A retrospective computed tomography analysis of maxillary fractures and the clinical outcomes of their unreduced parts
Article information
Abstract
Background
Some parts of a maxillary fracture—for example, the medial and posterior walls—may remain unreduced because they are unapproachable or hard to deal with. This study aimed to investigate the self-healing process of unreduced maxillary membranous parts of fractures through a longitudinal computed tomography (CT) analysis of cases of unilateral facial bone injuries involving the maxillary sinus walls.
Methods
Thirty-two patients who had undergone unilateral facial bone reduction surgery involving the maxillary sinus walls without reduction of the medial and posterior walls were analyzed in this retrospective chart review. Preoperative, immediate postoperative, and 3-month postoperative CT scans were analyzed. The maxillary sinus volume was calculated and improvements in bone continuity and alignment were evaluated.
Results
The volume of the traumatized maxillary sinuses increased after surgery, and expanded significantly by 3 months postoperatively (p< 0.05). The significant preoperative volume difference between the normal and traumatized sides (p= 0.024) resolved after surgery (p> 0.05), and this resolution was maintained at 3 months postoperatively (p > 0.05). The unreduced parts of the maxillary bone showed improved alignment and continuity (in 75.0% and 90.6% of cases, respectively), and improvements in bone alignment and bone continuity were found to be correlated using the Pearson chi-square test (p= 0.002).
Conclusion
Maxillary wall remodeling through self-healing occurred concomitantly with an increase in sinus volume and simultaneous improvements in bone alignment and continuity. Midfacial surgeons should be aware of the natural course of unreduced fractured medial and posterior maxillary walls in complex maxillary fractures.
INTRODUCTION
The paranasal sinuses have various functions. For instance, they reduce the weight of the skull by constituting areas of empty space in the skull. Additionally, active or passive ventilation of the paranasal sinuses can cool the brain [1], and specific pairs of the paranasal sinuses can control voice resonance, modulate intranasal gas pressure, and drain secretions from the mucosa of the nasal cavity through the mucociliary effect [2,3]. Furthermore, the paranasal sinuses serve as buffers against facial trauma, as they help distribute the force of external impacts. These sinuses also protect dental roots and the nasal cavity. However, because of the thin bony structures of maxillary sinuses— unlike the bones of the extremities—maxillary sinus fractures can easily occur due to external trauma [4]. Facial trauma is most commonly caused by violence, slipping and falling, traffic accidents, and sports activities [5].
Of the paranasal sinuses, the maxillary sinus is most commonly treated by oral and maxillofacial surgeons. Thus, having a solid understanding of the anatomical features and characteristics of this region is of fundamental importance. The maxillary sinus frequently has multiple cavities that are divided by several septa [6]. Rancitelli et al. [7] reported that 38.1% of the maxillary sinuses they investigated contained septa. It is also important to consider the distribution of the arterial supply to minimize postoperative complications [8-10]. Preserving special structures such as septa or the Schneiderian membrane and avoiding further injury of the arteries supplying the maxillary sinus are major concerns for surgeons.
Reduction techniques are commonly used to rebuild the original location and shape of the facial bone. However, some facial structures are difficult to approach, meaning that some parts of the fractures remain unreduced; for example, the medial and posterior walls of the maxillary sinus often cannot be reduced because of their location. It is widely accepted that only maxillary buttress reconstruction is sufficient for midface surgery. However, the natural course of unreduced fractured maxillary thin walls has not been clearly characterized. For this reason, we conducted this study to observe maxillary thin wall remodeling during the postoperative period.
The aim of this study was to investigate the self-healing process of unreduced midfacial bones through a longitudinal analysis of computed tomography (CT) scans of patients who underwent unilateral facial bone injuries involving the maxillary sinus walls.
METHODS
Study subjects
The subjects of this investigation were selected by chart review among patients who had undergone unilateral facial bone reduction surgery involving the maxillary sinus walls. All the patients had undergone surgery under general anesthesia by open reduction and internal fixation with titanium or absorbable plates and screws, without reduction of the medial and posterior walls of the maxillary sinus. The inclusion criteria were as follows: (1) no prior fracture history of the facial bones; (2) no old fracture identified on facial CT; (3) no history of maxillary sinusitis, wound infection, or further trauma during the 3-month postoperative period, as those conditions might affect the natural healing process after surgery; and (4) the availability of preoperative, immediate postoperative, and 3-month postoperative facial CT scans in their chart. To be more specific regarding the last inclusion criterion, not all of the patients received long-term postoperative facial CT follow-up. Long-term postoperative CT follow-up was only performed for patients who wanted their facial bone structures to be checked on CT. Scans were not obtained before 3 months postoperatively because bone healing might have still been taking place. The period between surgery and the long-term follow-up CT scans was between 3 months and 8 months, and 3-month postoperative CT scans accounted for the largest proportion of cases in the retrospective chart review. The exclusion criterion was bilateral midfacial fracture. The severity of the fracture, sex, age, mode of trauma, specific surgical technique, and involvement of other facial bone fractures were not considered. We had no exclusion criteria regarding the subtypes of zygomaticomaxillary complex fractures; therefore, all fracture types were included in the study.
