Necrotizing fasciitis arisen from nose
Article information
A 48-year-old man presented to the emergency room with a 6-day history of exacerbating erythema and swelling on the nose, upper lip, bilateral cheek, and periorbital area. He denied any facial trauma history but reported recent nasal hair plucking. There were necrotic gangrene and crepitus on the nose, upper lip and bilateral cheek with odorous purulent discharge (Fig. 1A). A contrast-enhanced computed tomography confirmed air opacities in soft tissues of the midface (Fig. 2). Overall vital status was unstable with body temperature reaching 39.7°C. The lab results of the patient strongly suggested high risk of necrotizing fasciitis with the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score 12. The patient was under poor hygiene and had history of alcohol abuse and uncontrolled diabetic mellitus with unknown onset.

Patient photos at (A) emergency room admission, (B) before 2nd serial debridement, (C) after 3rd debridement confirming no purulent discharge and fresh soft tissue, (D) 3 months after reconstruction with forehead flap, abbe flap, and bilateral cheek flaps combined.
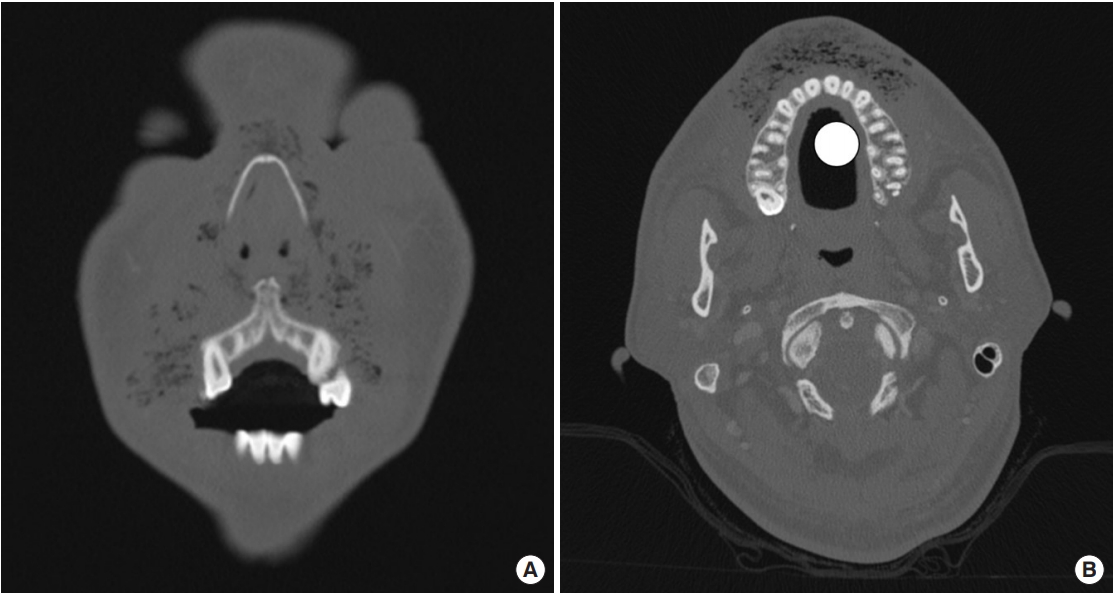
(A, B) Craniofacial contrast-enhanced computed tomography at the patient’s admission showing air opacities among bilateral cheek, upper lip, and nasal soft tissue.
Promptly broad-spectrum antibiotics combination of ampicillin/sulbactam and clindamycin were intravenously (IV) administrated, and initial debridement was performed under general anesthesia. Five days later tissue cultures grew Klebsiella pneumoniae and clindamycin-resistant group B Streptococcus. The antibiotics regimen was changed to ceftriaxone and metronidazole. The patient underwent serial debridement (Fig. 1B) until there was no pus-like discharge from the wound (Fig. 1C). After inflammatory signs and blood test normalized, the facial defect was successfully reconstructed with forehead flap, abbe flap, and bilateral cheek flaps combined (Fig. 1D).
Facial necrotizing fasciitis (NF) spreads rapidly along fascial planes causing extensive necrosis. Immediate surgical debridement of the necrotic tissue and administration of broad-spectrum IV antibiotics are crucial to prevent associated mortality. Facial NF mostly originates from dental or pharyngeal abscess and radiotherapy [1,2]. However, unlike other anatomic sites facial region is rarely affected to NF with the aid of their rich vascular supply [3].
Herein, we report a rare case of a patient who was diagnosed with facial NF without recent history of dental abscess nor radiotherapy. Both nasal plucking and immunocompromised state with uncontrolled diabetic mellitus are predisposing factors for nasal vestibulitis, which may have affected the patient to be prone to the facial NF arisen from nose [4].
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Seoul National University Boramae Hospital (IRB No. 30-2019-9) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patient provided written informed consent for the publication and the use of his images.
