|
 |
- Search
| Arch Craniofac Surg > Volume 18(4); 2017 > Article |
|
Abstract
Background
To evaluate the versatility and reach of modified nasolabial flap used in reconstruction of defects created in and around the oral cavity.
Methods
A total number of 20 cases were selected. Out of which 13 were males and 7 females. The age of these patients ranged from 24ŌĆō63 years. 29 modified nasolabial flaps were raised in twenty patients. Based on clinical and histopathological examination, out of 20 patients, 14 patients were diagnosed with oral submucous fibrosis, 3 with verrucous carcinoma, 1 with squamous papilloma, 1 with oro-antral fistula and 1 with traumatic loss of lower lip.
Results
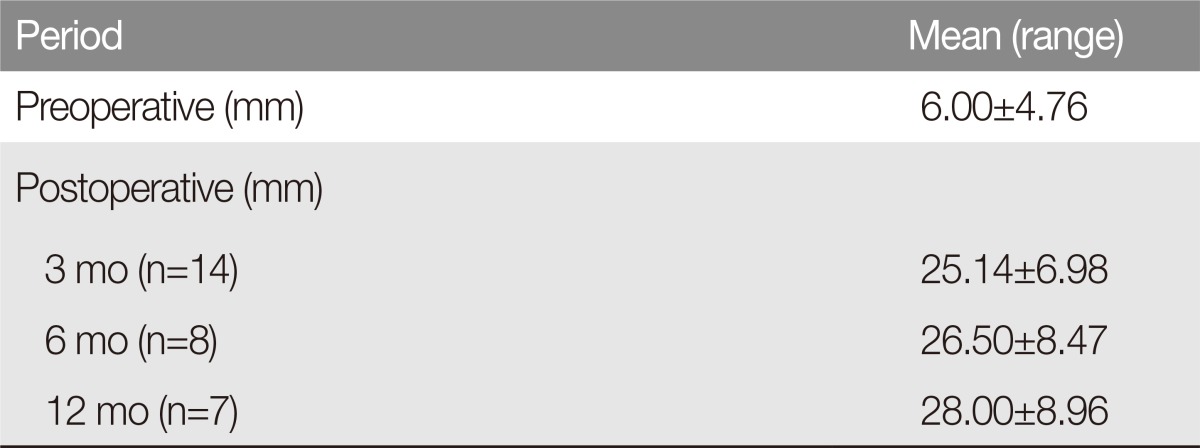
Minimum preoperative interincisal distance (IID) was 0 mm and maximum was 15 mm with mean of 6.00┬▒4.76 mm in patients with oral submucous fibrosis and 12 months postoperatively minimum IID was 16 mm and maximum was 41 mm with mean of 28.00┬▒8.96 mm. In one case, dehiscence (3.4%) was noted on the anterior tip for which tip revision was done. Bulky appearance of the flap intraorally was observed in 2 cases (6.9%). Five (17.2%) among the 29 flaps had visible scar at the donor site postoperatively up to 3 months.
Conclusion
Numerous reconstructive techniques have been employed in the reconstruction of small to intermediate sized defects of oral cavity. Modified nasolabial flap is a versatile flap which has robust vascularity and can be successfully used with minimal complications. It can be rotated intraorally to extend from the soft palate to the lip. Thus, it can be used efficiently to treat the small defects of the oral cavity as well as recreating lost lip structure.
With the advent of musculocutaneous flaps and microsurgical transfer, intraoral or nasal reconstruction has entered an area of sophistication whereby defects of any size can be repaired, however sometimes these technique are inappropriate because either the defect is too small or the patient's age and medical status do not permit a lengthy anesthetic and surgical procedure. The nasolabial flap represents the available local tissue that, in right circumstances, often circumvents these problems for repair of small or moderate sized local intra or extra-oral defect [1].
In our study, the modification that has been incorporated as a single stage flap surpasses most of the disadvantages of the classical nasolabial flap. The specificity of using this flap in addition to the robust vascularity; the flap also gives better esthetics. Modified nasolabial flap (Fig. 1) also provides supple soft tissue lining and adequate flexibility to the cheek thus facilitating excellent mouth opening on a long term basis. The goal of our study is to emphasize that this extended version of the nasolabial flap in a single surgery can be used in different ways.
We have used this flap not only to treat patients of oral submucous fibrosis but also used it in patients to line the alveolus and the lip in cases of verrucous carcinoma. We also used this flap to reconstruct three-fourth of a missing lip and in case of large oro-antral fistula. Finally, ugly scar can be prevented by careful suturing to the extent that it becomes invisible in the form of a natural nasolabial crease.
Twenty patients with intraoral and extraoral soft tissue defects resulting from trauma, precancerous conditions, tumor resection, etc. were included in this study. Based on clinical and histopathological examination, fourteen patients were diagnosed with oral submucous fibrosis, three with verrucous carcinoma, one with squamous papilloma, one with oro-antral fistula and one was a patient with traumatic loss of lower lip.
The following study variables were taken into consideration: age & sex of the patient, type & site of the defect, size of the defect and cause of the defect.
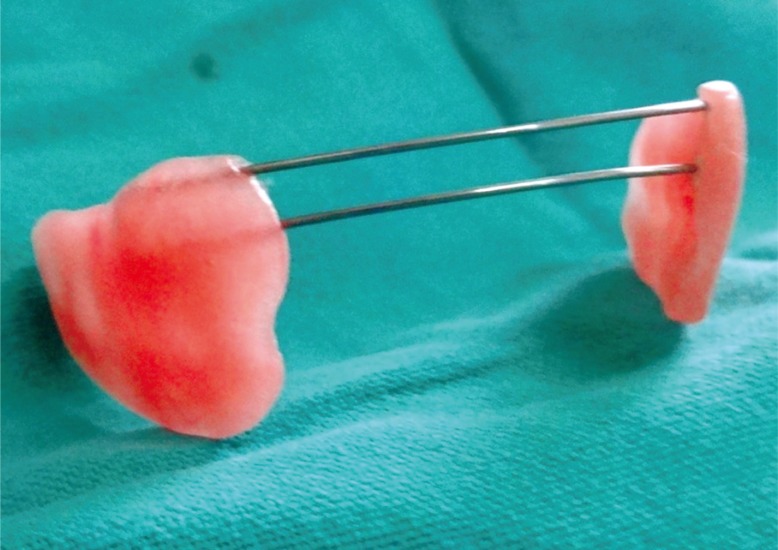
Postoperatively, functional and esthetic outcome of reconstruction of the concerned site was evaluated by clinical examination and post-treatment healing. A ŌĆ£flap protectingŌĆØ appliance was used to prevent the flaps from occlusal trauma in initial postoperative healing period of one month (Fig. 2).
In all our cases, postoperatively flap evaluation was done after 6 hours, 24 hours, 72 hours, 1 week, 3 weeks and 12 weeks and mouth opening was recorded after 1 month, 3 months, 6 months and some were even evaluated after one year.
The study was approved by Institutional Research Committee. We have taken informed consent for the procedure from every patient.