CT analysis
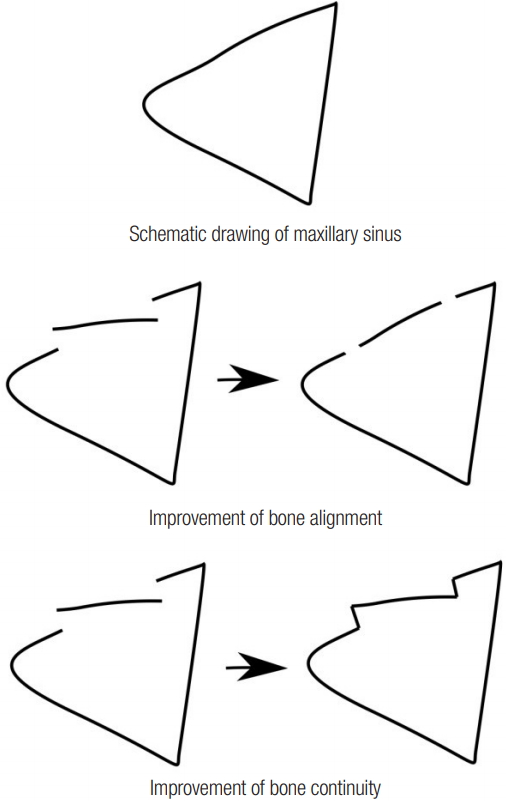
Maxillary sinus volume and improvements in bone alignment and continuity were compared on preoperative, immediate postoperative (within 2 weeks), and 3-month follow-up CT scans. To investigate the self-healing process of the unreduced maxillary sinus walls, CT volumetry was performed on both the injured and uninjured sides. For the injured side, preoperative, immediate postoperative, and 3-month postoperative volumetry was performed using the INFINITT PACS M6 software (INFINITT Healthcare Co., Ltd., Seoul, Korea). We calculated the maxillary sinus area two-dimensionally, and multiplied it by the thickness between each cut (3 mm) (Fig. 1). Technically, integral calculus was used to estimate maxillary sinus volume. The volume of both the injured and uninjured sides was calculated at the preoperative, immediate postoperative, and 3-month postoperative time points. Next, improvements in the bone alignment and bone continuity of the unreduced medial and posterior walls of the maxillary sinus were investigated by two plastic surgeons (HL and SWT) (Fig. 2). Bone alignment improvement was defined as a decrease in the extent of bony fragments, with a tendency for them to regain their original shape and linear contour. Bone continuity improvement was defined as the inability of the investigators to find the fracture line due to bone healing. Bone alignment and bone continuity improvement were graded as either improved or not improved. Improvement was only considered to have taken place if both investigators concurred.

Volumetric measurements made using the INFINITT PACS M6. The two-dimensional area of the axillary sinus was calculated in each image cut, and multiplied by 3 mm (the thickness between image cuts) to obtain the maxillary sinus volume (blue line).
Statistical analysis
Data were analyzed using SPSS for Windows version 24.0 (IBM Corp., Armonk, NY, USA). The level of statistical significance was set at p<0.05. The volume of the normal side was measured, and the volume of the traumatized side was measured at the preoperative, immediate postoperative, and 3-month postoperative time points. The pairwise difference between each category of volume measurements was analyzed using the paired t-test. The relationship between improvements in bone alignment and bone continuity was analyzed using the Pearson chi-square test.
Ethical approval
The study was approved by the Institutional Review Board of Hallym University Sacred Heart Hospital (IRB No. 2018-05-035-001) and performed in accordance with the principles of the Declaration of Helsinki.
RESULTS
Thirty-two patients (five men and 27 women) with preoperative, immediate postoperative, and 3-month postoperative facial CT data in their charts were included in this study. Their demographic features are shown in Table 1. Each category of volume measurements was defined as follows: NL, normal side volume; TS, traumatized side volume (preoperative); TSI, traumatized side volume (immediate postoperative); TS3, traumatized side volume (3 months postoperatively). The average maxillary sinus volume values were as follows: NL, 24.98±8.64 mL; TS, 23.10±8.00 mL; TSI, 25.09±7.88 mL; TS3, 25.49±8.06 mL (Table 2).
All possible pairs of the four categories of volume measurements were compared using the paired t-test (Table 3). TS was significantly smaller than NL by 1.88±4.47 mL (p=0.024), while the other two postoperative values (TSI and TS3) showed no significant difference compared to NL. Of the traumatized side values, TSI was larger than TS by 1.99±2.35 mL, TS3 was larger than TS by 2.39±2.23 mL, and TS3 was larger than TSI by 0.41±1.12 mL, all with statistical significance (p=0.000, p=0.000, p=0.048, respectively).
Twenty-four patients (75%) showed improved bone alignment 3 months after surgery, and 29 patients (90.6%) showed improved continuity during the same period (Fig. 3). A significant correlation was found between improvements in bone alignment and bone continuity by the Pearson chi-square test (p=0.002) (Table 4).
