|
 |
- Search
| Arch Craniofac Surg > Volume 21(5); 2020 > Article |
|
Abstract
Side effects of tattoos can occur due to unexpected body responses. Concerns about the side effects of tattoos are growing concomitantly with the increasing number of tattooed individuals. We report a rare case of basal cell carcinoma (BCC) on a tattooed eyebrow. A 48-year-old woman with no family history or occupational risk of skin cancer had her eyebrows tattooed 6 years prior, and she noticed a black mass on her right eyebrow 1 year before presentation. Staged excision was planned due to the patientŌĆÖs reluctance regarding the possibility of a wide scar. After the first surgical procedure, a histopathological examination confirmed BCC. Wide excision and primary closure were performed for remnant BCC, and no recurrence was observed. The mechanism of skin neoplasms involving tattoos has not been clearly identified. Unapproved tattoo inks contain carcinogenic substances, and previous case reports indicate that skin neoplasms may differ depending on the tattoo color. Therefore, the carcinogenic effects of these unknown components of tattoo ink might cause skin neoplasms. Accurate component analysis and systematic management of tattoo ink is necessary, and medical practitioners must also pay attention to this possibility because it is easy to overlook tattoos as a causal factor contributing to cancer.
The number of tattooed individuals is gradually increasing. A report from the Korea Ministry of Food and Drug Safety in 2018 estimated that 3 million tattoos on the trunk and limbs and 10 million semi-permanent tattoos on the eyebrows and lips had been performed. Therefore, the side effects of tattoos have emerged as an issue of growing concern. Tattooing can be defined as the insertion of pigment into the dermis using an instrument, and the inserted foreign material may cause complications such as implantation caused by trauma, infection, and various body reactions to the pigments [1]. We report a rare case of basal cell carcinoma (BCC) in a tattooed eyebrow.
A 48-year-old woman presented with a dark-colored mass in her right eyebrow that had been present for 1 year. She had acquired permanent tattoos on both eyebrows with black colorant 6 years previously for cosmetic reasons at an unlicensed beauty shop. The mass measured 1.2├Ś0.7 cm, had the appearance of a bunch of grapes, was black-colored and hard-textured, and had grown beyond the boundaries of the black tattoo pigment (Fig. 1). She had no relevant family or medical history. Her job involved working indoors, without abundant sunlight exposure.
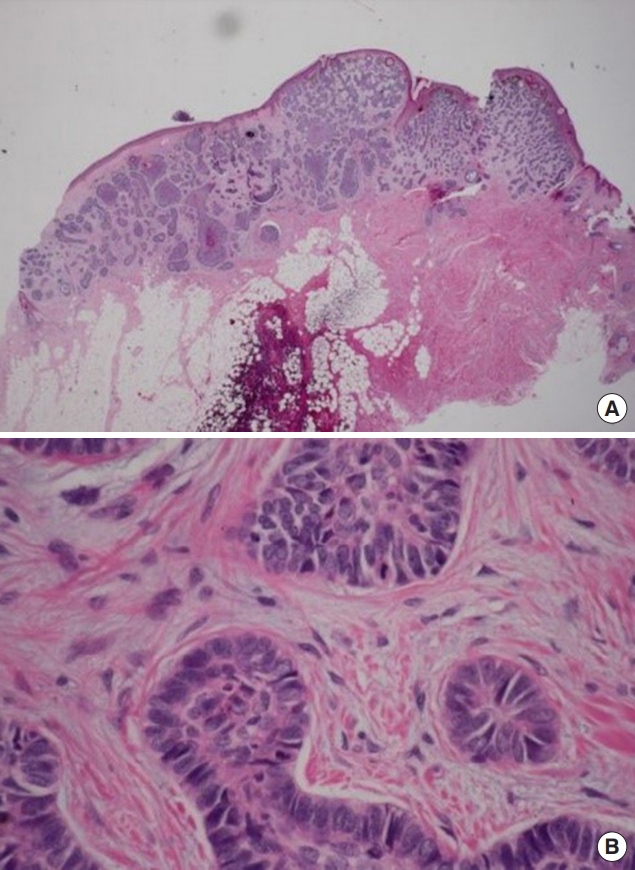
The patient was very reluctant regarding the possibility of a broad scar after wide excision. Since BCC rarely metastasizes, a staged excision was planned, with the possibility of additionally performing wide excision in the second procedure depending on the histopathological results of the first operation. The firststage excision was performed, removing most of the mass, and she was diagnosed with BCC based on a histopathological examination (Fig. 2). After 2 months, wide excision and primary closure were performed for the remnant BCC (Fig. 3). On histopathological examination, a clear margin was obtained, and there was no lymphovascular invasion. No recurrence was observed after 3 years of follow-up (Fig. 4).
Since the first report by Bashir [2] in 1976 of the occurrence of BCC in a tattooed area, several cases have been reported. The current report presents the second known case of BCC in a tattooed eyebrow [3], according to a literature search in PubMed with the search terms ŌĆ£basal cell carcinoma,ŌĆØ ŌĆ£tattoo,ŌĆØ and ŌĆ£eyebrow.ŌĆØ In the previous report of BCC on a tattooed eyebrow [3], the tumor had the shape of a depressed patch with the same color as the skin, whereas the mass described in the current report was protruding, with the shape of a bunch of grapes, and was black. In addition, the mass in the previous report was treated with Mohs micrographic surgery with a BurowŌĆÖs graft. In that case, there was no hair at the graft site, so camouflage with a black eye pencil was required to obtain an aesthetically acceptable outcome. However, in our case, by performing staged excision, only a linear scar remained at the surgical site, resulting in excellent aesthetic results. Most previous cases of BCC have been reported in individuals older than 60 years of age. Advanced age is generally known to be a risk factor for skin cancer [4]; thus, the causal relationship with tattoos is less evident in older patients. In the current case, the causality appeared to be clearer because the neoplasm occurred in a relatively young female patient with no relevant risk factors.
