|
 |
- Search
| Arch Craniofac Surg > Volume 22(5); 2021 > Article |
|
Abstract
A 65-year-old woman presented with a solid mass on the right temporal area. The mass had grown for over 2 years without any initiating event of trauma or inflammation. Before excision, the patient went through a computed tomography scan, revealing a calcified mass without bony connection. Under general anesthesia, an excisional biopsy was performed. Microscopic examination confirmed a diagnosis of soft tissue osteoma. Soft tissue osteoma is rare, especially in the head and neck region. Osteomas in the temporal region have not been reported yet. Due to its rarity, osteoma might be misdiagnosed as another soft tissue or bone origin tumor. Its treatment of choice is simple excision. In this review, we present an unusual clinical form of soft tissue osteoma.
When encountering a localized hard mass in soft tissues, plastic surgeons use a variety of diagnostic tools including physical examination, computed tomography, and magnetic resonance imaging. When a calcified or bone-forming tumor is suspicious after evaluation, the lesion needs to be removed to differentiate soft tissue osteoma from myositis ossificans, soft tissue osteochondroma, and osteosarcoma.
Osteoma is a benign, slow-growing mass that is usually associated with the maxillofacial skeleton. Osteoma can be divided into three groups: central, peripheral, and extra-skeletal. Central osteoma occurs in the endosteum. Peripheral osteoma forms within the periosteum. Extra-skeletal osteoma develops in the soft tissue [1,2]. Osteoma itself is an uncommon neoplasm. Soft-tissue osteoma is exceedingly rare. In the literature, the origin of soft-tissue osteoma is usually the oral cavity [3], skin, or extremities [4-6], with few occurring in the head and neck area [7]. In this study, we report a soft-tissue osteoma in the temporal region of the head, which has not been previously described in the literature.
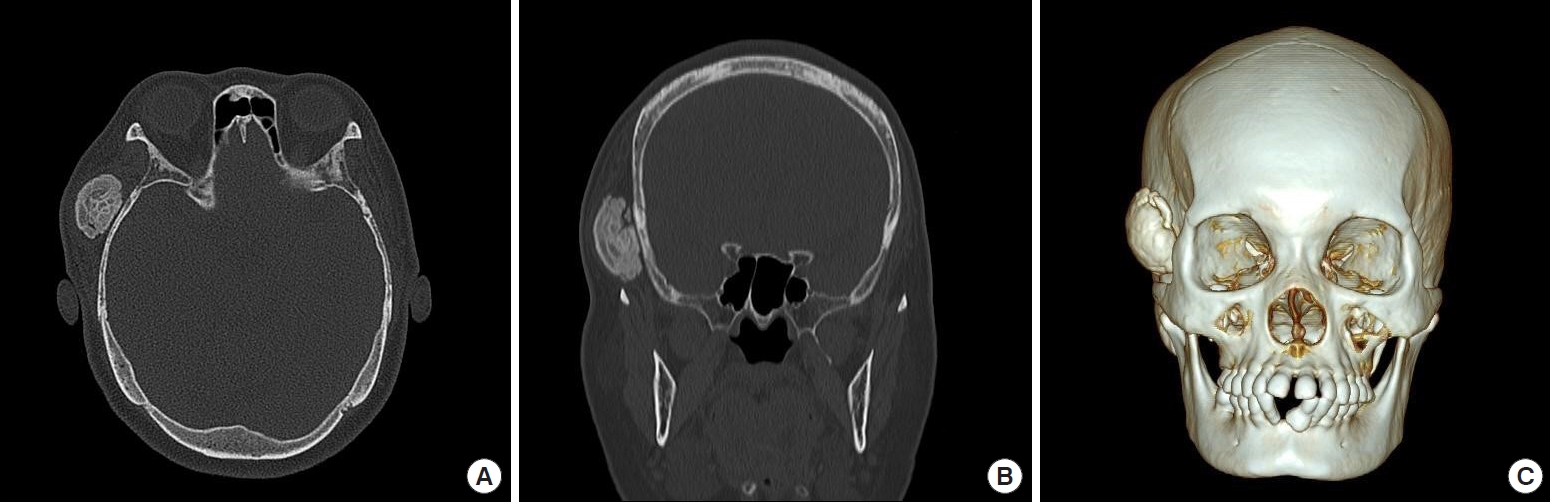
