|
 |
- Search
| Arch Craniofac Surg > Volume 19(4); 2018 > Article |
|
Abstract
Replantation using microvascular anastomosis is considered to be the optimal method in treating the amputated ear in terms of resulting color, texture, and shape. Only a few cases of ear replantation have been reported because it is anatomically difficult to identify suitable vessels for anastomosis. We successfully replanted the amputated helical rim of the ear using single arterial anastomosis. A 37-year-old man had his helical rim amputated by a human bite. The amputee was about 4 Ă 1 cm in dimension, composed of skin and soft tissue including auricular cartilage. Replantation was performed anastomosing a small artery of the amputee with a terminal branch of the posterior auricular artery. After replantation, intravenous heparinization was performed and prostaglandin E1 and aspirin were administered. Venous congestion was decompressed by stab incisions applied with heparin solution soaked gauze. Venous congestion of the amputee slowly began to resolve at 4 days after the operation. The amputated segment of the helical rim survived completely with good aesthetic shape and color. The authors propose that performing microvascular anastomosis should be attempted especially if it is possible to detect vessels on cut surfaces of ear amputee and stump. Proper postoperative care for venous congestion, arterial insufficiency, and infection should be followed for amputee survival.
The outer ear is an important aesthetic component of the face, its appearance as significant as its functional role. Therefore, reconstruction for the amputated ear should aim to retain its original shape. Although there are variable options of treatment, replantation of the amputated ear is better than other options in terms of color, texture and shape. Replantation by microvascular anastomosis is the first choice of treatment, but only a few cases of ear replantation have been reported because it is difficult to identify suitable vessels for anastomosis. We successfully replanted the amputated helical rim of ear using single arterial anastomosis. Venous congestion that occurred after surgery was decompressed by stab incisions and salvage using repeated application of gauze soaked with heparin solution. The amputated segment survived completely.
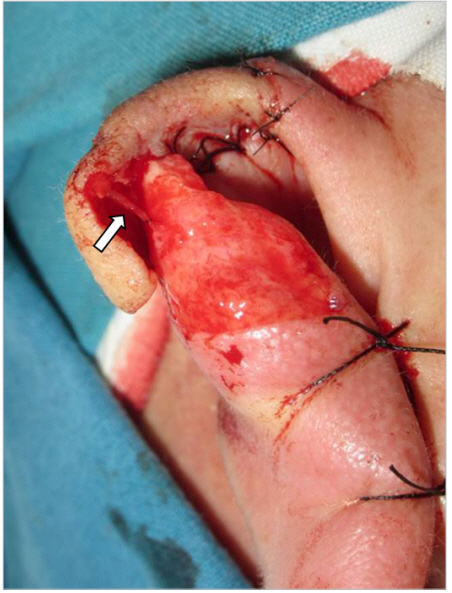
An otherwise healthy 37-year-old man presented with amputation of his right helical rim inflicted by a human bite. The size of the amputee was approximately 4Ă1 cm in dimension and was composed of skin, soft tissue, and auricular cartilage (Fig. 1). Upon arrival at the operating room, 3 hours of warm ischemic time and 8 hours of cold ischemic time (a total of 11 hours of ischemic time) had passed by. Under general anesthesia, replantation was performed. Fixing the posterior surface with nylon sutures, we explored the cut surfaces of the amputee and the stump. We detected a small transected artery on the cut surface of the amputee and identified a terminal branch of the posterior auricular artery (PAA) on the stump. They were approximated and anastomosed by three end-to-end stitches with 11-0 Ethilon sutures (Ethicon, Somerville, NJ, USA) (Fig. 2). Identification and anastomosis took approximately 1 hour. Thus, total ischemic time was 12 hours, including 11 preoperative and 1 intraoperative hour. After replantation, intravenous heparinization was performed for 5 days targeting activated partial thromboplastin time within the range of 30 seconds to 50 seconds. Intravenous prostaglandin E1 (Eglandin; Mitsubishi Tanabe Korea, Seoul, Korea) was administered at a dose of 10 Îźg per day for 7 days and oral aspirin (Rhonal; Kunwha Pharmaceutical Co., Seoul, Korea) at a dose of 100 mg per day for 18 days. Venous congestion that occurred immediately after surgery was decompressed by stab incisions wiped with heparin solution soaked gauze, which was changed every 15 minutes (Fig. 3). Preoperative hemoglobin level was 16 g/dL, and was maintained at 14 g/dL during salvage. Packed red blood transfusion was not required. The venous congestion of the amputee slowly began to recover at 4 days after the operation (Fig. 4). The stitches were removed on the 10th postoperative day and the patient discharged from the hospital on the 12th postoperative day. Thereafter, follow-up was done at the outpatient clinic, and clinical photos were taken at 5 weeks and 3 months (Figs. 5, 6). The amputated segment of the helical rim survived completely with good aesthetic color, texture and shape. The patient was satisfied.
