|
 |
- Search
| Arch Craniofac Surg > Volume 19(4); 2018 > Article |
|
Abstract
Intraorbital wooden foreign bodies may present difficulties in diagnosis due to their radiolucent nature. Delayed recognition and management can cause significant complications. We present a case report that demonstrates these problems and the sequela that can follow. A 56-year-old man presented with a 3-cm laceration in the right upper eyelid, sustained by a slipping accident. After computed tomography (CT) scanning and ophthalmology consultation, which revealed no fractures and suggested only pneumophthalmos, the wound was repaired by a plastic surgery resident. Ten days later, the patientŌĆÖs eyelid displayed signs of infection including pus discharge. Antibiotics and revisional repair failed to solve the infection. Nearly 2 months after the initial repair, a CT scan revealed a large wooden fragment in the superomedial orbit. Surgical exploration successfully removed the foreign body and inflamed pocket, and the patient healed uneventfully. However, the prolonged intraorbital infection had caused irreversible damage to the superior rectus muscle, with upgaze diplopia persisting 1 year after surgery and only minimal muscle function remaining. We report this case to warn clinicians of the difficulties in early diagnosis of intraorbital wooden foreign bodies and the grave prognosis of delayed management.
Due to their radiolucent nature, intraorbital wooden foreign bodies, when externally invisible, may be difficult to diagnose even with computed tomography (CT) or magnetic resonance imaging (MRI) due to their radiolucent nature. Delayed recognition and management can cause significant complications such as orbital cellulitis or abscess formation, chronic discharging sinuses, extraocular muscle damage, exophthalmos, and even central nervous system infection. We present a case report that demonstrates these diagnostic and therapeutic problems and the possible sequela.
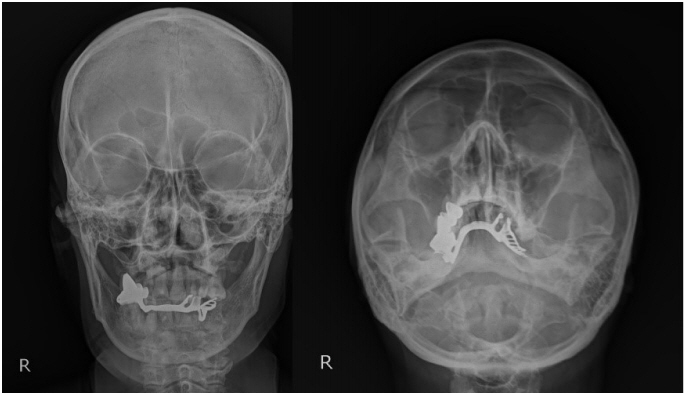
A 56-year-old man came to the emergency room with a 3-cm laceration in the right upper eyelid and severe periorbital swelling. The patient was drunk when injured and could not recall the exact circumstances of the accident. He could only presume that he had slipped and fallen down. Physical examination revealed subconjunctival hemorrhage and chemosis with mildly restricted extraocular movement (EOM) in all directions. Pupil size and light reflex were normal, as was visual acuity. After CT scanning and ophthalmology consultation, which suggested only mild retrobulbar hemorrhage and pneumophthalmos (Fig. 1), the wound, which appeared subcutaneous in depth with no visible foreign objects, was repaired by a plastic surgery resident.
The patient, who had been prescribed eyedrops to lower intraocular pressure along with oral tranexamic acid and intravenous steroids and antibiotics by the ophthalmology department, returned for outpatient follow-up 7 days later and had the sutures removed. Periorbital edema had improved, less so in the upper lid area where ptosis was now observed, previously unnoted due to the severe periorbital edema. EOM restriction had also lessened, except for in the upward direction. The remaining symptoms were attributed to intraorbital swelling, hemorrhage and emphysema by both the plastic surgery and ophthalmology departments. Three days later, the eyelid showed signs of infection including foul-smelling pus discharge, erythema and a soft palpable mass-like bulge. Incisional drainage with oral levofloxacin alleviated these inflammatory signs, and delayed repair with curettage was performed 7 days later. However, signs of infection had recurred when the patient returned to have the sutures removed 1 week later though levofloxacin had been constantly administered during these 2 weeks and there was no bacterial growth from the pus swab culture. Pus discharge, EOM limitation and diplopia persisted even after oral clindamycin was administered for 3 weeks following confirmation of growth of Staphylococcus epidermidis from follow-up wound cultures.
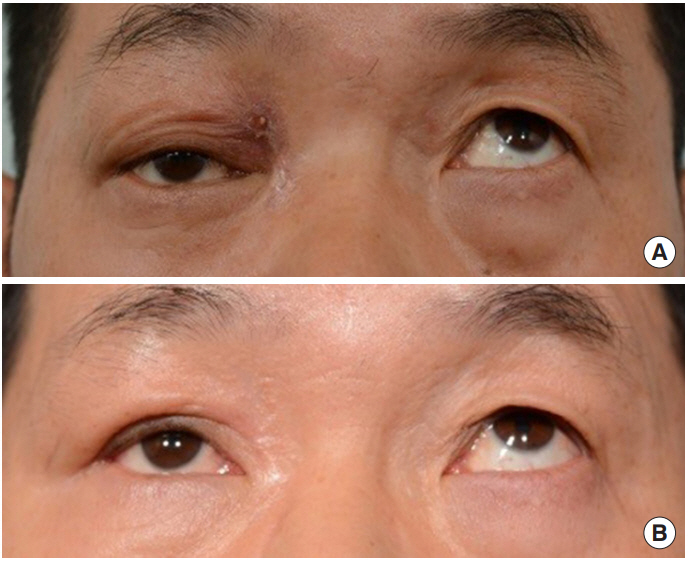
Nearly 2 months after the initial injury an enhanced orbital CT scan revealed an elongated lesion with perilesional retrobulbar fat stranding at right conal and extraconal spaces and superior rectus muscle displacement with swelling, which was interpreted by the radiology department as a retained wooden foreign body with superimposed orbital cellulitis (Fig. 2). Surgical exploration under general anesthesia was performed, and a piece of wood measuring 2.3 cm in length was removed through an incision on the superomedial upper eyelid, followed by scrupulous curettage and copious irrigation of the inflamed pocket (Fig. 3). The repaired surgical wound healed with no recurrent infections, and gradual improvement of blepharoptosis and EOM limitation was evident. Secondary scar revision and intralesional steroid injections further improved cicatricial contracture of the upper medial canthal area and residual symptoms of ptosis. However, the prolonged intraorbital infection had caused irreversible damage to the superior rectus muscle, with upgaze limitation and diplopia due to minimal remnant muscle function persisting at 1 year after surgery (Fig. 4).
Bartkowski et al. [1] have reported 20 intraorbital foreign bodies in 677 orbital trauma cases for a total incidence of 2.9%. Depending on their chemical composition, intraorbital foreign bodies can be classified into (1) metallic (2), non-metallic, and (3) organic substances [2]. Among the three types, organic substances are not only much more difficult to detect on imaging studies but also pose a higher risk of complications because secondary infection or decay of the foreign body may cause severe inflammation [3].
