|
 |
- Search
| Arch Craniofac Surg > Volume 20(6); 2019 > Article |
|
Abstract
Salivary gland tumors usually appear in solitary mass in single salivary gland. The coexistence of tumors with different histological types occurring within a unilateral parotid gland is an extremely rare event. We experienced a case which two different types of malignant tumors developed at different time points in same gland; metachronous tumors. The second tumor was excised widely and reconstruction was performed by free tissue transfer. Sensory and motor nerve to the left cheek appeared to be intact, and circulation was adequate. This rare case was presented in this article.
Although salivary gland tumors typically appear in the form of a singular mass restricted to a unilateral salivary gland, there are extremely rare cases that involve the development and coexistence of tumors with different characteristics [1]. The coexistence of tumors with different histological types occurring within a unilateral parotid gland is an extremely rare event, and found in <0.3% of all salivary gland neoplasms [2]. Although rarely observed, there have been cases of multiple tumor development in the salivary glands, which are mostly synchronous tumors. Synchronous tumors are defined by the development of Ōēź2 tumors at the same time, while metachronous tumors develop at different time points.
Ipsilateral development of metachronous malignant tumors of two different types is an extremely rare event and, to the best of our knowledge, there are few, if any reports in the literature describing this entity. In the present article, we report our experience with a patient who had been previously diagnosed with a single malignant tumor in the parotid gland and underwent parotidectomy, but was diagnosed with a different malignant tumor at the same location approximately 20 years later, which we introduce under the concept of multiple tumors.
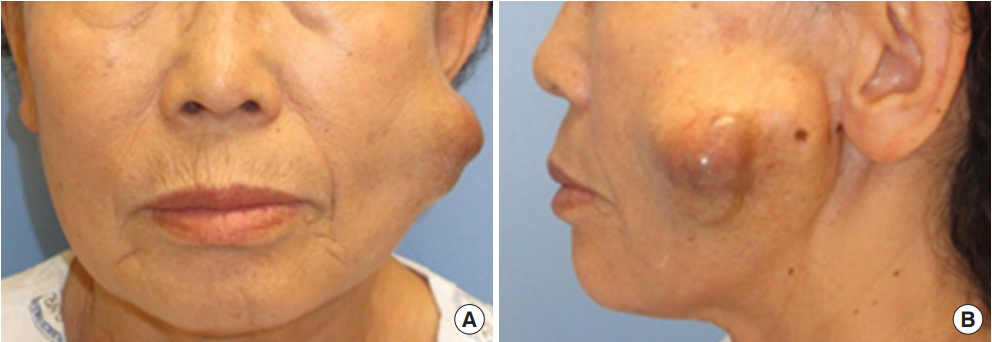
A 69-year-old female had been visiting the authorsŌĆÖ center for approximately 1 year with a protruding mass on the left cheek area, which had been growing in size (Fig. 1). The patient had also developed a similar left cheek mass approximately 20 years previously, which was suspected to be benign and was excised at a different center. The follow-up biopsy indicated that the mass was an epithelial-myoepithelial carcinoma (EMC).a type of malignant tumor; consequently, the patient underwent additional total parotidectomy. The patient was determined to be in complete remission and was lost to follow-up without requiring additional treatment.
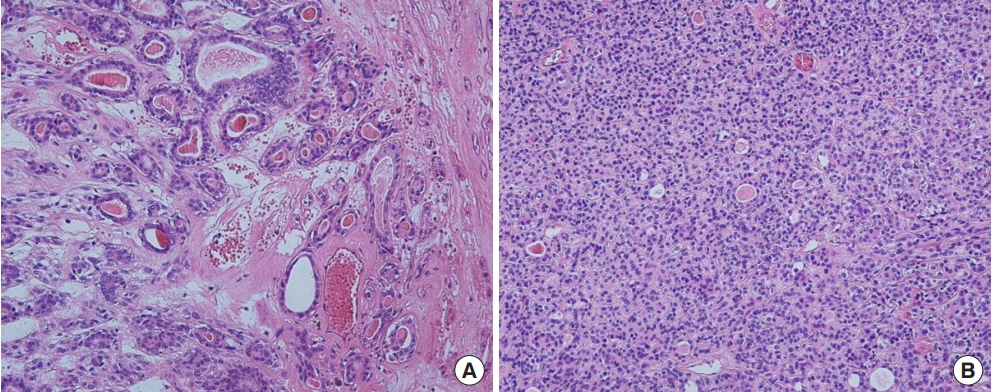
Approximately 20 years later, however, the patient visited the Seoul St. MaryŌĆÖs Hospital with a mass on the left cheek area that had been growing in size over the past year. From physical examination, a firm, non-tender, irregular shape mass, approximately 6├Ś6 cm in size, was palpated; her facial nerve function was intact. Furthermore, there was an accompanying discolored skin lesion in the upper part of the mass. Preoperative magnetic resonance imaging confirmed the presence of a welldefined mass, 2.6├Ś4.6├Ś4.6 cm in size, in the left masticator space, which consisted of solid and cystic parts with infiltration from the masticator muscle to the dermal layer (Fig. 2). Gross total resection of the lesion was performed with a safety margin of 1cm, followed by reconstruction of the wound with exposed facial nerve using an anteromedial thigh free flap. Based on histopathological analysis, the patient was diagnosed with basal cell adenocarcinoma (BCAC), and immunohistochemistry confirmed that the lesion was CD117, p63, SMMHC (smooth muscle myosin heavy chain), and p40 positive (Fig. 3).
The patient underwent radiotherapy thereafter. At the 12-month follow-up, the patient had not experienced recurrence or metastasis, and the operative wound was stable (Fig. 4).
There may be occasional development of multiple tumors in the salivary glands, which account for 1.7% to 5% of parotid lesions [3]. The case we encountered can be explained by the concept of extremely rare multiple tumor development involving the metachronous onset of two distinct primary malignant tumors, EMC and BCAC, arising from the same location with a 20-year gap between the two onsets. Nonetheless, the medical records from the initial EMC were incomplete, and there may have been residual gland tissue despite total parotidectomy. Metachronous development of BCAC 20 years later most likely originated from this previous lesion. Although there is a record of total parotidectomy performed 20 years ago at another hospital record, it is not clear exactly whether it was completely resected due to lack of data. However, if the pathology of the tumor that occurred 20 years later showed a tumor with a new character, it could be assumed that there was no remnant lesion of tumor but a new tumor occurred in the same location.
The most common forms of these tumors exhibiting a histological combination include Warthin tumors and pleomorphic adenoma [4]. These multiple tumors, demonstrating two distinct characteristics from a unilateral parotid neoplasm, can be differentiated into either synchronous or metachronous tumors [5]. While synchronous tumors are characterized by the development of more than one tumor at the same time, these tumors are separated by tumor-free salivary gland tissue [6]. In these cases, the tumor may be easily confused with a hybrid tumor, which is different because this tumor has identical origin at the same topographical area but exhibits >2 different histological types [7]. Meanwhile, metachronous tumors arise at different time points, although there is no clearly established standard for time periods. Previous studies have suggested that for multiple tumors, metachronous (30%) tumors are much less common than synchronous (70%) tumors [4]. Franzen et al. [4] reviewed 796 medical records of 758 patients who underwent parotidectomy over a 40 year-period, and reported that 13% of these patients had multiple tumors. These tumors were more often unilateral than bilateral, and synchronous than metachronous. The most common forms observed were unilateral and synchronous Warthin tumors and pleomorphic adenomas. All cases of metachronous tumors were found to be contralateral.
Among tumors originating from the salivary gland(s), EMC and BCAC are rarely observed low-grade malignant tumors, which often arise from the parotid gland. In 1991, these were classified as independent diseases under the World Health Organization classification [8]. EMC has biphasic pathological characteristics involving variable proportions of two distinct cell types. More specifically, the inner layer of ductal-lining exhibits characteristics of epithelial-type cells while the outer layer exhibits characteristics of clear, myoepithelial type cells. In this tumor, local recurrence rates is ranging from 23% to 80%, an incidence of metastasis is reported to be about 14% and a death rate is reported to be as high as 40% in literature [9]. BCAC has characteristics of basaloid cell proliferation similar to basal cell adenoma (BCA), but is different from BCA in that it exhibits necrosis or mitoses, as well as invasive activity such as capsular invasion. Wilson and Robinson [10] reported that BCAC recurred at a rate of 16.7% and uncommonly metastasized and rarely even causes death. Cases involving co-occurrence of EMC and BCAC are extremely rare. Franzen et al. [4] reported a case involving a 70-year-old man diagnosed with EMC, BCAC, and adenoid cystic carcinoma in a single mass on his right parotid gland, and another similar case involving EMC and BCAC simultaneously diagnosed in a single parotid gland tumor. However, the main difference in these previous cases is that they involved a hybrid tumor of a single mass at an identical anatomical location.
Both BCAC and EMC do not have defined treatment guidelines due to their low prevalence. Nevertheless, we have established a treatment protocol after reviewing several case reviews. In our patient, the size of the tumor was relatively large (4.4├Ś4.0├Ś1.9 cm) and, thus, was relatively high stage (T3), and infiltrated the skin and buccalis muscle. Accordingly, surgical excision of the tumor was performed. In addition, because both tumors are reported to have high risks for locoregional recurrence, despite the low risk for metastasis, additional radiation therapy was performed. To date, after 12 months of follow-up, the patient does not exhibit any signs of recurrence.
Notes
REFERENCES
1. Whitt JC, Schafer DR, Callihan MD. Multiple malignant salivary gland neoplasms: mucoepidermoid carcinoma of palate and adenoid cystic carcinoma of floor of mouth. Head Neck Pathol 2008;2:41-8.



