Cryptotia recurrence lowering technique with additional acellular dermal matrix graft
Article information
Abstract
Background
Cryptotia is a congenital anomaly in which the upper part of the retroauricular sulcus is absent and buried underneath the temporal skin. Various surgical techniques have been reported for the correction of cryptotia following Kubo’s V-Y plasty in 1933. Conventional methods using a local skin flap, skin grafting, tissue expansion, Z-plasty, and any of these combined approaches can result in skin deficiency of the upper auricle. The aim of this study was to develop a new method that improves cosmetic results and has fewer complications.
Methods
This study involved four patients in whom five cryptotia deformities were corrected using V-Y plasty and Z-plasty. After elevation of the flap, acellular dermal matrix (ADM; MegaDerm) that was over 5 mm in thickness was applied to the cephalo-auricular angle and positioned to enhance the projection of the ear. Lastly, the flap was transposed to complete the repair.
Results
Between January 2014 and February 2018, cryptotia correction with ADM graft was performed in four patients. None of the patients developed a recurrence of cryptotia, and there were no postoperative complications such as wound infection, seroma formation, and dehiscence. In addition, the procedures resulted in a favorable cosmetic appearance.
Conclusion
Based on these findings, i.e., no recurrence and a favorable cosmetic result, when using an ADM graft, it is suggested that this technique could be an alternative method of cryptotia correction. It could also lessen donor-site morbidity when compared to autologous cartilage grafting and be more cost-effective than using cartilage from a cadaver.
INTRODUCTION
Cryptotia is a congenital deformity in which the upper pole of the ear is buried beneath the temporal skin. It is a relatively common disease in Asians when compared to its incidence in Caucasians [1]. The congenital anomalies of the ear auricle can be divided into malformational disease and deformational disease, and cryptotia is included in the latter [2]. Abnormal insertion of the intrinsic muscles of the ear or the superior auricular muscle can be the deformational force [3]. This force usually causes the deformation of upper auricular cartilage, and two-thirds of patients with cryptotia have a cartilaginous as well as a skin deformity [1].
Many nonsurgical and surgical treatments for cryptotia correction have been reported. Nonsurgical therapy is usually effective in neonates because neonatal auricular cartilage is extremely pliable. After the neonatal stage, surgical treatment is considered more effective and the surgery is usually delayed until after the age of 6 years, when auricular growth is sufficient for correction [4,5]. Various techniques have been introduced in the literature (e.g., local flap [6], skin graft [7], expanded flap with tissue expander [8,9], etc.). Each technique has its advantages and disadvantages and these factors should be applied appropriately to the surgeon’s judgment and according to the patient’s status.
Recurrence of cryptotia is one of the most problematic early surgical complications. The recurrence rate is affected by the method of surgery and the rate is relatively high when correcting with local flaps. To help prevent this complication, the tissue expansion technique [8-10], molding with splint technique [11], and cartilage wedge graft technique [12] were presented. Though these methods have reduced the recurrence rate of cryptotia to a satisfactory level, the procedures are time-consuming or have an undesirable donor-site morbidity rate. Because of the complications of these techniques, their effectiveness is significantly reduced. Therefore, to address cryptotia recurrence, increased surgical time, and donor-site morbidity, the authors have designed a technique using an acellular dermal matrix (ADM) graft. This paper attempts to analyze the efficiency and suitability of this method.
METHODS
Five cryptotia deformities in four patients were corrected using Z-plasty and ADM graft. The central arm of the Z-plasty was positioned in the inferoposterior direction from the posterior edge of eminentia cymba conchae to the hairline. The anterior line was drawn downwards along the posterior margin of the ear and the posterior line was drawn along the hairline. Next, local anesthetic was injected into the operative field. The incision was made and the superior auricular muscle was detached from the helix. After this step, the skin flap was elevated. Additionally, the skin flap behind the ear was elevated above the cartilage. The posterior skin flap is relatively easy to dissect as it is loosely attached to the cartilage compared to the anterior skin of the ear. All the tissue, including abnormally inserted muscle, was dissected from the ear cartilage. The cartilage abnormality was then observed and ADM was carved as a wedge shape. The matrix was then grafted at the posterior auricular sulcus with 5-0 Prolene (Ethicon, Somerville, NJ, USA) (Fig. 1). The symmetry of projection of the ears was confirmed and a 200 mL Hemovac drain was inserted under the skin flap to prevent seroma and hematoma formation. The Z-plasty was then completed.
RESULTS
Between January 2014 and February 2018, five cryptotia deformities in four patients presented and the condition was corrected using an ADM graft technique. A Z-plasty method was effectively designed to cover the posterior exposed cartilage and to create an auriculocephalic sulcus. Postoperative complications such as wound infection, seroma formation, and dehiscence were absent in these cases. Patient age ranged from 9 to 28 years (Table 1) and one patient had previously received corrective otoplasty without cartilage or ADM graft. This patient had redeveloped blunting of the cephalo-auricular angle. However, the second surgery was successful with an added ADM graft (case 2).
