|
 |
- Search
| Arch Craniofac Surg > Volume 22(3); 2021 > Article |
|
Abstract
Posttraumatic pseudoaneurysm of the face is caused by blunt, penetrating, or surgical trauma. Although its incidence is low, pseudoaneurysm rupture can cause a life-threatening, massive hemorrhage. A 48-year-old man visited our emergency center due to a fall-down accident. Three-dimensional computed tomography (CT) showed a comminuted zygomaticomaxillary complex fracture of the left face. After open reduction and internal fixation, the surgical wound healed without any complications. However, the patient was readmitted 10 days after surgery due to pus-like discharge from the wound. Contrast-enhanced CT to find the abscess unexpectedly revealed a pseudoaneurysm in the left retromaxillary area. Massive oral bleeding occurred on the night of re-hospitalization and emergency surgery was done. The bleeding site was identified as a pseudo-aneurysmal rupture of the posterior superior alveolar artery in the retromaxillary area. Hemostasis was achieved by packing Vaseline gauze in the maxillary sinus using an endoscope. Delayed rupture and massive bleeding of posttraumatic retromaxillary pseudoaneurysm after a zygomaticomaxillary fracture is a low-probability, but high-impact event. Therefore, additional contrast-enhanced CT should be considered to evaluate the possibility of a posttraumatic pseudoaneurysm in cases of severe comminuted zygomaticomaxillary fracture.
Posttraumatic pseudoaneurysm is caused by blunt, penetrating, or surgical trauma. The most frequent sources in the face are the superficial temporal artery, the internal maxillary artery, and the distal part of the facial artery [1]. Although its incidence is low, pseudoaneurysm rupture causes a life-threatening hemorrhage, and hemostasis can be extremely difficult even when using a surgical approach [2]. Therefore, early diagnosis and treatment are very important. In this report, we present a unique case of diagnosis and treatment of a retromaxillary pseudoaneurysm.
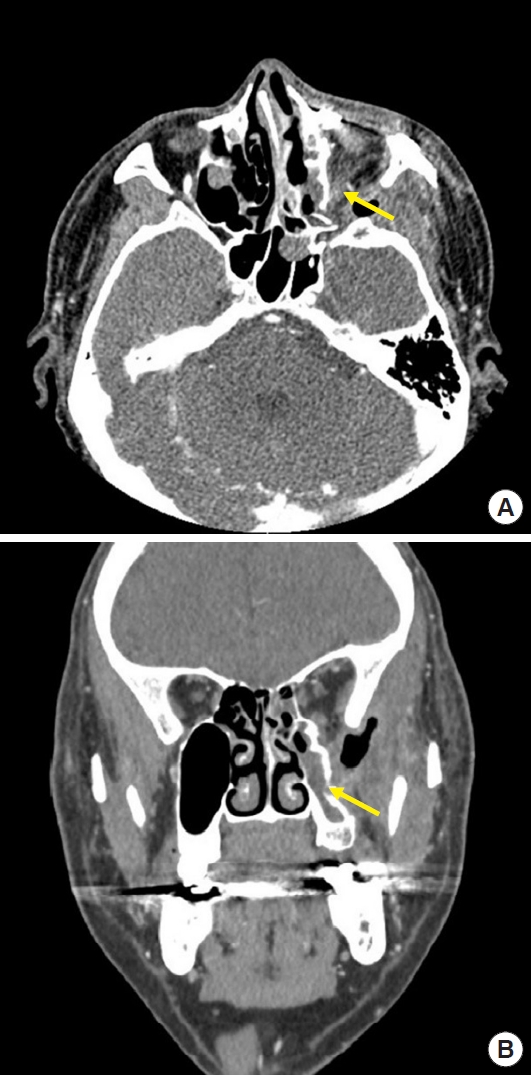
A 48-year-old man without underlying disease visited our emergency medical center after a fall-down accident. Physical examination revealed a deep lacerated wound with bone exposure on the left cheek. Three-dimensional facial computed tomography (CT) showed a comminuted zygomaticomaxillary complex fracture on the left side (Fig. 1). In an emergency operation, all foreign bodies and contaminated tissues inside the open wound were removed, and primary closure was then done. After facial swelling had subsided, open reduction and internal fixation (ORIF) was performed for the left zygomaticomaxillary fracture under general anesthesia. The patient was discharged without any complications.
However, the patient was readmitted only 10 days after surgery due to pus-like discharge from the previous wound. The patient also complained of left cheek pain. Contrast-enhanced facial CT to evaluate the abscess and inflammation of the left cheek unexpectedly revealed a pseudoaneurysm in the left retromaxillary area (Fig. 2). The patient was scheduled for angioembolization with surgical exploration as a backup plan for the treatment of the pseudoaneurysm on the following day. However, massive oral and nasal bleeding occurred on the night of re-hospitalization. At the bedside, the previous gingivobuccal incision site was reopened and temporary hemostasis was achieved by manual compression on the posterior maxillary wall with gauze packing through the gap of the maxillary anterior wall. An emergency operation under general anesthesia was performed within a few minutes. An endoscopic approach was used to determine the bleeding focus more precisely. The bleeding site was identified as a pseudo-aneurysmal rupture of the posterior superior alveolar artery in the left retromaxillary area (Fig. 3). Electrocauterization and ligation were not enough to achieve hemostasis at the bleeding site. Vaseline gauze packing was therefore performed at the bleeding site for compression in the maxillary sinus. The hemoglobin level of the patient decreased by about 2.0 g/dL in 4 hours, necessitating urgent blood transfusion. The postoperative contrast-enhanced facial CT showed a significant decrease in the pseudoaneurysm size (Fig. 4). No additional active bleeding occurred at the operation site during 6 months of postoperative follow-up (Fig. 5).
An aneurysm is an irreversible extension of an artery. A true aneurysm is defined as extension of the entire artery wall, which is composed of the tunica intima, media, and adventitia, whereas a false aneurysm (or pseudoaneurysm) occurs when only part of the artery wall and surrounding tissues are expanded.
Posttraumatic facial aneurysm is caused by incomplete tearing of the vascular wall and blood flow into the surrounding tissues through the side. If leakage continues through the torn blood vessel, it gradually increases in size and eventually becomes a pseudoaneurysm [3]. Additionally, a pseudoaneurysm can be torn by trauma-induced fractured bone fragments, resulting in massive bleeding [4].
A facial pseudoaneurysm most often forms within days to weeks after a blunt injury on the face [5], or within a similar interval after bone reduction surgery. The risk factors for facial pseudoaneurysm are infection, poor nutrition, and radiation therapy [6]. In this case, it was not clear whether the pseudoaneurysm had occurred at the time of injury or after reduction surgery.
