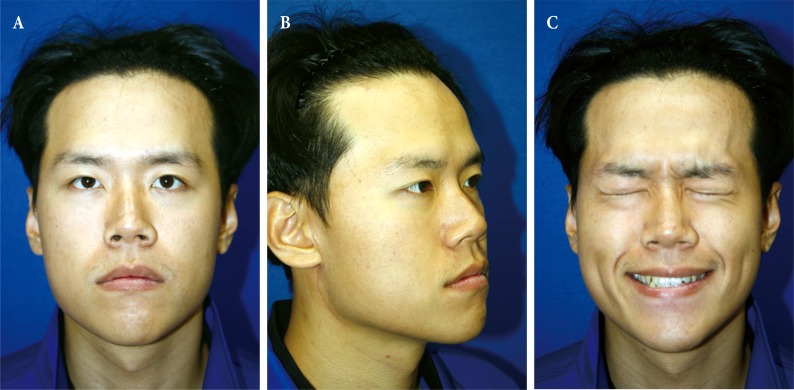
A 24-year-old man visited the hospital with oval shape mass in right mandibular angle, which had grown slowly from 3 years before the visit to the hospital as main complaint. There were no particular apparent traumas and no other medical history other than asthma. A soft mass of 5├Ś4 cm in size on physical examination was palpated, there was no presence of facial nerve weakness, and he was complaining that he felt as if the face of the affected side, was turned to ipsilateral direction (Fig. 1).
A well-defined lobulated mass of 4 cm in size was found in the deep lobe of right parotid gland from Magnetic resonance imaging (MRI) scanning and a pleomorphic adenoma was suspected (Fig. 2). We planned a total parotidectomy and decided to use the ADM to correct for the predicted depression. The mass was located at deep lobe as shown in the MRI images and a total parotidectomy was performed. 5 branches of facial nerve were identified during the surgery and all of them was preserved. The material known as ADM of 4 cm├Ś7 cm in size, 3.4 mm thickness (Flex HD, Ethicon Co. LLC., Somerville, New Jersey and Cincinnati, OH, USA) were adequately trimmed for the depressed part from where the mass was removed. The part between the cheek flap and nerve were augmented centering the depressed site after the mass was removed. After the closed draining tubes were inserted over and under the ADM, the site was sutured (Figs. 3, 4).
Drains were drained by 27 mL/day a day after surgery in bloody character, gradually became serosanguineous, and decreased in volume and drained to less than 10 mL/day 3 days after surgery, but were removed somewhat later. We removed superficial one and cut deep one to allow drainage naturally 5 days after surgery, and removed deep one 7 days after surgery. The surgery site was healed well without any complications such as seroma or infection, and mild weakness of the depressor of the lower lip was observed (House Brackmann Grade II). This symptom was completely resolved at 4 months after the surgery. Such as Frey's syndrome were not observed, there was minimal depression and the facial symmetry was well maintained, as the patient satisfaction was high (Fig. 5). The pathological result was confirmed as pleomorphic adenoma.
DISCUSSION
Pleomorphic adenoma is a most common type of parotid tumor, and usually benign, and slow growing. But it has been known for rarely malignant degeneration [1]. Likewise this case, the parotid tumor occurred in deep lobe is far rare compared to the superficial lobe, applicable to frequency of 5% of the total parotid tumor [2].
One of the most important complications of parotid surgery for pleomorphic adenoma is recurrent disease [3]. The most important causes of recurrence are incomplete tumor excision and spillage. These are associated with histologic findings for the tumor (multicentric nature, focal absence of the capsule, and the presence of pseudopods). Therefore, radical resection of the tumor is difficult. Furthermore, it is difficult to distinguish the facial nerve from scar tissue when performing reoperation for recurrent pleomorphic adenoma because of exposure during the first operation [4]. As the importance of removing the cuff surround the tumor was emphasized for several decades, superficial parotidectomy or total parotidectomy was successfully used to treat pleomorphic adenoma, and an average recurrence rate declined to below 2% [5].
Malignant and deep parotid tumors are indications for total parotidectomy [6,7]. Features predictive of malignant change include tumors which are greater than 4 cm and/or demonstrate fixity, facial nerve involvement, palpable cervical nodes, and deep lobe involvement [5]. In addition, a significant risk factor for recurrence is younger age [8]. In our case, total parotidectomy was performed because the patient was 24 years old and the mass was 4 cm and was located in the deep lobe.
Frey's syndrome and infra-auricular depressed deformities are the ones of the most common complications that can occur after total parotidectomy. For the prevention of above-mentioned two complications, a number of scholars have been trying in diversities, including Sternocleidomastoid muscle flap, temporoparietal fascia flap, the superficial musculoaponeurotic system flap, the free or vascularized dermal fat graft, and other mesh materials such as Ethisorb (Ethicon Inc., Somerville, NJ, USA) or polytetrafluoroethylene (Gore-Tex; W. L. Gore and Associates, Flagstaff, AZ, USA) [6,9].
In particular, in case of temporoparietal fascia flap, it has relatively low donor site morbidity, compared to the above-listed other surgical methods, and its effectiveness are recognized in terms that it is enough to fill the large size of defect after total parotidectomy. However, in terms that the scar remains longer than ADM, and in terms that that there is a potential of alopecia due to its locational feature, and in terms that it requires longer operating time. The disadvantage of free or vascularized grafts of fat, dermal fat is that they are easily absorbed, which result in recurrence of the original facial contour deformity. And they require additional donor sites and leave a scar [6,10,11]. Other mesh materials had the shortcoming of the greater risk of rejection than ADM [12,13]. In addition, incidence of extrusion was rather high in polytetrafluoroethylene than ADM. In case of Ethisorb, it is absorbed over time due to its resorbable properties [9,13].
ADM is derived from allograft skin, with the cellular constituents of the epithelium and dermis removed by a series of treatments. Since only type IV collagen was preserved, there is no immune response during implantation. Therefore, the possibility of rejection is low [12]. In addition to this advantage, it does not have little potential of deformation by the gravity after the surgery, and there is no restraint on circulation, which makes fabrication free and each deformation into various shapes can be described as another advantage of the reconstruction using the ADM. Therefore, ADM-utilized reconstruction was performed in this case.
Although there had been cases reported for the use of ADM in other countries to the best our knowledge, there has been no report on application to Korean. But in this case, we experienced satisfactory results without any complications such as Frey's syndrome or infra-auricular depressed deformities. Therefore, we want to add this case to the literatures related to performance of reconstruction by using other existing ADM.