Before advances in microsurgical techniques, treatment modalities of the amputated ear included reconstruction with the auricular cartilage after it was dissected from the amputated segment and embedded in the abdominal wall or the retroauricular subcutaneous tissues, reconstruction with the dissected auricular cartilage after wrapping with temporalis muscle fascia, and reconstruction with composite grafts reattaching the amputated segment to its original position [1-3]. However, these procedures result in an unacceptable shape or develop partial necrosis. On the other hand, although microsurgical replantation of the amputated ear requires much experience, it usually leads to highly satisfactory results. In cases of earlobe amputation, although it is feasible, reconstruction with composite grafts has limited indications because of the relatively large size of the amputated segment and variable survival rate. Flap surgery has the disadvantages of a mismatch in texture and color and is accompanied by scar formation at the donor site. Since 1980 when Pennington et al. [4] initially performed a successful replantation of a completely avulsed ear by microvascular anastomosis, many such cases have been reported in the literature, most of which were of total or subtotal avulsion (upper two thirds of the ear) [4-7]. However, there have been a few reports regarding successful replantation of smaller amputated segments of the ear [8]. The authors have experienced and published successful replantation of an amputated earlobe using the terminal branches of the superficial temporal artery (STA) [5].
As stated in previous reports, the most critical point in partial ear amputation replantation is identifying appropriate vessels for anastomosis. Because vessels distributed in the ear are fine and anatomically ill-defined, they may cause technical difficulties. The auricular surface is supplied by well-developed interconnections of the auricular branches that originate from the PAA and STA. These interconnections make the ear potentially well vascularized by one arterial system when the other is ligated during surgery [6]. The STA ascends in front of the auricle, of which main branches give off its final branches to the ear lobe, the tragus and the ascending helix. Cymba conchae, cavum conchae, scapha and helix are supplied by perforating branches of the PAA. Although there are variabilities, the PAA is reported to be dominant artery for the auricle [7]. In this case, a terminal branch of the PAA was identified, and end-toend anastomosis was performed.
After confirming reperfusion of the replanted segment, we tried to perform venous anastomosis but failed to identify appropriate veins for anastomosis. Inevitably, venous congestion occurred after the procedure, which was resolved by stab incisions and drainage on the anterior surface of replant. According to the literature, in cases when venous anastomosis is unfeasible, venous congestion can be decompressed through a variety of exsanguination methods. These include continual rubbing of the wound margin, stab incisions or pinpricks, and systemic or local administration of heparin and leech therapy [9-14]. Exsanguination by arteriovenous anastomosis is a surgical procedure that connects a remaining artery to a relatively large vein either directly or with a vein graft after arterial anastomosis is completed [7]. However, the smaller the amputee, the more challenging arteriovenous anastomosis becomes. Because complete decompression of venous congestion cannot be achieved in such small amputated segments, the alternative is salvage via stab incisions or pinpricks. This method close observation and meticulous management of the surgical wound because blood clots on the wound need to be removed to achieve continuous exsanguination. In cases of severe crushing injuries, such management may aggravate the surgical wound, and any delayed monitoring may result in irreversible changes.
As in replantation of the upper and lower extremities, antiplatelet drugs such as dipyridamole or low dose aspirin have been used to inhibit blood coagulation. Heparin may be administered systemically or locally to prolong blood clotting time, systemic heparin therapy requires a continuous monitoring of clotting time and may induce bleeding from other sites in patients with associated injuries. The medical leech is widely used to decompress venous congestion in patients who have undergone digital replantation. The leechâs saliva contains hirudin, which has the ability to induce anticoagulation, local anesthesia, and vasodilation, allowing persistent exsanguination [15,16]. Protection against microorganisms such as Aeromonas hydrophila should be provided by administration of second- or third-generation cephalosporins and aminoglycosides.
Kim et al. [8] reported a case in which microsurgical replantation of a partial amputation of the helix of the ear was followed by leech salvage in 2009. We have had experience using leeches in our previous auricular amputation cases, but the amputee in this case was (1) relatively small and therefore sufficiently exsanguinated using heparin gauze wipes and (2) accompanied by a large contact area to amputee volume ratio, therefore venous neovascularization was probably easily formed. Venous congestion began to recover at 4 days after the operation, which is earlier than the average 7 to 8 days reported in the literature [5,8].
We report a successful case of artery only anastomosis performed for a small segment amputation of the auricular helix. Although the vascular anatomy is ill-defined and the vessels are small, replantation should be attempted as a first line option because this will most likely result in excellent texture, color, and shape. Venous anastomosis is challenging and may be overcome using exsanguination therapies.
REFERENCES
1. Sexton RP. Utilization of the amputated ear cartilage. Plast Reconstr Surg (1946) 1955;15:419-22.