Among organic substances, wooden foreign bodies provide an ideal environment for microorganism growth due to their organic nature and porous consistency [3]. Retained intraorbital wooden foreign bodies may lead to complications such as prolonged suppuration with a draining fistula, foreign body granuloma, orbital cellulitis, abscess formation, panophthalmitis, extraocular muscle damage, exophthalmos and even brain abscesses [4,5]. Trauma cases that apparently seem minor with no visibly protruding objects can still retain intraorbital wooden foreign bodies. In the absence of outwardly detectable signs, a high index of suspicion for the possibility of such penetrating events is required, particularly because a detailed physical examination is often overlooked in minor trauma cases, delaying detection and management which can potentially lead to severe sequela.
As there are no definitive imaging studies for detecting intraorbital wooden material, the respective advantages and disadvantages of the following studies should be taken into account for early detection and differentiation of organic and nonorganic foreign bodies. As demonstrated by the nonspecific findings of this patientŌĆÖs initial plain skull radiographs (Fig. 5), the radiolucent nature of intraorbital wooden foreign bodies often renders plain film radiography useless in detecting the substances. Meanwhile, on CT scans, wooden foreign bodies may be misdiagnosed as emphysema, as was in this particular case [6]. CT findings of wooden objects vary over time and with the composition of the cellulose matrix [4]. In the acute stage the considerably low density of wood can resemble air bubbles. In the subacute stage, wooden objects show a moderate density similar to orbital fat. In the chronic stage, the density can become higher than that of the adjacent extraocular muscles, raising the possibility of detection in CT imaging. At the same time, an inflammatory foreign body retained to this stage could potentially cause severe complications [2,4,7]. On MRI, both dry and fresh wood are usually hypointense relative to intraorbital fat on both T1- and T2-weighted sequences and do not enhance with gadolinium [5,8]. However, MRI cannot be used when metallic foreign bodies are suspected, as the magnetic field may move any metallic structures inside the orbit. The generally high cost and extended scan times of MRIs also often make them a less favorable option [2,7]. Lastly, ophthalmic ultrasonography requires specific expertise that is not widely available, and, similar to MRI, is time consuming while less effective in detecting wooden bodies in the orbit [4,9]. In short, no single imaging study can be considered the gold standard for diagnosing intraorbital wooden foreign bodies.
Surgical removal of wooden foreign bodies requires extreme caution. The exact number and location of the wooden fragments should be approximated through imaging studies as best as possible before surgery. Utmost care must be taken to prevent fragmentation of wood pieces during extraction, which can result in fragment retention, migration or late infection [10].
The patient involved in this case could not remember the circumstances of his injury, and no wooden pieces were immediately visible in the wound. This lack of clinical signs led to the equivocal initial CT findings being interpreted as emphysema by all involved physicians. In addition, although symptoms of infection persisted for over 2 months, the patient was not compliant with a close follow-up schedule. This both impeded intensive intravenous antimicrobial therapy and delayed detection of the causal object, for although residents suspected the possibility of a foreign body after 1 month of continued symptoms, it was another month before the patient was finally persuaded to adjust his personal schedule to meet a board-certified plastic surgeon for the first time and receive a CT scan. No additional imaging studies had been performed during this 2-month period. The longstanding granulomatous reaction induced by the unrecognized wooden foreign body resulted in significant sequela; permanent limitation of upward gaze, blepharoptosis and upper medial canthal scar contracture [9]. Therefore, in patients presenting with penetrating periorbital trauma, a high index of suspicion for retained foreign bodies based on a detailed history of the injury and thorough evaluation of clinical signs is necessary, especially when inflammatory signs persist and EOM limitation is evident. Implementing appropriate imaging modalities for diagnosis and careful surgical removal of the foreign material is critical to minimize complications.
Fig.┬Ā1.
Initial computed tomography (CT) scan taken at the emergency room. The wooden foreign body (arrows) embedded deep in the superomedial orbit was mistaken for emphysema by the ophthalmology, radiology and plastic surgery departments.
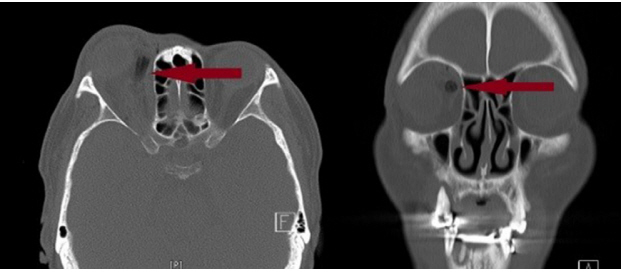
Fig.┬Ā2.
Secondary computed tomography (CT) scan taken almost 2 months after injury, clearly displaying the retained wooden foreign body (arrows) with perilesional retrobulbar fat stranding, superimposed infection and superior rectus muscle displacement with swelling.
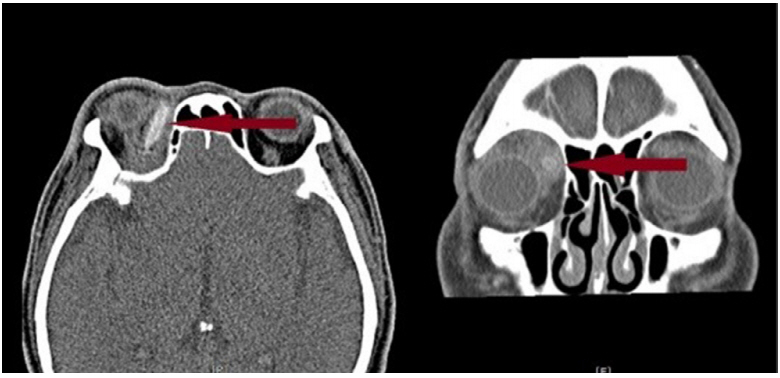
Fig.┬Ā3.
Intraoperative findings. Surgical exploration successfully removed a 2.3-cm-sized wooden foreign body from the superomedial orbit. (A) Intraoperative view of the wooden foreign body inside the surgical field. (B) Removed wooden object.

