|
 |
- Search
| Arch Craniofac Surg > Volume 20(5); 2019 > Article |
|
Abstract
Post-traumatic hematoma formation is a common complication of contusion. If the hematoma is large enough to aspirate or drain, it can be treated quickly and appropriately. However, if the hematoma is small or concealed by local swelling, it may be overlooked and left untreated. In most cases, a hematoma will resolve following conservative treatment; however, associated infection or muscle fibrosis can occur. Herein, we present the case of a patient with a chin deformity caused by a post-traumatic hematoma. The deformity was treated using botulinum toxin and triamcinolone acetonide injections as minimally invasive treatments. The course of treatment was good.
The occurrence of contusions in the mental region may result in hematoma formation and muscle weakening, which can go unnoticed, particularly if there is no open wound. Over time, fibrosis may develop in the region of the hematoma, which, in conjunction with inactivation of the mentalis muscle, can create facial asymmetry and deformity. In addition to causing cosmetic and functional defects, facial asymmetry can have social and psychological effects. The treatment of post-traumatic chin deformities has not yet been standardized, although surgical methods are possible [1]. In this report, we present a case of a chin deformity caused by muscle fibrosis, which was successfully treated non-surgically using botulinum toxin type A (BoNT-A) and triamcinolone acetonide injections as a convenient, less invasive method.
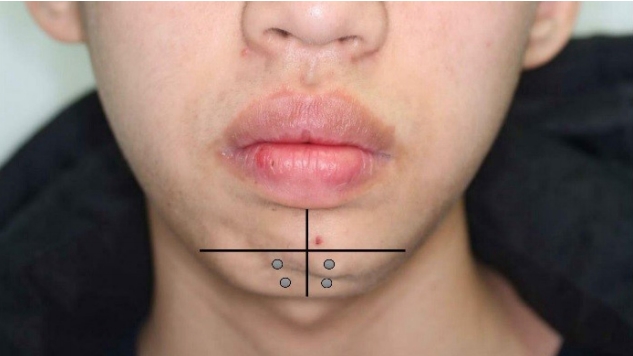
A 14-year-old adolescent presented to our hospital with a masslike lesion left of the mental region (Fig. 1). Three years prior, he collided with a parked car while riding a bicycle and subsequently sought medical attention at the emergency room. There was no fracture or laceration in the mental region; therefore, a plastic surgeon was not consulted. The presumption was that the collision led to post-traumatic hematoma formation in the chin; however, because this was not immediately obvious at the time of injury, no treatment was provided.
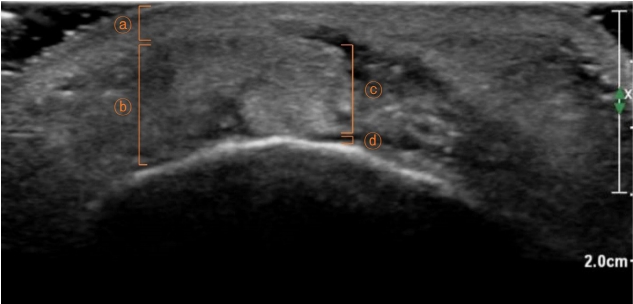
On physical examination, the lesion was found to be soft, immovable, and ovoid, and measured 2.3├Ś0.8 cm with irregular margins. Ultrasonography of the mass indicated hypoechogenicity of the mental fat layer, suggesting mentalis muscle fibrosis (Fig. 2).
Rather than surgically excising the lesion, we treated the contralateral mentalis with BoNT-A injections (Botulax; Hugel Inc., Chuncheon, Korea). We presumed that the patient habitually overused the mentalis muscle, and that left mentalis muscle function had further decreased due to trauma. Botulax was mixed with 1 mL of normal saline and injected at two points on each side of the mentalis in 2.5 U injections (total 10 U) using a 31-gauge needle (Fig. 3).
Following BoNT-A injections in 2 consecutive months, the patientŌĆÖs chin asymmetry improved; however, a bulging deformity over the left mentalis remained (Fig. 4). Therefore, triamcinolone (20 mg/mL) (Rheudenolone; Kukje Pharm, Ansan, Korea) mixed with 2% lidocaine was injected into the subcutaneous tissue of the mental region.
After 5 months of follow-up, reactivation of the mentalis muscle was observed, prompting us to resume the BoNT-A injections. The patient then visited our clinic every 6 months for further BoNT-A injections. After 8 months of follow-up, no palpable mass-like lesion was observed on the chin (Fig. 5).
In the present case, facial bone computed tomography of the patient indicated that the mandible was intact, and that there were no open wounds caused by the accident. Three years later, ultrasonography indicated the presence of post-traumatic hematoma, caused by capillary bleeding and edema at the contusion site, and hypoechogenicity of the mental fat layer, suggesting fibrosis of the mentalis muscle. This caused fibrotic changes of the mentalis muscle.
Many surgeons have reported the advantages or benefits of surgical treatment of muscle fibrosis; however, in most cases, the surgical results have been unsatisfactory [1]. In this case, we used BoNT-A and triamcinolone injections as a non-invasive and less complicated form of treatment to improve the patientŌĆÖs chin deformity.
Triamcinolone acetonide is a corticosteroid that can be used for intra-lesion injections due to its good local potency, relatively low systemic absorption, and persistence in tissues. Triamcinolone acetonide acts as an immunosuppressive agent due to its antagonistic activity on soluble factors released by sensitized lymphocytes that have been activated by nonspecific antigens, and it also inhibits inflammatory reactions. Therefore, fibrosis can be prevented by decreasing fibroblastic proliferation and collagen deposition [2]. Other studies have used triamcinolone acetonide for the treatment of fibrosis [3].
In 1985, Scott et al. [4] published the first study on using botulinum toxin to treat blepharospasm. Since then, botulinum toxin has been used for aesthetic purposes in diverse anatomical regions, including the eye, forehead, calf, and trapezius muscle. Botulinum toxin has also been used for therapeutic purposes in treating conditions such as sialocele, hyperhidrosis, facial spasms, and facial asymmetry [5]. Botulinum toxin is a common treatment for correcting facial asymmetries, particularly in cases of hemifacial palsy in which BoNT-A injections on the contralateral side are an effective treatment [6]. Botulinum toxin acts by blocking acetylcholine in neuromuscular synaptic clefts [7].
Based on the results of previous studies, we expected to observe three therapeutic effects of BoNT-A injections. First, we expected to correct the hyperactivity of the contralateral mentalis muscle. The mentalis muscle was not treated within an appropriate period of time after the initial contusion, resulting in fibrosis, which led to muscle weakening and chin asymmetry due to the uninjured contralateral mentalis. The patientŌĆÖs habit of unconsciously overusing the mentalis may have influenced this asymmetry. Second, the BoNT-A injections were expected to restore the muscle to a resting state and assist in muscle healing. Therefore, BoNT-A was injected into both the injured and contralateral muscles [8]. Finally, BoNT-A was expected to aid in the treatment of muscle fibrosis. BoNT-A has emerged as both a primary and an adjunctive treatment for musculoskeletal pain, muscle spasms, spasticity, and a variety of other disorders. Recent reports have also shown that BoNT-A injections are useful for treating radiation fibrosis syndrome [9].
After these procedures, the patient was satisfied with the results, and there were no associated complications during the 8-month follow-up period. Based on this report, BoNT-A injections and triamcinolone therapy can be used to correct muscle fibrosis and facial asymmetry.
Notes
Fig.┬Ā1.
The arrow shows the 2.3-├Ś0.8-cm palpable mass on the chin. The asterisk shows activation of the contralateral mentalis muscle.