Physical and radiological examination is the main diagnostic method for pseudoaneurysms. On physical examination, the features of traumatic facial pseudoaneurysm include pain, progressive pulsatile swelling, and neuralgia [4,7]. In patients with anterior maxillary wall fracture, pain may occur if proper reconstruction is not performed, so it is necessary to differentiate it [8]. In the case of neuralgia, it is necessary to differentially diagnose the numbness of the entire cheek, the ala of nose, and the upper lip, which are the dominant regions of the infraorbital nerve due to midfacial bone fractures such as orbital wall fracture and zygomaticomaxillary fracture, which are common among facial bone fractures [9,10].
Imaging studies are very helpful diagnostic tools for the evaluation of the location and the size of the pseudoaneurysm. In particular, contrast-enhanced CT can be used to determine the location of the pseudoaneurysm, its size, and its relationship with adjacent structures [2,7]. Contrast-enhanced CT shows a pseudoaneurysm as a hyperattenuating smooth-walled sac adjacent to an artery. In this case, the patient did not complain of any particular symptoms other than left cheek pain before the rupture. However, the presence of the pseudoaneurysm was confirmed on contrast-enhanced facial CT, and we judged that rupture of the pseudoaneurysm had caused massive oral and nasal bleeding. Furthermore, the patient had no history of additional facial trauma or other specific underlying diseases that could have caused the massive bleeding. Therefore, an immediate emergency operation was performed while continuously applying manual compression to the bleeding site.
The treatment options for pseudoaneurysm have been described in previous articles. These include direct compression of the aneurysm, angioembolization, and surgical resection of the affected part of the artery [2]. Angioembolization is a promising noninvasive treatment method that has recently attracted attention. It can access microvascular structures that are difficult to reach by surgery. Furthermore, it does not require general anesthesia and has the advantage of low blood loss [11]. However, complications such as thromboembolic events, craniofacial pain, swelling and paralysis, and nasopharyngeal ulcers may occur due to intraoperative rupture of the pseudoaneurysm wall [12]. Also, the development of a new venous malformation region near the site of embolization can occur [13]. So, persistent follow-up through imaging is required.
There are several lessons to be learned from the clinical management of the case described herein. First, when the patient visited the emergency medical center after a fall-down accident, non-enhanced 3-dimensional facial CT was performed only to evaluate the facial bone fracture. In this patient, the surgical procedures performed for wound irrigation and internal fixation after open reduction are unlikely to have caused damage to the maxillary posterior wall during surgery. Any application of shock or external pressure to the patient during hospitalization can be precluded. For the above reasons we presume that the vessel had been injured due to the fracture of the posterior maxillary wall at the time of trauma resulting in the formation of a pseudoaneurysm and delayed rupture. Retrospectively, it would have been better if the possibility of a pseudoaneurysm had been checked earlier by conducting a contrast-enhanced facial CT scan to assess the damage of the facial vessels, as the severe comminution of the open fractures of the maxilla and the zygoma have been indicative of trauma severity. Even if contrast-enhanced facial CT had been performed after ORIF, the retromaxillary pseudoaneurysm might have been detected before the life-threatening emergency.
Severe fractures of the posterior maxillary wall as detected on non-enhanced facial CT, increase the possibility of injury to the adjacent maxillary artery. In such cases, additional contrast-enhanced facial CT imaging could be indicated for the early detection and treatment of pseudoaneurysm.
Second, we did not implement a complete solution to the pseudoaneurysm. Adjuvant angioembolization immediately after identifying the pseudoaneurysm would have produced a better result.
Therefore, during the initial assessment of a severe facial bone fracture, contrast-enhanced facial CT might be helpful for evaluating both the facial bone fracture and abnormalities of the vascular system. If a pseudoaneurysm is found, close observation, follow-up contrast-enhanced facial CT, and adequate treatment are required.
Notes
Conflict of interest
JHH and KSK are editorial board members of the journal but were not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Ethical approval
The study was approved by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUHEXP-2021-114) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Fig.┬Ā1.
Preoperative 3-dimensional facial computed tomography image of the patient. A comminuted zygomaticomaxillary fracture can be observed on the left side.
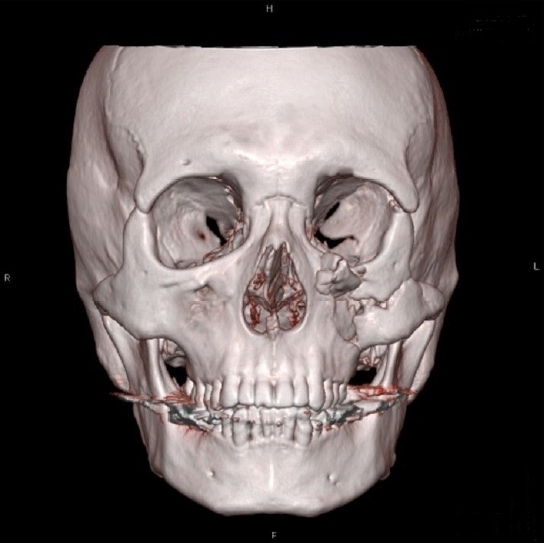
Fig.┬Ā2.
The preoperative computed tomography (CT) images show a 1├Ś0.8-cm pseudoaneurysm in the left retromaxillary area (yellow arrow). (A) Axial view. (B) Coronal view.