Fig.┬Ā4.
Preoperative and postoperative clinical photographs. (A) Preoperative clinical photo displaying upgaze limitation of the right
eye and pus discharge on medial upper eyelid. (B) Postoperative 9 month photo. Upgaze and upper lid function have improved but upgaze is still severely limited; secondary scar revision with contracture release on the upper medial lid area has also been performed.
REFERENCES
1. Bartkowski SB, Kurek M, Stypulkowska J, Krzystkowa KM, Zapala J. Foreign bodies in the orbit: review of 20 cases. J Maxillofac Surg 1984;12:97-102.


2. Ananth Kumar GB, Dhupar V, Akkara F, Praveen Kumar S. Foreign body in the orbital floor: a case report. J Maxillofac Oral Surg 2015;14:832-5.


3. Sitaula S, Gautam V. Intraorbital wooden foreign body: a case report. J Kathmandu Med Coll 2014;3:119-21.

4. Ho VT, McGuckin JF Jr, Smergel EM. Intraorbital wooden foreign body: CT and MR appearance. AJNR Am J Neuroradiol 1996;17:134-6.


5. Dunn IF, Kim DH, Rubin PA, Blinder R, Gates J, Golby AJ. Orbitocranial wooden foreign body: a pre-, intra-, and postoperative chronicle: case report. Neurosurgery 2009;65:E383-4.



6. Roberts CF, Leehey PJ 3rd. Intraorbital wood foreign body mimicking air at CT. Radiology 1992;185:507-8.


7. Lee JA, Lee HY. A case of retained wooden foreign body in orbit. Korean J Ophthalmol 2002;16:114-8.


8. Nagae LM, Katowitz WR, Bilaniuk LT, Anninger WV, Pollock AN. Radiological detection of intraorbital wooden foreign bodies. Pediatr Emerg Care 2011;27:895-6.


- TOOLS
-
METRICS

-
- 12 Crossref
- Scopus
- 5,473 View
- 86 Download
- Related articles in ACFS
-
Delayed intraorbital infection after craniofacial bone surgery2019 October;20(5)