2. Curry JL, Petruzzelli GJ, McClatchey KD, Lingen MW. Synchronous benign and malignant salivary gland tumors in ipsilateral glands: a report of two cases and a review of literature. Head Neck 2002;24:301-6.


3. Ochal-Choinska A, Bruzgielewicz A, Osuch-Wojcikiewicz E. Synchronous multiple unilateral parotid gland tumors of benign and malignant histological types: case report and literature review. Braz J Otorhinolaryngol 2019;85:388-92.


4. Franzen AM, Coordes A, Franzen CK, Guenzel T. Are multiple tumors of the parotid gland uncommon or underestimated? Anticancer Res 2017;37:5263-7.

5. Ethunandan M, Pratt CA, Morrison A, Anand R, Macpherson DW, Wilson AW. Multiple synchronous and metachronous neoplasms of the parotid gland: the Chichester experience. Br J Oral Maxillofac Surg 2006;44:397-401.


6. Bae YK, Kim DS, Suh JS, Ro JY. Combined epithelial-myoepithelial carcinoma and basal cell adenocarcinoma of the parotid gland: a case report. Korean J Pathol 1999;33:453-6.
7. Sabri A, Bawab I, Khalifeh I, Alam E. Hybrid tumor of the parotid gland: a case report and review of the literature. Case Rep Otolaryngol 2015;2015:192453.




8. Zhan KY, Lentsch EJ. Basal cell adenocarcinoma of the major salivary glands: a population-level study of 509 cases. Laryngoscope 2016;126:1086-90.


- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 3,512 View
- 65 Download
- Related articles in ACFS