Fig.┬Ā3.
Endoscopic photograph of the patientŌĆÖs left retromaxillary area. It was easier to secure the surgical field of view via an endoscopic approach. Definitive hemostasis could also be accomplished.

REFERENCES
1. Conner WC 3rd, Rohrich RJ, Pollock RA. Traumatic aneurysms of the face and temple: a patient report and literature review, 1644 to 1998. Ann Plast Surg 1998;41:321-6.


2. Alonso N, de Oliveira Bastos E, Massenburg BB. Pseudoaneurysm of the internal maxillary artery: a case report of facial trauma and recurrent bleeding. Int J Surg Case Rep 2016;21:63-6.



3. Dudaryk R, Horn DB, Green JM 3rd. Facial artery pseudoaneurysm: challenges of airway management. Anesth Prog 2018;65:52-5.



4. Nastro Siniscalchi E, Catalfamo L, Pitrone A, Papa R, Fama F, Lo Giudice G, et al. Traumatic pseudoaneurysm of the internal maxillary artery: a rare life-threatening hemorrhage as a complication of maxillofacial fractures. Case Rep Med 2016;2016:9168429.



5. Feliciano DV, Cruse PA, Burch JM, Bitondo CG. Delayed diagnosis of arterial injuries. Am J Surg 1987;154:579-84.


6. Hertzer NR. Extracranial carotid aneurysms: a new look at an old problem. J Vasc Surg 2000;31:823-5.


7. Goddard AJ, Lenthall RK, Bradley PJ. Endovascular management of infected carotid artery pseudoaneurysm complicating pharyngolaryngectomy: complete occlusion followed by early recurrence and rebleeding. J Laryngol Otol 2004;118:991-5.


8. Park JK, Kim SW. Zygomaticomaxillary complex fracture after two-jaw surgery. Arch Craniofac Surg 2020;21:301-4.



9. Lee SY, Kim SH, Hwang JH, Kim KS. Sensory recovery after infraorbital nerve avulsion injury. Arch Craniofac Surg 2020;21:244-8.



10. Lee H, Kim KS, Choi JH, Hwang JH, Lee SY. Trauma severity and mandibular fracture patterns in a regional trauma center. Arch Craniofac Surg 2020;21:294-300.



11. Hassan F, Younes A, Rifai M. Endovascular embolization of post-tonsillectomy pseudoaneurysm: a single-center case series. Cardiovasc Intervent Radiol 2019;42:528-33.


- TOOLS
-
METRICS

-
- 5 Crossref
- Scopus
- 3,611 View
- 81 Download
- Related articles in ACFS
-
Treatment of post-traumatic hematoma and fibrosis using hyaluronidase injection2018 September;19(3)