A computed tomography-based analysis of the structure of the mandible according to age and sex
Article information
Abstract
Background
The primary objectives of mandibular surgery are to achieve optimal occlusion, low sensory disturbance, and adequate fixation with early movement. In-depth knowledge of the mandibular structure is required to achieve these goals. This study used computed tomography (CT) to evaluate the mandibular cortical thickness and cancellous space according to age and sex.
Methods
We enrolled 230 consecutive patients, aged 20 to 50 years, who underwent CT scanning. The cortex and cancellous space centered around the inferior alveolar nerve (IAN) canal were measured at two specific locations: the lingula and second molar region. Statistical analysis of differences according to increasing age and sex was performed.
Results
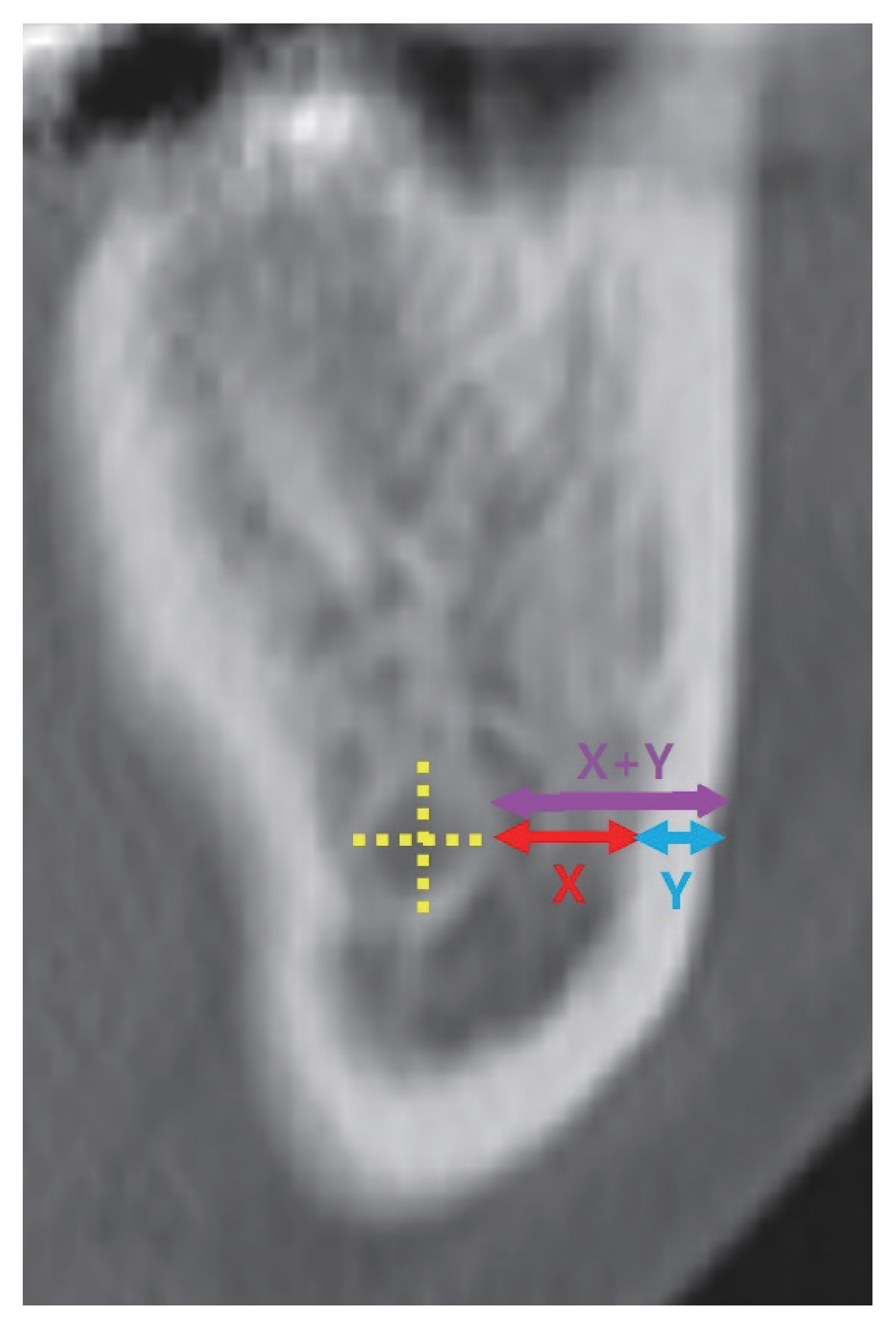
The t-test revealed that the cancellous space and cortical thickness differed significantly with respect to the threshold of 35 years of age. Both cortical thickness and cancellous space in the molar region were negatively correlated with age. Meanwhile, both cortical thickness and cancellous space in the lingula region showed a positive correlation with age. With respect to sex, significant differences in the cancellous space at the molar region and the cortical thickness at the lingula were observed. However, no further statistically significant differences were observed in other variables with respect to sex. The sum of each measurement on the mandibular body reflected the safe distance from the surface of the outer cortex to the IAN canal. The safe distances also showed statistically significant differences between those above and below 35 years of age.
Conclusion
Knowledge of the anatomical structure of the mandible and of changes in bone structure is crucial to ensure optimal surgical outcomes and avoid damage to the IAN. CT examination is useful to identify changes in the bone structure, and these should be taken into account in the planning of surgery for older patients.
INTRODUCTION
A comprehensive understanding of the structural features of the inferior alveolar nerve (IAN) canal, cortical bone, and cancellous space is essential for successful mandibular surgery requiring fixation or osteotomy. Depending on patient age and sex, there are anatomical variations in the proximity of the IAN canal to the outer cortex and in bone thickness. These may account for the vulnerability of the nerve to injury or bony instability when performing osteotomy or plate fixation [1–4]. These complications frequently occur if the IAN canal runs close to the buccal cortex or if the cortex itself is too thin.