The patients were taken under general anesthesia. All aseptic precautions were followed during surgery. Post-surgical defects were reconstructed by the modified nasolabial flap (Fig. 3). Marking of the flap was done from the tip of nasolabial fold to the inferior border of mandible followed by incision. The skin incision was carried through the dermis and subcutaneous fat to the level of the underlying musculature. The artery lies in a plane deep to the facial mimetic musculature and in a medial position along the nasofacial groove. Flap was raised in the supero-inferior fashion and in the plane of the superficial musculoaponeurotic system from both terminal points to the region of the central subcutaneous pedicle which was based on facial artery (Fig. 4). The pedicle was approximately 1 cm lateral to the corner of mouth and the diameter of the pedicle was roughly 1ŌĆō1.5 cm. The flap was transposed intraorally through a small transbuccal tunnel anterior to the pedicle. The transposed flap was used to cover the full span of intraoral defects. In oral submucous fibrosis cases, the inferior wing of the flap was sutured to the anterior edge of the defect, while the superior wing was sutured to the posterior edge of the defect (Fig. 5). Suturing was done with 3-0 vicryl intraorally. The extraoral defect was closed in layers with 3-0 vicryl and 4-0 nylon.
A total number of twenty cases were selected for the study, of which thirteen were males and seven were females. The age of the patients ranged from 24ŌĆō63 years.
Interincisal distance (IID) was recorded in all patients of Oral Submucous fibrosis (n=14) preoperatively.
Minimum preoperative IID (n=14) was 0 mm and maximum was 15 mm with mean of 6.00┬▒4.76 mm in patients with oral submucous fibrosis. One month postoperatively minimum IID was 14 mm and maximum was 40 mm with mean of 23.79┬▒7.06 mm, 3 months postoperatively minimum IID was 18 mm and maximum was 40 mm with mean 25.14┬▒6.98 mm, 6 months postoperatively (n=8) minimum IID was 14 mm and maximum was 40 mm with mean of 26.50┬▒8.47 mm, 12 months postoperatively (n=7) minimum IID was 16 mm and maximum was 41 mm with mean of 28.00┬▒8.96 mm (Table 1).
Each patient was evaluated postoperatively for color of the flap, anterior and posterior tip of the flap and all margins. Color of all the flaps remained similar to that of the donor area. All margins of the flaps were well adapted and no dehiscence was seen except one case which showed wound dehiscence at anterior tip of the flap. During the early postoperative period, flap viability was checked using pin prick test which demonstrated excellent vascularity in all the flaps.
The following observations were recorded in the postoperative period.
The flap remained viable in all the cases with good healing and adaptation to the recipient site. The survival rate and adaptation of all the flaps was 100%. This local flap proved to be ideal for small to moderate sized defect of oro-facial region & also for intraoral reconstruction.
Intraoral hair growth was a commonly observed manifestation in males; they experienced mild discomfort which was managed by plucking the hair under topical anesthesia during follow-up. There was gradual reduction in hair growth and subsequent mucosalization of the flap over a period of six months to one year postoperatively.
Postoperatively, wound healing at the donor & recipient sites was satisfactory for all the patients. There were no signs of gaping, discoloration, sloughing due to vascular changes, necrosis or infection of the flap. In one case, dehiscence (3.4%) was noted on the anterior tip (left side) for which tip revision was done.
The nasolabial flap was first described in the Sushruta Samhita text in 600 AD as a means of correcting cutaneous defects [2]. Contemporary surgical descriptions began in 1830 when Dieffenbach used superiorly based nasolabial flaps to reconstruct nasal alae [3].
The inferiorly based nasolabial flap has been described for reconstruction of the floor of the mouth, lips, tongue, buccal mucosa, upper and. lower alveolus, maxilla, and oro-nasal defects. Various authors described its use for reconstruction of defects resulting from different pathologies, but they encountered various complications like oro-cutaneous fistula [4], bulkiness of the flap [5] and delayed healing [6]. This flap also requires a two stage surgery and the available flap tissue for reconstruction is half of what is available in the modified nasolabial flap.
Singh et al. [7] performed a retrospective analysis of 26 cases of oral cancer treated with primary excision and nasolabial flap reconstruction was carried out. A primary tumor was located in the buccal mucosa, the alveolus, the tip of the tongue, the commissure and lip. They concluded that the nasolabial flap is versatile for covering or reconstructing small or medium-sized defects of the oral cavity in selected patients. The nasolabial flap is a good flap for the reconstruction of small oral defects after excision of primary tumors and results in good overall cosmetic and functional outcome.
