Endoscopic slide-in orbital wall reconstruction for isolated medial blowout fractures
Article information
Abstract
Background
This study evaluated the efficacy of the endoscopic medial orbital wall repair by comparing it with the conventional transcaruncular method. This surgical approach differs from the established endoscopic technique in that we push the mesh inside the orbit rather than placing it over the defect.
Methods
We retrospectively reviewed 40 patients with isolated medial orbital blowout fractures who underwent medial orbital wall reconstruction. Twenty-six patients underwent endoscopic repair, and 14 patients underwent external repair. All patients had preoperative computed tomography scans taken to determine the defect size. Pre- and postoperative exophthalmometry, operation time, the existence of diplopia, and pain were evaluated and compared between the two methods. We present a case showing our procedure.
Results
The operation time was significantly shorter in the endoscopic group (44.7 minutes vs. 73.9 minutes, <i>p</i>= 0.035). The preoperative defect size, enophthalmos correction rate, and pain did not significantly differ between the two groups. All patients with preoperative diplopia, eyeball movement limitation, or enophthalmos had their symptoms resolved, except for one patient who had preexisting strabismus.
Conclusion
This study demonstrates that endoscopic medial orbital wall repair is not inferior to the transcaruncular method. The endoscopic approach seems to reduce the operation time, probably because the dissection process is shorter, and no wound repair is needed. Compared to the previous endoscopic method, our method is not complicated, and is more physiological. Larger scale studies should be performed for validation.
INTRODUCTION
Isolated medial wall fracture is the most common type of orbital blowout fracture [1]. Conventionally, isolated medial orbital wall fractures are treated surgically through a transcaruncular incision, if indicated. The endonasal endoscopic approach, which was first introduced by Yamaguchi et al. in 1991 [2], is also a popular method. However, comprehensive studies comparing endoscopic and transcaruncular approaches are rare. In this series, the mesh was trimmed to match the defect size after computed tomography (CT) evaluation and then inserted into the orbital space, which we named the “slide-in” technique. This approach differs from previously known endoscopic methods, where the implants were placed in the ethmoid space. We aimed to study the efficacy of this approach by comparing the outcomes of patients who underwent medial orbital wall repair through the transcaruncular approach with that of those who underwent this new technique.
METHODS
The institutional review board approved this study (IRB No. B-1905/540-107). Patients with isolated medial orbital wall fractures who received either endoscopic or transcaruncular medial orbital wall reconstruction between June 2013 and March 2019 at Seoul National University Bundang Hospital were reviewed. All surgeries were performed by a single surgeon (BKK) within 2 weeks of the injury. The indication for surgery was a defect size of at least 1 cm2, or significant herniation of orbital tissue upon the preoperative CT scan. Before June 2018, our treatment protocol was transcaruncular repair. All patients who underwent surgery in June 2018 or later underwent endoscopic repair. The surgeries were performed in an elective manner, rather than emergency, to allow the swelling to decrease and facilitate the operation. Patients were discharged on the same day or the day after the operation.
All patients underwent preoperative CT scans to diagnose the fracture and measure the defect size. All patients received preand postoperative ophthalmologic examinations including exophthalmometry, diplopia tests, and extraocular movement examinations. Subjective pain was measured using the numeric rating scale (NRS), and the average score on the day of operation was calculated. All patients who underwent the endoscopic approach had postoperative CT scans taken to confirm appropriate reduction. The patients were followed up for at least 6 months.
In both approaches, Synpor porous polyethylene implants (Depuy Synthes; Johnson and Johnson, New Brunswick, NJ, USA) were used for reconstruction. In the endoscopic approach, after packing epinephrine-soaked gauzes for 5 minutes, the middle turbinate was pushed aside. After injecting local solution, the incision was made at the uncinate process. Dissection was performed through the ethmoid space to reach the medial orbital wall. A Synpor mesh was trimmed to be about 2 mm larger in length and breadth compared to the defect size measured via the preoperative CT scan, and then pushed into the orbit starting from the posterior side, the superior and inferior borders, and then the anterior part of the mesh. Then, the middle meatus was packed with epinephrine-soaked gauzes (Fig. 1, Supplementary Video S1). Operation time was measured from the moment of local solution injection until the final nasal packing.