Achieving adequate fixation, optimizing occlusion, and minimizing sensory disturbances are the primary objectives in mandibular surgery, including fracture-related surgery and orthognathic surgery [3–9]. Following mandibular bone fracture reduction or repositioning of bone segments in jaw surgery, adequate internal fixation of the plate is necessary for the stability of the bone [10]. Adequate fixation allows early mobilization of the jaw after surgery and enables patients to regain function sooner and return to their daily lives earlier [3]. Therefore, an effective fixation method can reduce hospital stay and result in good surgical outcomes [3]. Furthermore, as the IAN passes through the IAN canal, which is located inside the mandibular structure, adverse events, such as stretching or transection of the IAN, may occur during mandibular surgery [1,2]. Specifically, the IAN may be damaged directly during osteotomy and splitting procedures in orthognathic surgery, and care should be taken to minimize such complications [4].
A review of structural characteristics using computed tomography (CT) is valuable in this regard. Although the bony changes associated with age and sex have been studied, few studies have examined such changes in the mandible [11–14]. This study used CT to evaluate, statistically test, and describe mandibular changes with respect to age and sex to promote the safety of related surgical procedures.
METHODS
Patients
This was a retrospective study involving 230 consecutive patients who underwent CT scanning in the department of plastic surgery at our hospital between 2017 and 2021. All patients who underwent CT scanning for any reason in the plastic and reconstructive surgery department were enrolled. To avoid bias associated with an edentulous mandible or mandibular growth, we only included patients aged 20–50 years [15]. We excluded patients with a diagnosis of mandibular deformity or history of mandibular surgery or fractures and those with mandibular tumors that could affect the structure of the mandible. Patient demographic characteristics are shown in Table 1.
