Reconstruction of a total defect of the lower eyelid with a temporoparietal fascial flap: a case report
Article information
Abstract
The reconstruction of total lower eyelid defects is challenging to plastic surgeons due to the complicated anatomical structure of the eyelid. In addition, in the setting of cancer excision, the resection is deep, which requires some volume augmentation. However, in some cases, free tissue transfer is not applicable. We report a case of using a temporoparietal fascia flap (TPFF) for reconstructing a total lower eyelid defect. A large erythematous mass in an 83-year-old woman was diagnosed as squamous cell carcinoma by biopsy. After wide excision, the defect size was about 8× 6 cm. The lower eyelid structures including the tarsus were removed. The TPFF including the superficial temporal artery was elevated and inset to the defect area. After the flap inset, a split-thickness skin graft with an acellular dermal matrix was performed on the fascial flap. There were no wound problems such as infection, dehiscence, or necrosis. After the patient’s discharge, partial skin graft loss and ectropion occurred. The complications resolved spontaneously during the postoperative period. We report a case of reconstructing a lower eyelid defect using a TPFF. A TPFF can be applied to patients with large defects for whom free tissue transfer surgery is not appropriate as in this case.
INTRODUCTION
To plastic surgeons, eyelid defects are very challenging to solve. The eyelid is a very delicate structure and plays an important role in both aesthetic and functional aspects [1,2]. Thus, surgeons should consider these two aspects simultaneously when repairing an eyelid defect.
The temporoparietal fascia flap (TPFF) is one of the thinnest flaps in the human body [3]. It is pliable enough to cover an irregular contour without distortion and has rich vascularity, acting as a dependable scaffold for skin grafts. It also has a wide arc of rotation that allows for extension to the midface, mandible, and oral cavity [4,5]. These advantages make the TPFF a very versatile reconstructive option in the head and neck areas.
In this report, we describe a case of a TPFF applied to a huge defect area including the lower eyelid and midface. If applicable, free tissue transfer may be superior to TPFF in that the former does not require an additional skin graft whereas the TPFF does. However, our patient was of an older age with low compliance to postoperative care. Thus, we planned the TPFF with a skin graft instead of free tissue transfer. Thus, a TPFF might be a suitable substitute for free tissue transfer in these patients.
CASE REPORT
A large erythematous mass in the left cheek of an 83-year-old woman was diagnosed as squamous cell carcinoma by biopsy (Fig. 1). Before surgery, facial and neck computed tomography was done. In the imaging modality, a large mass of about 5.4× 2.4× 4.3 cm in size was seen in the left cheek soft tissue layer without bone invasion. There was no evidence of cervical lymphadenopathy. Thus, wide excision with immediate reconstruction was planned.
Intraoperatively, the head and neck surgery team performed a wide excision, superficial parotidectomy, and selective neck dissection first. After the tumor was removed, the defect measured about 8 x6 cm with minimal malar bone exposure. Lower eyelid structures including the conjunctiva, tarsus, and pretarsal orbicularis oculi muscle were then removed (Fig. 2).
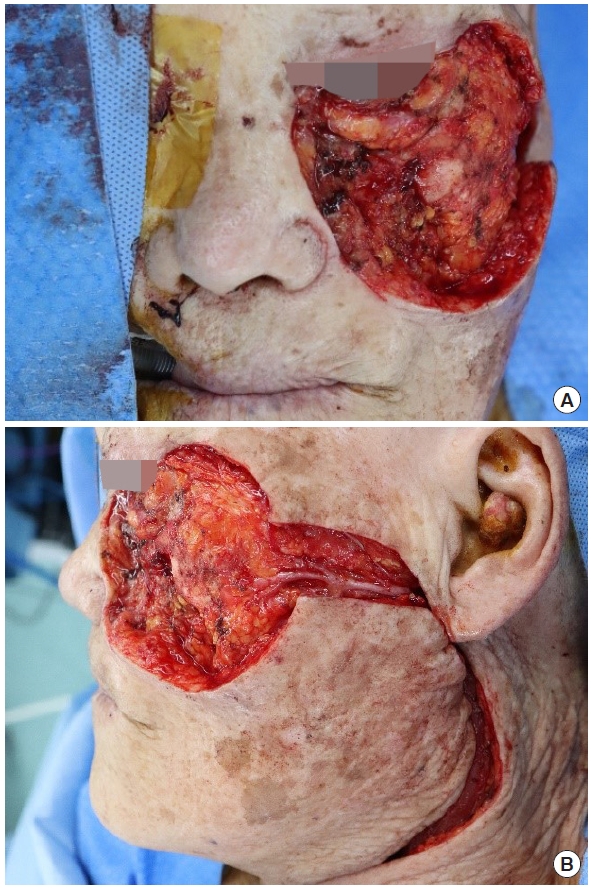
Photographs after wide excision of the mass and superficial parotidectomy. The left lower eyelid structures were removed and the defect measured about 8×6 cm. (A) Anterior view and (B) lateral view.