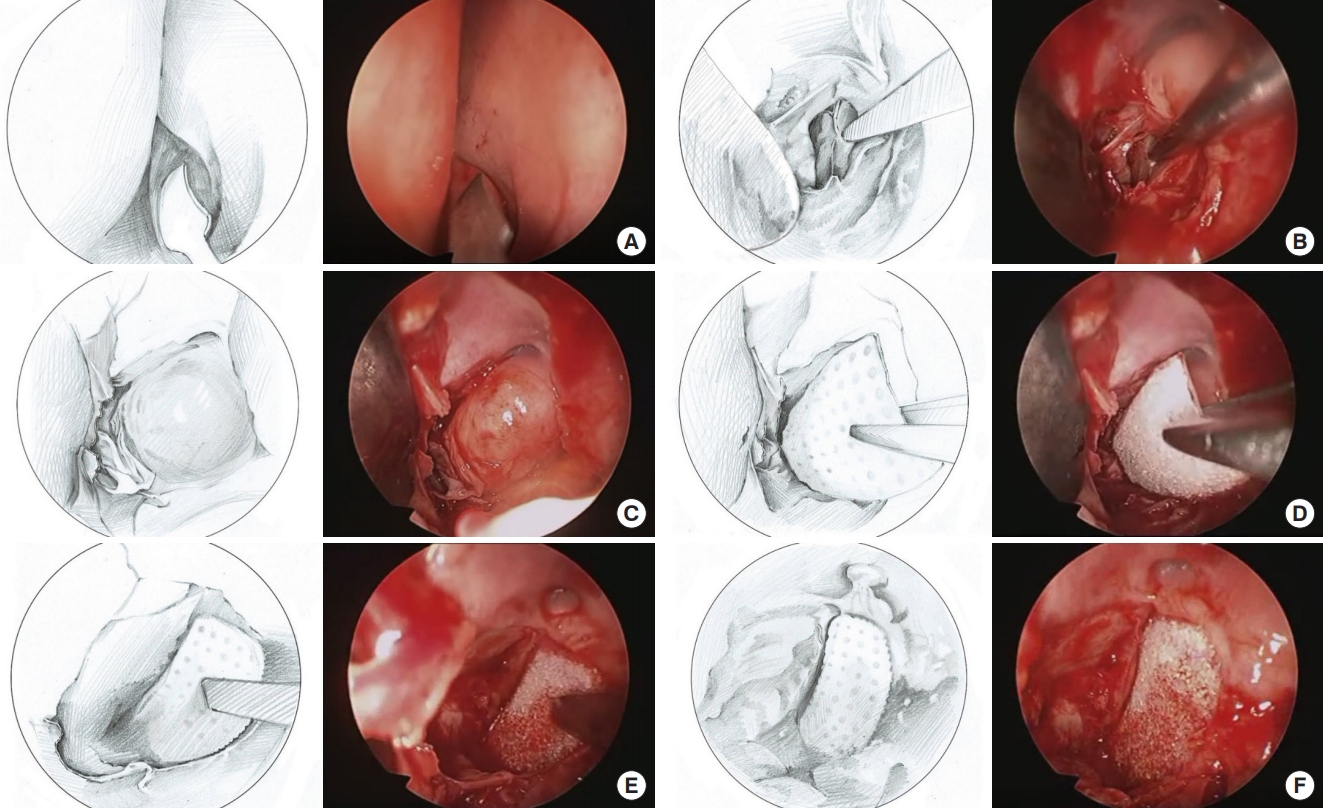
Graphical depiction of the surgical procedure. (A) The incision is made through the uncinate process. (B) Dissection is done through the ethmoid space to reach the medial orbital wall. (C) The herniated orbital content through the fractured wall is visualized. (D) The Synpor mesh is pushed into the orbit starting from the posterior side, (E) then the superior and inferior borders, and lastly, the anterior part of the mesh. (F) The Synpor mesh is in place, adequately blocking any orbital content herniation.
Enophthalmos of at least 2 mm relative to the lateral orbital rim was considered as positive for enophthalmos. Marco prism exophthalmometer (Marco, Jacksonville, FL, USA) was used for measurement. The enophthalmos correction rate was deduced by subtracting the preoperative degree of enophthalmos from the postoperative degree of enophthalmos, both in millimeters. For example, if a right-sided patient’s pre- and postoperative exophthalmometry results were 16/18 and 18/18, respectively, then the enophthalmos correction rate is ([18-16]–[18-18]=2).