Measurements
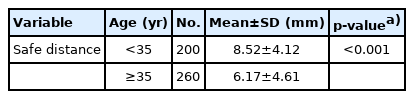
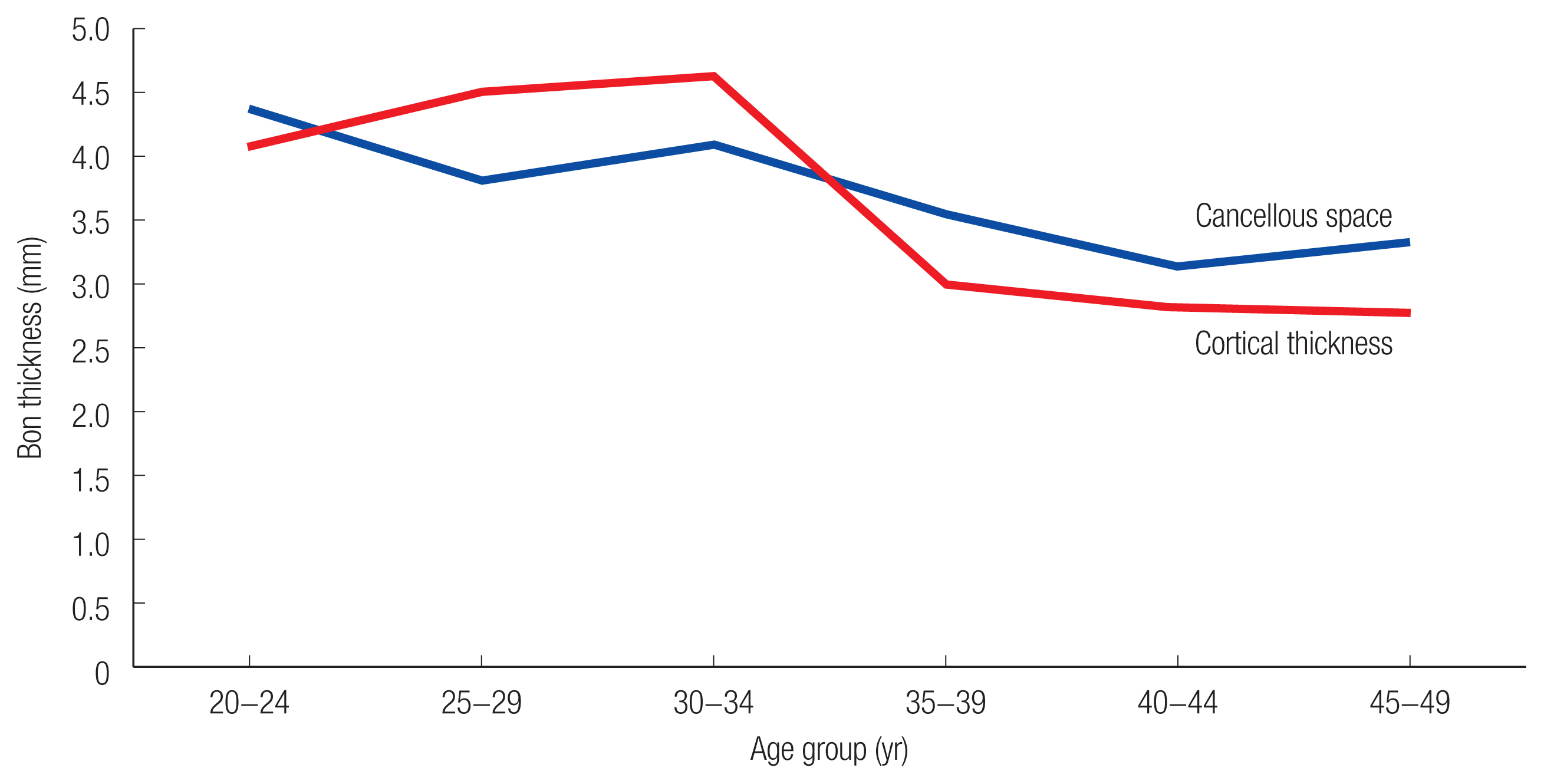
All patients underwent CT scanning (Siemens, Erlangen, Germany) with a high attenuation value (Hounsfield 1,000 or less), and the obtained images were sent to the image viewer, PiView STAR (Infinitt Co. Ltd., Seoul, Korea). The horizontal cancellous space and cortical thickness were measured centered on the IAN canal using PiView STAR (Infinitt Co. Ltd.). The measurements were made in two locations: at the lingula and at the second molar region (Figs. 1, 2). We determined the measurement location in advance to ensure consistency, and we defined the lingula region as the first section of the CT scan showing the entire IAN canal after the mandibular foramen. When measuring the second molar region, the authors took measurements from the first section of CT showing the second molar after the first molar [16]. As shown in Figs. 1 and 2, the yellow dotted line represents the center of the IAN canal. The width of the cancellous bone space and the cortical thickness were measured by drawing a horizontal line extending from the center of the IAN canal to the cortical surface, indicated as X and Y, respectively (Figs. 1, 2). During the measurements, when X (cancellous space) was too narrow to be identified in the limited CT resolution, the value was recorded as zero. All measurements of the body of the mandible were performed in the coronal view, while the transverse view was used for measurements of the lingula region. Data from both sides of the mandible were collected from 230 patients, with a total of 460 sides included and