The mechanism through which tattoos cause skin neoplasms has not been fully elucidated, although some possibilities have been proposed. First, traumatic skin puncture by needles may cause skin neoplasms in combination with the persistent inflammatory response to foreign substances. These trauma-induced cases usually appear rapidly, within a year of tattooing [5]. Other proposed mechanisms include the direct injection of carcinogenic substances in the process of tattooing, changes in the absorption of ultraviolet (UV) rays, and chronic local inflammatory conditions. In addition to BCC, several cases of other skin neoplasms such as squamous cell carcinoma and melanoma, which are more likely to metastasize, have been reported in areas that have been tattooed [6,7]. In these cases, it seems that prompt diagnosis and treatment are needed to reduce the risk of metastasis. In previous case reports of skin neoplasms in tattooed areas, melanoma and BCC occurred in black or dark blue tattoos, and squamous cell carcinoma and keratoacanthomas occurred mostly in red tattoos [6]. This discrepancy supports the possibility that carcinogenic effects are caused by unknown components present in the colorants of tattoos. The exact composition of tattoo ink is not systematically managed, although tattoo ink is known to contain aluminum, titanium, carbon, mercury, cadmium, and allergenic metals, such as chromium, nickel, and cobalt. Mercury, cobalt sulfate, and carbon black are classified as group 2B (possibly carcinogenic to humans) and cadmium is classified as group 1 (carcinogenic to humans) [6]. In addition, byproducts that are carcinogenic to animals that are not present in the initial ink can appear after exposure to UV or laser rays [6]. In the component tests of 14 commercially available black inks, dibutyl phthalate, a softener, was extracted from all inks, as well as other substances such as hexachloro-1,3-butadiene, dibenzofuran, benzophenone, hexamethyl benzene, and hexamethylenetetramine [8]. These ingredients are genotoxic, teratogenic, and/or carcinogenic substances. According to European market studies, currently commercially available tattoo inks contain azo pigments or polycyclic compounds, and 60% of organic colorants in tattoo ink are azo compounds classified as carcinogenic substances [6]. Thus, unapproved tattoo ink contains several substances that have not been proven safe.
In addition to skin neoplasms, tattoos can cause various complications such as anaphylaxis, uveitis, pseudolymphoma, granulomatous reactions, infections (hepatitis B and C, human immunodeficiency virus, herpes simplex virus, and syphilis), skin infections, necrotizing fasciitis, magnetic resonance imagingŌĆōassociated burns, and keloid scar formation [1]. Tattoos are becoming increasingly popular, but their complications range from mild to life-threatening. Therefore, tattooists, patients, and healthcare providers must be aware of tattoo-related complications, and education on infections and prevention is essential.
Tattoo procedures are often performed illicitly by unlicensed personnel, and safety management and complication monitoring should be carried out. In addition, accurate analyses of the components of unapproved tattoo ink should be performed, and strict systematic management is necessary in the future. Skin neoplasms usually occur several years after tattooing; therefore, it is easy for healthcare providers to overlook the association with tattoos. For this reason, medical practitioners should consider the causal relationship of skin neoplasms with tattoos by conducting accurate inquiries and establishing appropriate diagnoses and treatment plans.
Notes
Fig.┬Ā1.
A 48-year-old woman with basal cell carcinoma in the right eyebrow. An irregularly protruding, darkly-colored basal cell carcinoma measuring 1.2├Ś0.7 cm is observed in a tattooed eyebrow.

REFERENCES
1. Petrochko JM, Krakowski AC, Donnelly C, Wilson JB, Irick JB, Stawicki SP. Tattoo-associated complications and related topics: a comprehensive review. Int J Acad Med 2019;5:19-50.

3. Lee JS, Park J, Kim SM, Yun SK, Kim HU. Basal cell carcinoma arising in a tattooed eyebrow. Ann Dermatol 2009;21:281-4.



4. Han SH, Kim SH, Kim CK, Jo DI. Multiple nonmelanocytic skin cancers in multiple regions. Arch Craniofac Surg 2020;21:188-92.




5. Maxim E, Higgins H, DŌĆÖSouza L. A case of multiple squamous cell carcinomas arising from red tattoo pigment. Int J Womens Dermatol 2017;3:228-30.



- TOOLS
-
METRICS

-
- 2 Crossref
- Scopus
- 4,620 View
- 99 Download
- Related articles in ACFS
-
Giant basal cell carcinoma of the left lateral neck2021 June;22(3)
Sebaceous carcinoma arising from sebaceoma2021 April;22(2)
Two separate nodules of Merkel cell carcinoma occurring concomitantly on one cheek2019 June;20(3)