Case 1
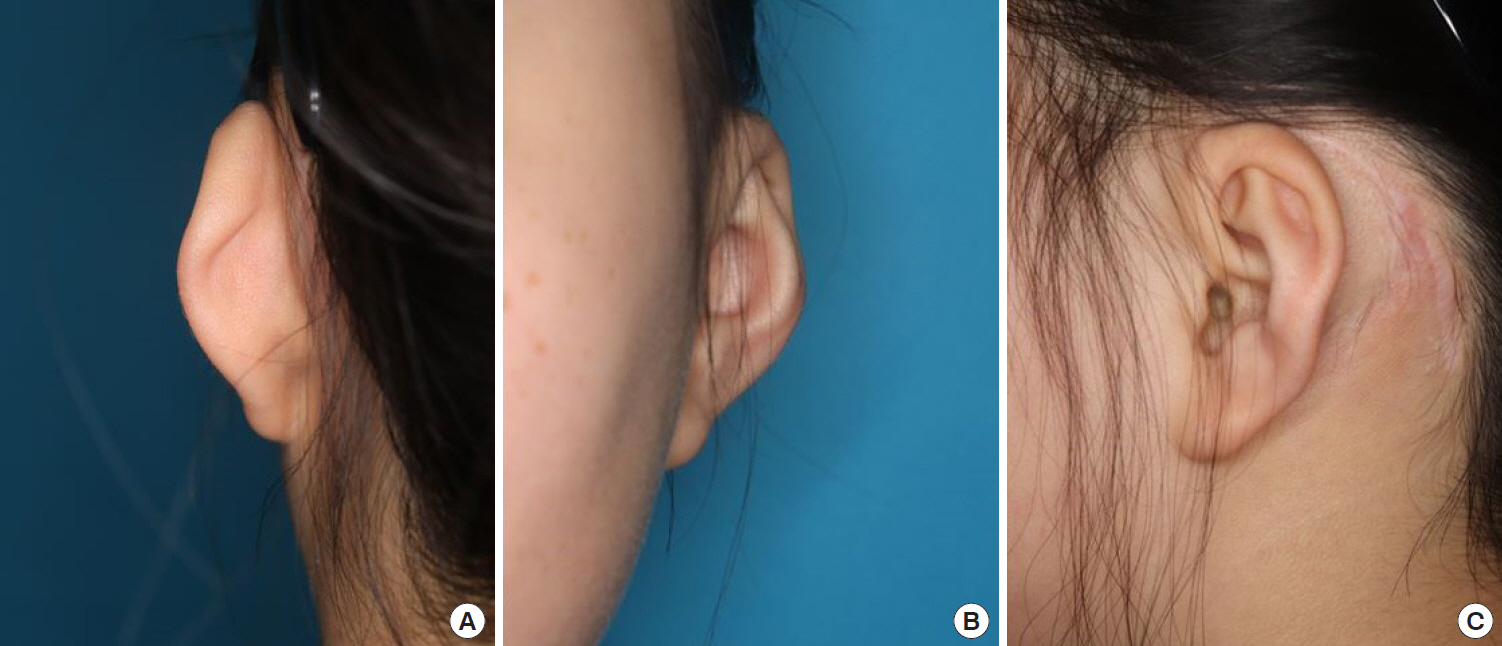
A 9-year-old female patient visited the outpatient clinic and presented with left-sided cryptotia. Because of the asymmetrical shape of the ear and the difficulty wearing glasses, surgical correction was requested. Physical examination revealed mild cryptotia, but the cephalo-auricular sulcus was shallow. It was confirmed as a transverse type of cryptotia in which the body and the superior crus of the antihelix are contracted (Fig. 2).

Preoperative image of the left ear. Transverse type cryptotia and shallow cephalo-auricular angle were noted. (A) Posterior view, (B) anterior view, and (C) lateral view.
As it was not a severe form of cryptotia, the decision was made to cover the elevated posterior auricle using the Z-plasty technique. After making the skin incision, the transverse intrinsic muscle was dissected and 1×2 cm ADM was applied.
At 1-year after surgery, the results remained satisfactory as the auriculotemporal sulcus was still present and the projection of the helix was substantial enough to wear eye glasses. The images in Fig. 3 were obtained a year after the surgery. They show that the ear position was maintained well and without cryptotia recurrence.
Case 2
A 23-year-old female patient was examined at the clinic for the treatment of right-sided cryptotia. The patient received cryptotia correction surgery in October 2014 and despite regular follow-up evaluations, the cryptotia recurred and the ear required an additional surgical correction. The additional correction was necessary due specifically to the recurrence of the blunting of the cephalo-auricular angle, and the lowering of the projection of the upper helix. In addition, the skin flap added in the previous surgery was bulging upward (Fig. 4).

(A) Recurred cryptotia: the skin flap added in the previous operation had bulged upward. (B) Postoperative image: enough ear projection was recovered.