Non-paired t-tests were used to compare the operation time, defect size from the preoperative CT scan, enophthalmos correction rate, and pain between the two groups. A p-value of less than 0.05 was considered statistically significant.
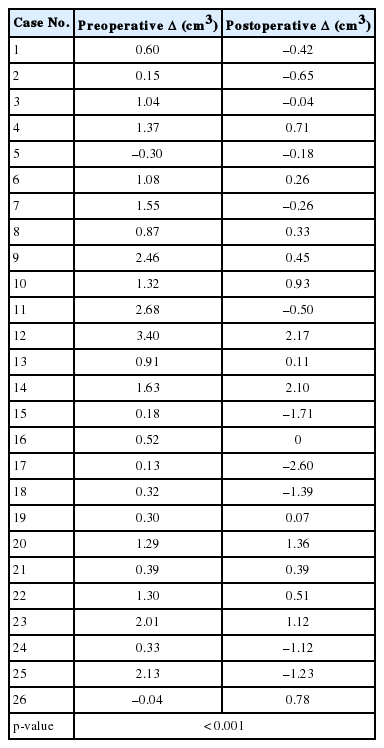
The difference in orbital volume between the injured and normal sides (Δ, in cm3) was compared pre- and postoperatively for the endoscopic group, and analyzed using the paired t-test.
RESULTS
We recruited 40 patients in our study. Twenty-six patients underwent endoscopic repair, whereas 14 underwent reconstruction via the transcaruncular approach. Thirty-three of the patients were men, and seven were women (Table 1). Twenty patients each had fractures on the right and left side. Fourteen patients had accompanying nasal bone fractures, but none had naso-orbito-ethmoidal fractures.
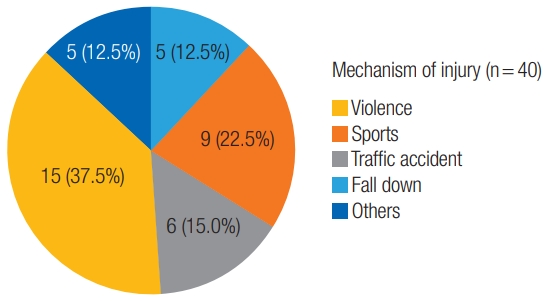
The most common mechanism of injury was violence, accounting for 15 patients (37.5%). The second most common was sports, accounting for nine patients (22.5%). Six patients (15%) were injured in traffic accidents, and five patients (12.5%) had injuries from falling down (Fig. 2).
The average preoperative defect sizes were 265.2 mm2 and 276.4 mm2 for the endoscopic and transcaruncular groups, respectively, and did not significantly differ (p=0.73).
Three patients in the endoscopic group had preoperative diplopia. This completely resolved in two patients, and persisted in the other patient, possibly because of his preexisting strabismus. Three patients in the transcaruncular group had preoperative diplopia, which completely resolved after the operation. The number of patients who had preoperative extraocular movement restriction in the endoscopic group and the transcaruncular group was three and two, respectively. The symptoms subsided in all patients after surgery. In the endoscopic group, two patients had preoperative enophthalmos greater than 2 mm, which resolved postoperatively. No patients had preoperative enophthalmos in the transcaruncular group (Table 2).
The average operation time was 44.73 minutes in the endoscopic group, which was significantly shorter than that in the transcaruncular group which was (73.93 minutes, p<0.05). The average enophthalmos correction rate was 0.405 in the endoscopic group, and 0.192 in the transcaruncular group. This difference was not significant (p=0.32). The average NRS pain scores of the endoscopic and transcaruncular groups were 2.84 and 2.69, respectively, which were not significantly different (p=0.64) (Table 3).
Supplementary Tables S1 and S2 summarize the demographics, postoperative findings, and results of the patients for each group.
All patients who underwent the endoscopic approach had their fractures appropriately reconstructed according to the postoperative CT scans. Most preoperative Δ values were positive, indicating that the fractured sides had larger orbital volumes compared to the normal sides. However, most of the postoperative Δ values were smaller than the preoperative Δ values, many of which were negative, and this difference was statistically significant (p<0.001) (Table 4).