studied. The cohort was split into two groups with respect to age (age of 35 years was used as the threshold) and sex. Bony changes according to age in the mandible and lingula regions are illustrated in two linear graphs. The sum of the cortical thickness and cancellous space was calculated to find a safe distance from the cortical surface to the canal. Subsequently, the safe distances were tested statistically for patients above and below the age threshold of 35 years.

Method of measurement in the molar region (coronal section of computed tomography). The yellow dotted cruciate indicates the inferior alveolar nerve (IAN) canal and its center. The imaginary line perpendicular to the outer cortex from the center of the IAN canal was drawn. The red double arrow represents the width of the cancellous space, and the blue double arrow represents cortical bone thickness.
Method of measurement in the lingula region (transverse section of computed tomography). The first section forming the canal was defined as a measurement point. The yellow dotted cruciate indicates the inferior alveolar nerve (IAN) canal and its center. The imaginary line perpendicular to the outer cortex from the center of the IAN canal was drawn. The red double arrow represents the width of the cancellous space, and the blue double arrow represents cortical bone thickness.
Statistical analysis
The statistical analyses were performed using SPSS version 26 (IBM Corp., Armonk, NY, USA). The independent t-test was used to detect differences in measurements with respect to age and sex. A p-value less than 0.05 was considered statistically significant.