A 65-year-old woman presented a hard protruding mass on the right temporal area without pain or tenderness. The mass had grown for over 2 years without prior event of trauma or associated inflammation. On physical examination, the mass was found to be a solid mass. The patient demonstrated a normal facial expression. To evaluate its size, contour, and location, the patient underwent an enhanced computed tomography imaging scan. In the scan, the mass was revealed to be a calcified mass with a size of about 2.8×1.9×3.8 cm without any bony connections. Although it was accompanied by surrounding soft tissues, no cortical bone disruption was observed. The radiologist interpreted the mass as a calcified granuloma or pilomatrixoma (Fig. 1).
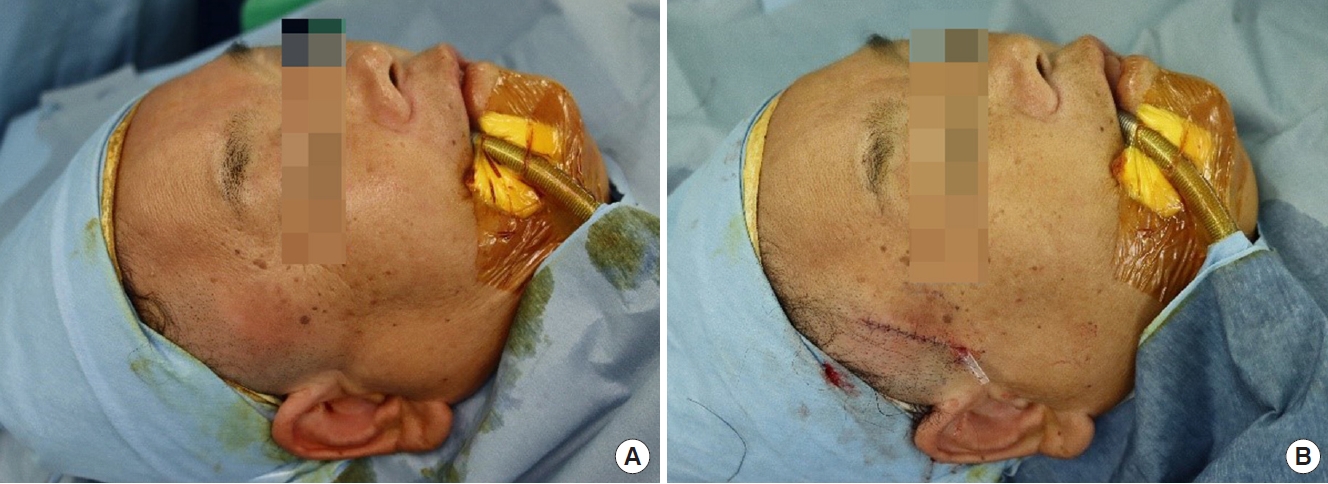
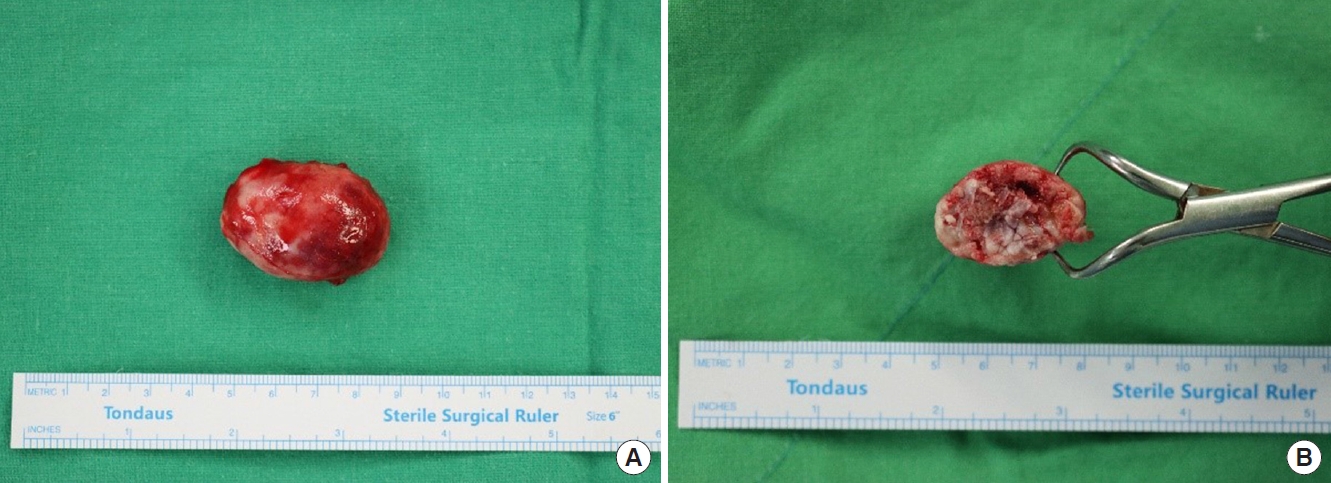
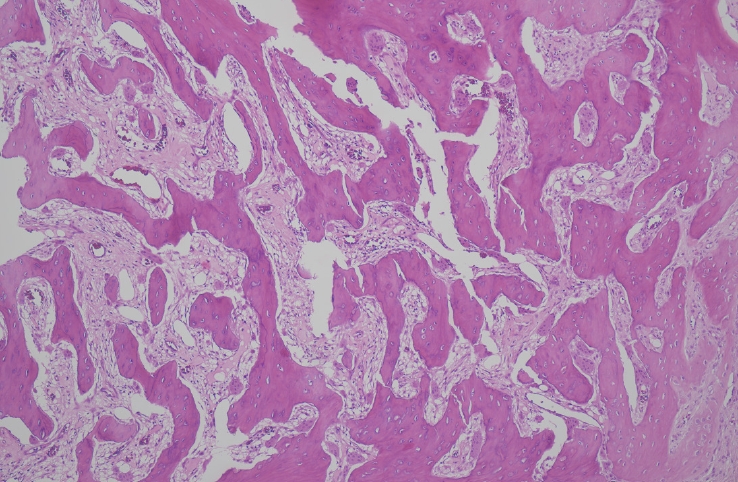
Under general anesthesia, a longitudinal incision of approximately 4 cm was conducted over the center of the mass located between the temporalis muscle and the skull (Fig. 2). The mass had an actual measurement of 4.8×3×2.7 cm. It was gray-white and well capsulated (Fig. 3). Microscopic examination confirmed the diagnosis as soft tissue osteoma (Fig. 4). After the operation, the patient reported a decrease in forehead wrinkling on the right side. In the follow-up period, the symptom was resolved.
Other bone-forming neoplasms demonstrating calcified lesions with soft tissue origin include myositis ossificans, soft tissue osteochondroma, and osteosarcoma. Compared with soft tissue osteoma, these other forms of neoplasms may require adjuvant chemotherapy, radiotherapy, or a wider range of excision [8]. Consequently, it is significant to make an accurate histologic confirmation through excisional biopsies.
Soft tissue osteomas are composed of mature lamellar bone that often include a small portion of trabecular bone and hyaline cartilage [9]. These tumors are slow-growing and isolated from the adjacent bone. Moreover, they are devoid of histologic characteristics such as atypia, hypercellularity, and zonal patterns which appear in osteosarcoma or myositis ossificans. In myositis ossificans, soft tissue osteochondroma and osteosarcoma may show zonal growth pattern, little ossification in the central zone, maturation at the periphery, or hypercellularity [10].