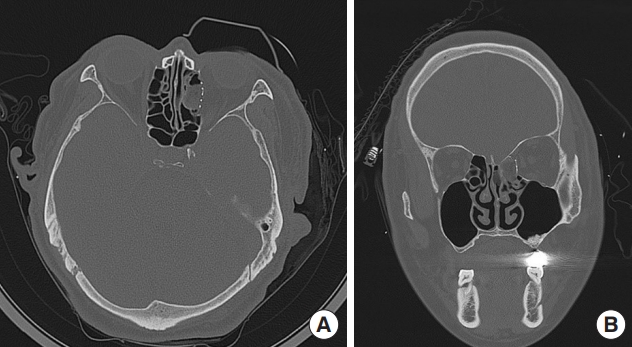
Figs. 3 and 4 show the pre- and postoperative CT scans of a patient who underwent endoscopic slide-in reconstruction. He had no preoperative symptoms and the preoperative exophthalmometry result was normal (11/11 [93]). However, the defect size was quite large (22×10 mm2), requiring surgical reconstruction. The operation time was 33 minutes, and there were no postoperative complications. The immediate postoperative CT scan showed adequate reduction and reconstruction of the medial wall (Fig. 4). The patient showed no diplopia or enophthalmos on his last outpatient visit 7 months postoperatively.
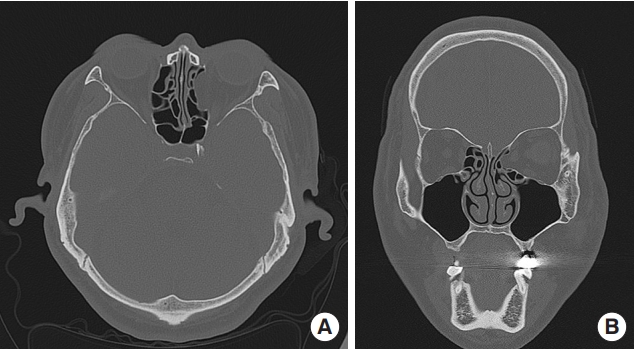
Preoperative computed tomography (CT) scan of a patient. A CT scan was obtained for further evaluation, which revealed a medial orbital wall fracture on the left side. He had no preoperative symptoms, and the preoperative exophthalmometry result was normal (11/11 [93]). However, the defect size was considerably large (22×10 mm2), and therefore, surgical reconstruction was performed using the endoscopic slide-in method. Axial view (A) and coronal view (B).
Postoperative computed tomography (CT) scan of an example patient. The operative time was 33 minutes, and there were no postoperative complications. The immediate postoperative CT scan showed adequate reduction and reconstruction of the medial wall. The patient had no diplopia or enophthalmos on his last outpatient visit 7 months postoperatively. Axial view (A) and coronal view (B).
DISCUSSION
The transcaruncular approach for medial orbital wall reconstruction is one of the most commonly used methods because it is safe and effective and leaves minimal cosmetic deficits. However, this approach has several drawbacks and potential side effects such as injury to the globe or the delicate structures of the lacrimal system. Muscle traction that results in muscle edema and diplopia can occur while “pulling” the herniated tissue into the orbit. Because the operation is performed in the intraorbital space, hemorrhage may occur in the ethmoid space. The visual field is also narrow through the transcaruncular approach.
To overcome these disadvantages, surgeons have attempted to find a better approach. Since its introduction by Yamaguchi et al. in 1991 [2], endonasal endoscopic repair has become a popular method for medial orbital wall reduction and/or reconstruction. A few studies have suggested that the results of endoscopic repair are qualifiable [2,3]. However, they did not provide a comparison with the external method.
Other studies comparing the two methods concluded that the endoscopic method was not inferior to the external method [4-8]. Endoscopic repair in these studies placed Merocel, Medpor implants, or silastic sheets in the ethmoid space to maintain reduction. Our study differed from these previous studies in that we placed a Synpor mesh into the orbit rather than placing the implant in the ethmoid cavity. We hypothesized that this would provide a more stable reduction state and prevent implant migration. Our results revealed that the slide-in endoscopic repair was not inferior to the transcaruncular method. However, a comparison with previous endoscopic techniques was not performed, although it would have provided a more direct analysis. We decided that the comparison with the external method was enough to prove the efficacy and safety of our endoscopic method.