The modification that has been incorporated as a single stage flap surpasses most of the disadvantages of the inferiorly based nasolabial flap and therefore, in our study it has become preferred design of nasolabial flap. The advantages of using this flap in addition to the robust vascularity; the flap also gives better esthetics. In cases of oral submucous fibrosis (OSMF) achieving and maintaining a satisfactory mouth opening is of prime importance. In the year 2009, Tauro [8] conducted a study ŌĆ£A unique melolabial flap in the surgical management of oral submucous fibrosisŌĆōŌĆ£the seagull flapŌĆØŌĆōan experience with 85 casesŌĆØ, one hundred and seventy flaps were performed in 85 patients with bilateral submucous fibrosis in the span of ten years from 1999ŌĆō2009. The flap was referred as ŌĆ£sea-gull nasolabial flapŌĆØ which offers outstanding features, providing supple soft tissue lining and adequate flexibility to the cheek.
Borle et al. [9] conducted a study in which the OSMF patients were treated by bilateral release of fibrous bands & coronoidectomy or coronoidotomy. They reported that the interincisal opening improved significantly from a mean of 14 mm (range, 3ŌĆō23 mm) to a mean of 41 mm (range, 23ŌĆō55 mm). A soft temporomandibular joint trainer was placed postoperatively in the oral cavity for 10 days to prevent dehiscence of the flap as a result of occlusal trauma. Similarly, in our study there was gradual increase in mouth opening from a mean of 25.14┬▒6.98 to 28.00┬▒8.96 mm at the end of one year. This study showed a significant improvement in mouth opening, the maximum being 41 mm. It is also to be noted that in our case series, no coronoidectomy, coronoidotomy or myotomy were performed to achieve the mouth opening. In our study, physiotherapy was started after a latent period of 10 days. Patients were instructed and motivated to continue the physiotherapy themselves with wooden spatulas followed by Heister's jaw exerciser to prevent contractures and relapse.
In the year 2011, Agarwal et al. [10] performed a study to evaluate the use of extended nasolabial flaps in the management of oral submucous fibrosis in which they encountered intraoral hair growth in men. Likewise, in our case series intraoral hair growth was a common manifestation postoperatively in males which was gradually reduced over a period of one year.
Verrucous carcinoma (VC) was defined by Ackerman [11] in 1948 as a diagnostically problematic squamous cell neoplasia involving lip, oropharyngeal, and laryngeal mucosa. As a result, this neoplasm was named as ŌĆ£Ackerman's tumorŌĆØ. VC is strongly associated with the chronic use of tobacco or with the practice of chewing betel nuts. Treatment modalities for verrucous lesions have included surgery, radiation therapy, chemotherapy, cryotherapy, laser therapy, photodynamic therapy, and treatment with recombinant alphaŌĆōinterferon. Surgical excision remains the preferred treatment for the primary lesion followed by reconstruction with split skin graft, local flaps, cheek flap, fasciocutaneous free flaps either anterolateral thigh or radial artery forearm flap can be used [12].
A surgical excision with wide margins and an appropriate reconstruction is necessary to optimize the disease and functional outcome. We have used modified nasolabial flap to line the alveolus and lip in cases of VC.
Traumatic lesions of the lip are also common etiologies requiring reconstructive surgery. Frequently, gunshot wounds or motor vehicle accidents result in defects that affect functioning and aesthetic appearance of the lips. These injuries often require total or subtotal repair. The main goals of reconstruction remain the restoration of oral competence, the maintenance of oral opening, and the restoration of normal anatomic relations so that both the active (smile) and passive (form) cosmetic outcome is acceptable.
Small, full-thickness defects involving approximately one fourth to one third of the lip can usually be managed by primary closure. In some cases the size of the defect makes it necessary to use myocutaneous or free flap by microvascular technique. If the defect involves 1/3ŌĆō2/3 of the lip, it can be managed by a cross-lip flap, like Abb├®'s or Estlander, circular rotational flap, such as Karapandzic or Gillies, nasolabial flap or the Kazanjian reverse flap [13].
We have used this flap for reconstruction of lower lip that was lost due to trauma, the defect spanned three-fourth of the lower lip. Flap survived well and we have achieved good lip seal and good function in speaking. It is an useful adjunct in recreating lost lip structure.
References
1. Deora SS, Nanjappa M, Kumaraswamy SV. Bilateral pedicled nasolabial flaps for the anterior alveolus mandibular defect: a review. J Maxillofac Oral Surg 2010;9:385-388. PMID: 22190830.