The TPFF was designed on the left scalp and the superficial temporal artery was traced using Doppler ultrasonography. A Y-shaped skin incision was made to the suprafascial level. After exposure of the temporalis muscle, an 8× 6 cm sized TPFF was elevated after ligating the distal part of the superficial temporal artery (Fig. 3). The TPFF was then inset to the defect area and anchored to the adjacent skin and conjunctiva. On the TPFF, a split-thickness skin graft harvested from the left thigh and acellular dermal matrix (Matriderm; MedSkin Solutions Dr. Suwelack, Billerbeck, Germany) was applied (Fig. 4). A bolster dressing was done to prevent hematoma formation and increase the uptake rate of the skin graft. During the postoperative period, a partial loss of the skin graft occurred. However, the loss recovered after dressing changes. Although mild ectropion without sclera show remained, the corneal protective function was restored.
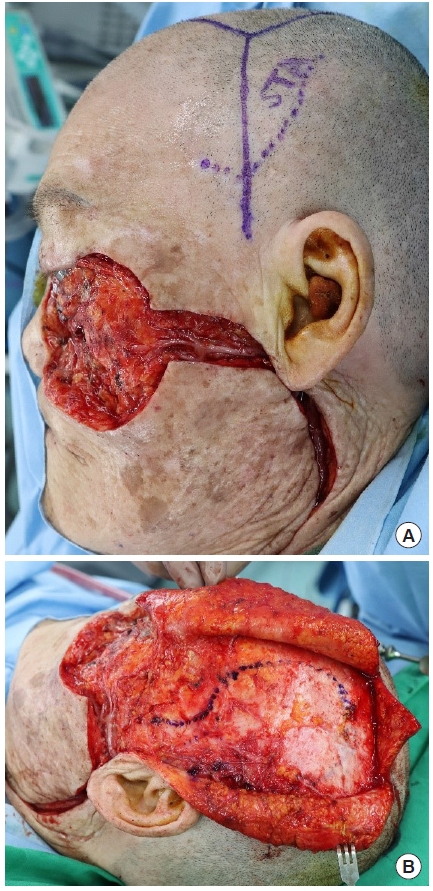
Temporoparietal fascia flap. (A) The superficial temporal artery was marked using Doppler ultrasonography. (B) After fascia layer exposure, the flap was designed to include the superficial temporal artery.
DISCUSSION
Lower eyelid defects usually pose a challenge to plastic surgeons. If poorly treated, patients may experience recurrent keratitis, corneal ulceration, and blindness in severe cases [6]. Aesthetic outcomes are also important to avoid negative social and psychological effects. Various surgical methods have been introduced for reconstruction depending upon the size of the defect [7]. The options include primary repair, skin grafts, local flaps, and free flaps.
For substantial defects that extend to a bone depth or in devitalized tissue beds, a skin graft is not adequate because of its low uptake rate and insufficient volume. Extensive defects prevent local advancement or a rotation flap from covering the defect. Forced closure with great tension may cause unfavorable wound healing or distort the adjacent structures [1,7].
In our case, the defect was huge, ranging from the lower eyelid to the cheek. Thus, options such as primary repair or a local flap were excluded. The depth of the defect was to the level of the malar bone. Thus, skin grafting alone was also not chosen. The patient had severe dementia. She was not expected to remain still after surgery. Thus, free tissue transfer was not applicable.
The TPFF is an easily accessible flap with a dependable blood supply. As mentioned, its pliable contour, wide rotation arc, and scaffold reliability make it a good alternative to a free flap [3-5]. Also, low donor site morbidity is one of its advantages [8]. Thus, the TPFF is widely used in head and neck reconstruction including hair-bearing tissue transfer, auricular defect, laryngectomy, skull base reconstruction, and periorbital reconstruction.
We used the TPFF to reconstruct a lower eyelid defect and obtained a satisfactory result. Through this case report, the readers can consider the TPFF as a good substitute for free tissue transfer under these circumstances.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved for exemption by the Institutional Review Board of Jeonbuk National University Hospital (IRB exemption No. CUH 2021-09-071).
Patient consent
The patient provided written informed consent for the publication and the use of her images.
Author contribution
Conceptualization: Nae-Ho Lee. Data curation: Yun-Seob Kim. Formal analysis: Yun-Seob Kim, Nae-Ho Lee. Methodology: Nae-Ho Lee, Si-Gyun Roh. Project administration: Nae-Ho Lee. Visualization: Yun-Seob Kim. Writing - original draft: Yun-Seob Kim. Writing - review & editing: Nae-Ho Lee. Investigation: Yun-Seob Kim. Resources: Yun-Seob Kim, Jin-Yong Shin. Supervision: Nae-Ho Lee, Si-Gyun Roh, Jin-Yong Shin. Validation: Si-Gyun Roh, Jin-Yong Shin.
Abbreviations
TPFF
temporoparietal fascia flap