DISCUSSION
Maxillary thin wall remodeling was observed during the postoperative period. The volume of the traumatized maxillary sinuses expanded gradually after surgery, with statistical significance (p<0.05). Furthermore, the significant preoperative volume difference between the normal side and traumatized side (TS–NL, p=0.024) resolved after surgery (TSI–NL, p>0.05), and this recovery was maintained at 3 months postoperatively (TS3–NL, p>0.05). Furthermore, the unreduced parts of the maxillary bone showed improved alignment and continuity (in 75.0% and 90.6% of cases, respectively), meaning that the maxillary thin wall contour improved. In the statistical analysis, bone alignment and bone continuity were correlated with each other, implying that these two processes occurred simultaneously. Maxillary wall remodeling took place through self-healing in the patients analyzed in this study, with larger sinus volume and simultaneous improvements in bone alignment and continuity.
In the present study, the posterior lateral wall and medial wall of the maxillary sinus showed improvements despite not being surgically approachable. Additionally, the anterior wall, which is surgically approachable, showed a better contour at 3 months after surgery. One possible explanations for this self-healing process relates to the fact that facial bones heal by direct ossification of the mesenchyme, unlike the other bones of the skeleton, which healed via preformed cartilage through the process of endochondral ossification [11]. Osseous defect healing, bone regeneration, and the implant-bone interface have previously been investigated in a few articles [12-14]. Additionally, other factors can affect facial bone healing. Esteve-Altava and Rasskin-Gutman [15] claimed that bone in the craniofacial area is regulated by different genetic and epigenetic factors from those affecting other bones, resulting the presence of many cavities in the craniofacial area, including the paranasal sinuses. This mechanism of facial bone control through which injured cavities are restored may contribute to the self-healing process of facial bone fractures. Turning to other hypotheses, the amount of periosteum is much richer in the facial bone area than in other areas, which might contribute to bone healing. Claims have been made about the bone healing potential of the periosteum since the 17th century. Lin et al. [16] conducted molecular investigations into facial bone healing by the periosteum. Jung et al. [17] proposed a hypothesis according to which medial orbital wall remodeling takes place along its periosteum. The ratio of periosteum tissue to bone tissue of the facial bones is much higher than that of bones in the extremities [18]. This might contribute to self-healing of the membranous parts of the facial bones. Other factors, such as positive air pressure from sinus ventilation and muscle actions such as posterior pulling by the pterygoid muscles, may help the self-healing process. Paranasal sinus pressure rises during expiration [19]. The lower head of the lateral pterygoid muscle and the deep head of the medial pterygoid muscle originate from the lateral pterygoid plate and may be able to affect the location of the fragmented posterior maxillary wall. These actions might have contributed to the increase in maxillary volume observed 3 months after surgery.
Maxillofacial reconstruction surgery focuses on rebuilding the original shape of the affected region [20]. All functions of the upper jaw—including ventilation through the paranasal sinus system, chewing, biting, and swallowing—are associated with the original shape of the maxillary bone [20,21]. Maxillary and zygomaticomaxillary complex fracture reduction focuses on restoring the malar prominence, zygomatic arch, and maxillary buttresses [22]. The results of the present study imply that even unreduced parts can heal spontaneously if the fractured part is membranous. Therefore, surgeons should be aware that the self-healing process will continue after surgery. For this reason, meticulous reduction of small fragments of the fractured thin wall may not be necessary, and instead it may be better to focus on preserving the periosteum, which induces self-healing. Furthermore, dealing with these fragmented parts may increase the risk of iatrogenic injury of the original anatomical features. It is easy to injure the maxillary septa and arteries distributed around and inside the maxillary sinus because of limited visibility. Iatrogenic injuries of these structures may increase the complication rate [23,24].Therefore, concentrating on reducing the buttress and preserving the periosteum would be much more important for promoting self-healing at thin wall fracture sites.
This study has some limitations. Volume does not inherently provide any information on the shape of the maxillary sinus. Even though the data confirmed volumetric expansion of the fractured site after reduction, this does not technically mean that the shape improved. The evaluation of bone continuity and alignment play supplementary roles in this regard; nonetheless, the data on these parameters relied on a subjective analysis (albeit by facial bone experts). Other limitations include the issue that because of the retrospective nature of this study, functional aspects of the maxillary sinus, such as voice pitch, brain temperature (which might be affected by maxillary sinus ventilation), and the mucociliary effect could not be quantified. Further studies incorporating both structural and functional analyses could guide surgeons who operate on midface fractures.
In conclusion, a longitudinal analysis of CT scans demonstrated maxillary wall remodeling through self-healing, with a concomitant increase in the maxillary sinus volume and simultaneous improvements in bone alignment and continuity. It is clear that fractured maxillary thin walls in cases of complex maxillary fractures go through a natural course of healing.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Hallym University Sacred Heart Hospital (IRB No. 2018-05- 035-001) and performed in accordance with the principles of the Declaration of Helsinki.