Fig.┬Ā2.
Ultrasonogram of the chin lesion. A 2.3-├Ś0.8-cm subcutaneous mass and hypoechogenicity of the mental fat layer can be identified, suggesting fibrotic changes following hematoma formation (ŌōÉ, dermis layer; Ōōæ, subcutaneous layer; ŌōÆ, mass; Ōōō, muscle layer).
REFERENCES
1. Beiner JM, Jokl P. Muscle contusion injuries: current treatment options. J Am Acad Orthop Surg 2001;9:227-37.


2. James L, Shetty A, Rishi D, Abraham M. Management of oral submucous fibrosis with injection of hyaluronidase and dexamethasone in grade III oral submucous fibrosis: a retrospective study. J Int Oral Health 2015;7:82-5.
3. Singh M, Niranjan HS, Mehrotra R, Sharma D, Gupta SC. Efficacy of hydrocortisone acetate/hyaluronidase vs triamcinolone acetonide/hyaluronidase in the treatment of oral submucous fibrosis. Indian J Med Res 2010;131:665-9.

4. Scott AB, Kennedy RA, Stubbs HA. Botulinum A toxin injection as a treatment for blepharospasm. Arch Ophthalmol 1985;103:347-50.


5. Hosp C, Naumann MK, Hamm H. Botulinum toxin treatment of autonomic disorders: focal hyperhidrosis and sialorrhea. Semin Neurol 2016;36:20-8.



6. Kim J. Contralateral botulinum toxin injection to improve facial asymmetry after acute facial paralysis. Otol Neurotol 2013;34:319-24.


7. Popescu MN, Popescu SI, Cernat CC, Boariu AM, Calin E, Vieru A, et al. Injecting botulinum toxin into the treatment of blepharospasm. Rom J Ophthalmol 2018;62:162-5.



- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 8,690 View
- 108 Download
- Related articles in ACFS
-
Treatment of post-traumatic hematoma and fibrosis using hyaluronidase injection2018 September;19(3)