In plain radiography and computed tomography scan, extraskeletal osteomas show densely ossified lesion. Myositis ossificans may show variable radiographic appearances according to disease course. Its typical feature is circumferential calcification with a radiolucent center compared to uniform density shown in soft-tissue osteoma. Soft-tissue osteochondroma tends to have a more irregular shape in radiography than osteoma. It may have a cartilage cap or scattered mineralization. Radiographic signs of soft tissue osteosarcoma include amorphous calcification and ossification. It may have extensive central mineralization and lack of peripheral well-defined ossification [9]. These differential diagnoses are usually located at lower extremities.
Osteoma is a common benign bone tumor that usually arises from the long bones or the maxillofacial skeleton. Extra-skeletal osteomas have been found in different parts of the body, most often in the tongue [3], skin and extremities [4-6]. Apart from some reports of such tumors in the tongue or oral cavity, none of the previous literature has reported these tumors in the head and neck region.
Since soft tissue osteomas are not common, they can be misdiagnosed as pilomatrixoma [11] or tumors of bone origin. To avoid such misdiagnoses, preoperative computed tomography imaging and excisional biopsy are vital. By doing surgical excision for diagnostic purpose, treatment goals can also be fulfilled.
The exact etiology of benign bone-forming lesions of the soft tissue remains unclear. In previous work, it has been proposed that myositis ossificans, soft tissue osteochondroma, and soft tissue osteoma can form a spectrum of changes related to soft tissue injury. However, the homogeneous structure of osteoma and the lack of inflammation hint at another cause suggest another pathophysiology