2. Pers M. Cheek flaps in partial rhinoplasty: a new variation: the in-and-out flap. Scand J Plast Reconstr Surg 1967;1:37-44.

3. Cormack GC, Lamberty BG. The arterial anatomy of skin flaps. 2nd ed. Edinburgh: Churchill Livingstone; 1994.
4. Kshirsagar R, Chugh Modi A, Rai A. Bilateral inferiorly based nasolabial flaps for the management of advanced oral submucous fibrosis. J Maxillofac Oral Surg 2010;9:22-26. PMID: 23139561.



5. van Wijk MP, Damen A, Nauta JM, Lichtendahl DH, Dhar BK. Reconstruction of the anterior floor of the mouth with the inferiorly based nasolabial flap. Eur J Plast Surg 2000;23:200-203.

6. Maurer P, Eckert AW, Schubert J. Functional rehabilitation following resection of the floor of the mouth: the nasolabial flap revisited. J Craniomaxillofac Surg 2002;30:369-372. PMID: 12425993.


7. Singh S, Singh RK, Pandey M. Nasolabial flap reconstruction in oral cancer. World J Surg Oncol 2012;10:227. PMID: 23110587.



8. Tauro DP. A unique melolabial flap in the surgical management of oral submucous fibrosisŌĆöŌĆ£the sea gull flapŌĆØŌĆöan experience with 85 cases. Int J Oral Maxillofac Surg 2009;38:508.

9. Borle RM, Nimonkar PV, Rajan R. Extended nasolabial flaps in the management of oral submucous fibrosis. Br J Oral Maxillofac Surg 2009;47:382-385. PMID: 18995935.


10. Agarwal M, Gupta DK, Tiwari AD. Extended nasolabial flaps in the management of oral submucous fibrosis. J Maxillofac Oral Surg 2011;10:216-219. PMID: 22942590.



12. Sadasivan A, Thankappan K, Rajapurkar M, Shetty S, Sreehari S, Iyer S. Verrucous lesions of the oral cavity treated with surgery: analysis of clinico-pathologic features and outcome. Contemp Clin Dent 2012;3:60-63. PMID: 22557899.



- TOOLS
-
METRICS

-
- 2 Crossref
- Scopus
- 7,083 View
- 172 Download
- Related articles in ACFS
-
Asian Pacific Craniofacial Association and Archives of Craniofacial Surgery2022 April;23(2)
Potential role of artificial intelligence in craniofacial surgery2021 October;22(5)
Delayed intraorbital infection after craniofacial bone surgery2019 October;20(5)
The Efficacy of Bioabsorbable Mesh in Craniofacial Trauma Surgery2016 September;17(3)