2. Mladick RA, Carraway JH. Ear reattachment by the modified pocket principle: case report. Plast Reconstr Surg 1973;51:584-7.


3. Clemons JE, Connelly MV. Reattachment of a totally amputated auricle. Arch Otolaryngol 1973;97:269-72.


4. Pennington DG, Lai MF, Pelly AD. Successful replantation of a completely avulsed ear by microvascular anastomosis. Plast Reconstr Surg 1980;65:820-3.


5. Jung SN, Yoon S, Kwon H, Yim YM. Successful replantation of an amputated earlobe by microvascular anastomosis. J Craniofac Surg 2009;20:822-4.


6. Strauch B, Yu HL, Chen ZW, Liebling R. Atlas of microvascular surgery: anatomy and operative approaches. New York: Thieme; 1993.
7. Pinar YA, Ikiz ZA, Bilge O. Arterial anatomy of the auricle: its importance for reconstructive surgery. Surg Radiol Anat 2003;25:175-9.


8. Kim KS, Kim ES, Hwang JH, Lee SY. Microsurgical replantation of a partial helix of the ear. Microsurgery 2009;29:548-51.


9. Steffen A, Katzbach R, Klaiber S. A comparison of ear reattachment methods: a review of 25 years since Pennington. Plast Reconstr Surg 2006;118:1358-64.


10. Cho BH, Ahn HB. Microsurgical replantation of a partial ear, with leech therapy. Ann Plast Surg 1999;43:427-9.


11. Kind GM, Buncke GM, Placik OJ, Jansen DA, DâAmore T, Buncke HJ Jr. Total ear replantation. Plast Reconstr Surg 1997;99:1858-67.


12. Turpin IM, Altman DI, Cruz HG, Achauer BM. Salvage of the severely injured ear. Ann Plast Surg 1988;21:170-9.


13. Juri J, Irigaray A, Juri C, Grilli D, Blanco CM, Vazquez GD. Ear replantation. Plast Reconstr Surg 1987;80:431-5.


14. Tanaka Y, Tajima S. Completely successful replantation of an amputated ear by microvascular anastomosis. Plast Reconstr Surg 1989;84:665-8.


- TOOLS
-
METRICS

-
- 4 Crossref
- Scopus
- 5,454 View
- 95 Download
- Related articles in ACFS