In contrast to a study by Han et al. [6], the operation time was significantly shorter using the endoscopic approach. In the earlier period of endoscopic usage, the operation time was longer than the average operation time of the transcaruncular method. However, as the operator became skilled in the endoscopic method, the operation time of the endoscopic method was substantially shortened. We suggest that once the operator becomes skilled, the endoscopic method can save time, which is probably because the dissection process is shorter and wound repair is unnecessary.
To confirm appropriate reduction with our new method, all 26 patients who underwent the endoscopic approach had postoperative CT scans taken. All postoperative scans revealed appropriate reduction of the medial wall. We analyzed the preand postoperative orbital volumes to add credibility to the results. The difference between the preoperative and postoperative orbital volumes was much larger in the injured side than in the normal side, implying a significant reduction in orbital volume after the operation. This suggests that endoscopic repair successfully reduced the herniated tissue back into the orbit. One pitfall was that we did not take postoperative CT scans of the patients who underwent the transcaruncular approach. Although obtaining them would have provided a better comparison between the two methods, additional scans seemed less likely to benefit these patients.
Our study also included a new factor, pain, which was not included in any other study, to the best of our knowledge. Although the NRS pain score is a subjective measure, we demonstrated that the endoscopic method is not more painful than the external approach.
The incidence of pre- or postoperative symptoms, including diplopia, restriction of movement, and enophthalmos, were lower than in previously reported studies [1,3,4,6,8]. This was probably because the operations were performed a few days after the injury, giving time for the swelling to subside.
From our experience, the endonasal endoscopic slide-in technique for medial orbital wall reconstruction is less invasive, and is easier to approach as the dissection procedure is simple. The surgeon has a more detailed close-up vision, and it is more educational as the surgeon’s vision is shared with everybody in the operating room. The procedure is more anatomical since the reduction takes place by pushing the herniated objects, rather than by pulling the tissue into the orbit. It is also much faster as the simpler dissection process and absence of wound repair saves time.
To maximize these benefits during endoscopic slide-in reconstruction, there are some key points that the operator should keep in mind. The surgical mesh must be broad enough to cover the entire defect, and long enough so that the posterior end can be placed on the posterior shelf. To ensure complete coverage, it is essential to measure the defect size via the preoperative CT scan. We recommend trimming the mesh to be approximately 2 mm larger than the defect in all directions. By pushing the mesh into the orbit through consecutive orders (posterior, superior, inferior, followed by anterior), as mentioned in the methods section, the larger mesh can always successfully slide into the orbit. This procedure is probably the most difficult part of the endoscopic slide-in method, and requires some time and practice. As muscle incarceration may occur during this procedure, a forced duction test is strongly recommended.
Our method has drawbacks. If bleeding occurs, then the visual field can be completely disturbed. The patient may experience nose bleeding for 1 or 2 days postoperatively. The slidingin procedure may give rise to blow-in fracture or muscle incarceration; thus, an intraoperative or postoperative CT scan is recommended. In addition, based on the operator’s experience in both approaches, the endoscopic method has a steeper learning curve. Lastly, the endoscopic approach has limited indications; it cannot be used for comminuted fractures or combined inferior wall fractures, as the orbit is not stable enough to endure the sliding-in procedure under these circumstances. However, in our opinion, if used in appropriate indications, the merits of the endoscopic method are great enough to overcome these drawbacks.
In conclusion, our endoscopic slide-in technique did not turn out to be complicated, and the results were not inferior compared to those of the external method. We suggest that our endoscopic method is beneficial to patients as it reduces the operation time, and can prevent several potential side effects found in the transcaruncular approach. We are planning to conduct a larger-scale study for further validation.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B1905/540-107) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patient provided written informed consent for the publication and the use of his images.
Supplementary material
Supplementary Table S1.
Summary of the endoscopic group.
Supplemental data can be found at: https://doi.org/10.7181/acfs.2020.00605.
Supplementary Table S2.
Summary of the transcaruncular group.
Supplemental data can be found at: https://doi.org/10.7181/acfs.2020.00605.
Supplementary Video S1.
Video demonstrating the entire surgical procedure of the endoscopic slide-in medial orbital wall reconstruction.
Supplemental data can be found at: https://doi.org/10.7181/acfs.2020.00605.v001.