of the tumor [10]. To be classified as a neoplasm, such a lesion tends to arise spontaneously, not secondary to trauma or inflammation. Moreover, it needs to not be of developmental origin. It should grow unattached to the periosteum or periarticular structures [10]. The present case fulfills these criteria.
Notes
Ethical approval
The study was approved for exemption by the Institutional Review Board of Jeonbuk National University Hospital (IRB exemption No. CUH 2021-09-015).
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Author contribution
Conceptualization: Nae-Ho Lee. Data curation: Yun-Seob Kim. Formal analysis: Si-Gyun Roh, Yun-Seob Kim. Methodology: Nae-Ho Lee, Yun-Seob Kim. Project administration: Si-Gyun Roh. Writing - original draft: Yun-Seob Kim. Writing - review & editing: Nae-Ho Lee, Yun-Seob Kim. Investigation: Yun-Seob Kim. Supervision: Si-Gyun Roh, Jong-Lim Kim, Nae-Ho Lee, Jin-Yong Shin. Validation: Si-Gyun Roh, Jong-Lim Kim, JinYong Shin.
REFERENCES
1. Sim HS, Lee DG, Hwang JH, Kim KS, Lee SY. Peripheral osteoma on the medial eyebrow successfully extracted while preserving supratrochlear nerve. Arch Craniofac Surg 2019;20:421-4.



2. Yoo H, Doh G, Kim BK. Treatment of multiple craniofacial osteomas by endoscopic approach. Arch Craniofac Surg 2020;21:261-3.



3. Liu JY, Tan KK. Lingual osteoma: case report and literature review. Singapore Med J 2011;52:e198. -200.

5. Holmen J, Stevens MA, El-Khoury GY. Case report: paraarticular soft-tissue osteoma of the hip. Iowa Orthop J 1999;19:139-41.


6. Tsai CH, Wang DY, Horng-Chaung H. Soft-tissue osteoma of the hand: case report. J Hand Surg Am 2006;31:998-1000.


7. Li L, Wang Y, Zhao YF, Lu HZ, Zou SM, Luo DH. Soft-tissue osteoma in the neck paravertebral space. Quant Imaging Med Surg 2012;2:139-41.


9. Kransdorf MJ, Meis JM. From the archives of the AFIP: extraskeletal osseous and cartilaginous tumors of the extremities. Radiographics 1993;13:853-84.


- TOOLS
-
METRICS

-
- 3 Crossref
- Scopus
- 3,484 View
- 102 Download
- Related articles in ACFS