To begin the procedure, the previous surgical scar was opened to approach the upper helix. There remained some deformational force. Next, the adhesion was removed and a wedge graft of ADM was placed at the posterior auricular sulcus. To prevent hematoma and seroma formation, a Silastic drain was inserted and the skin was repaired.
Fig. 4B is obtained a month after the surgery, and a deep cephalo-auricular angle was relatively well maintained. There were no complications until 2 years after surgery but, the scar contracture of the temporal area became a concern. Because the scarring may affect cryptotia recurrence, scar management is ongoing.
DISCUSSION
When evaluating cryptotia cases, the most important points that the surgeon should consider are aesthetic results and low complication rates. The postoperative scar status and adequate projection of the ear helix are essential factors in assessing the aesthetic result. Paredes et al. [13] reported that the surgical correction of cryptotia attempts to achieve four goals: (1) recreation of the auriculo-cephalic sulcus; (2) correction of any cartilaginous deformity; (3) release of abnormal auricular muscle insertion; and (4) provision of additional skin. Many surgeons have described methods to cover an elevated ear helix, while also attempting to reduce scars. As introduced earlier, various techniques, including using a skin graft or local flaps, have been presented. Therefore, it is necessary to properly modulate the above techniques according to the patient’s condition and the experience and judgment of the surgeon.
Cryptotia recurrence is the most problematic early postsurgical complication. One of the main causes of recurrence is skin deficiency. This deficiency occurs frequently using the local flap. Hirose et al. [3] summarized the problem as follows: first, due to the lack of skin, the ears tend to go back to the buried state and second, the natural hairline is disturbed. Also, when designing a large flap to supplement enough skin, the conspicuous scar remains. Skin grafts can provide enough skin for the procedure and various methods of using skin grafts have been suggested. However, common problems with this method are conspicuous scarring and, in addition, color mismatch. Mutimer and Mulliken [8] solved the above problems using a tissue expander. They corrected cryptotia by using a two-staged tissue expander method and no recurrence occurred. However, two times of surgery are required with this method and it is sometimes difficult for patients to accept their cosmetic appearance during the period of the tissue extension. Another method was described by Kim et al. [11] who conducted a correction with a local flap and used a polyethylene implant (Medpor) to prevent early recurrence. Oh et al. [12] conducted a cartilage wedge graft in the superior portion of cephalo-auricular angle to prevent the recurrence. No recurrence has occurred in the aforementioned series.
The method of surgery described here is similar to using a cartilage wedge graft. The ADM in the form of a wedge was grafted on the posterior auricular sulcus and produced good results. Since ADM provides structural support and acts as a barrier between the skin and the cartilage, the recurrence rate can be lowered. In addition, the ADM can be easily handled and sized, and the thickness can be adjusted freely regardless of donor-site morbidity. The postoperative scar may be relatively less noticeable in this procedure than in other procedures, as the local flap is used to counter the skin deficiency, while also reducing the recurrence rate. The authors use Z-plasty, but in the case of a mild cryptotia without cartilage abnormality, the combination of trefoil flap and ADM graft can reduce scarring and the recurrence rate simultaneously.
Questions remain as to whether ADM can faithfully play its role as a scaffold. The hardness of ADM is lower than that of cartilage, but it is hard enough to serve as a scaffold. Also, because it is free from the morbidity of the autologous tissue harvest, the volume and thickness of ADM can be easily manipulated to compensate for the lack of hardness. Second, absorption of ADM is another problem. There were various studies on the ratio of ADM absorption. Kim et al. [14] described no statistically significant decrease in ADM volume after 12 weeks of surgery in Murine model. Besides, other studies showed an absorption rate of 16% to 79.8% [15-18]. Also, the absorption rate can vary sufficiently depending on graft site and blood supply [14]. This problem needs to be checked for a long-term result for cases that have been performed by an ADM graft in the posterior auricular sulcus.
The main limitation of this study is its presentation of a small number of cases. Although there is no recurrence in this series, it is necessary to perform this technique in more cases in order to have more data. Another limitation is the short duration of postsurgical observation. Since the ADM can be absorbed by the body, longer postoperative observation is required than with other surgical methods. Sclafani et al. [15] quantitatively checked the change of the AlloDerm volume in a study that conducted augmentation of the postauricular area soft tissue using AlloDerm and verified that the volume decreased until six months after surgery, and then the volume of AlloDerm was stabilized. The minimum follow-up period in this study is more than one year, although volume absorption may have occurred, but not affected recurrence. In addition, asymmetry may develop during the growth process after the cryptotia correction. An ear of 5 to 7 years old child is similar to that of an adult in size. Therefore, there is not much chance of ear change in the course of growth in our 9 years old child case. However, further research is planned on comparing objective indicators of longterm results in large case.
In conclusion, the authors’ method of cryptotia correction with additional ADM graft could potentially be a method of reducing recurrence rate, while also leaving an inconspicuous scar. This appears to be a safe technique with minimal donorsite morbidity and undesirable sequelae such as infection or ADM graft failure.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.