RESULTS
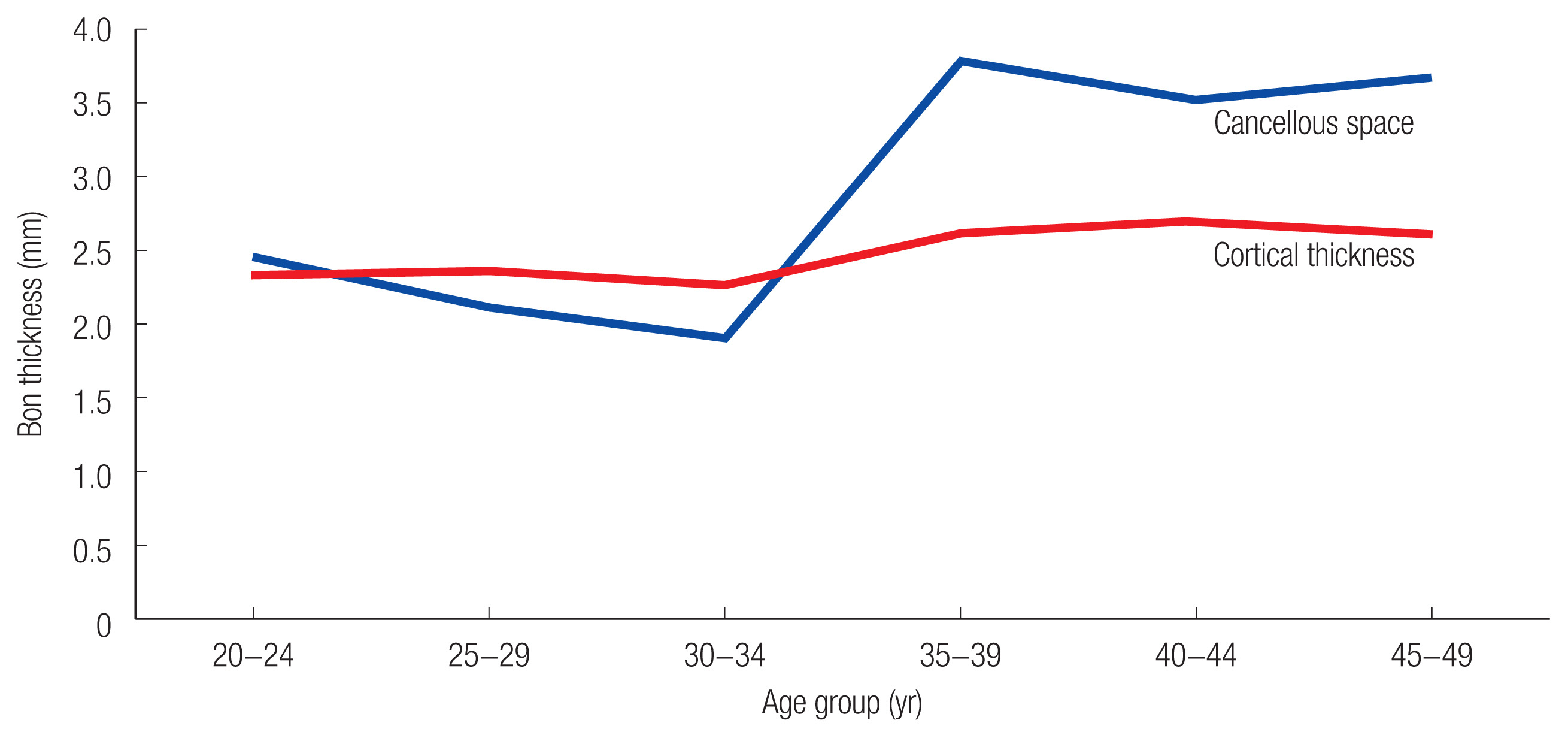
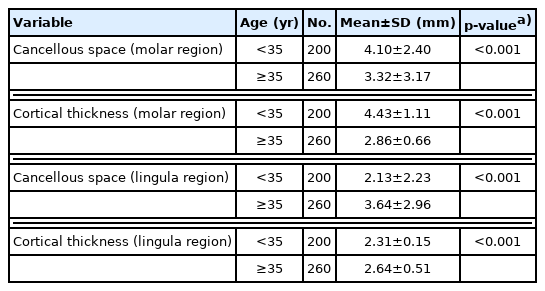
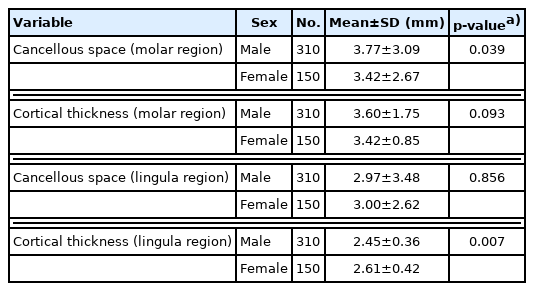
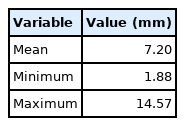
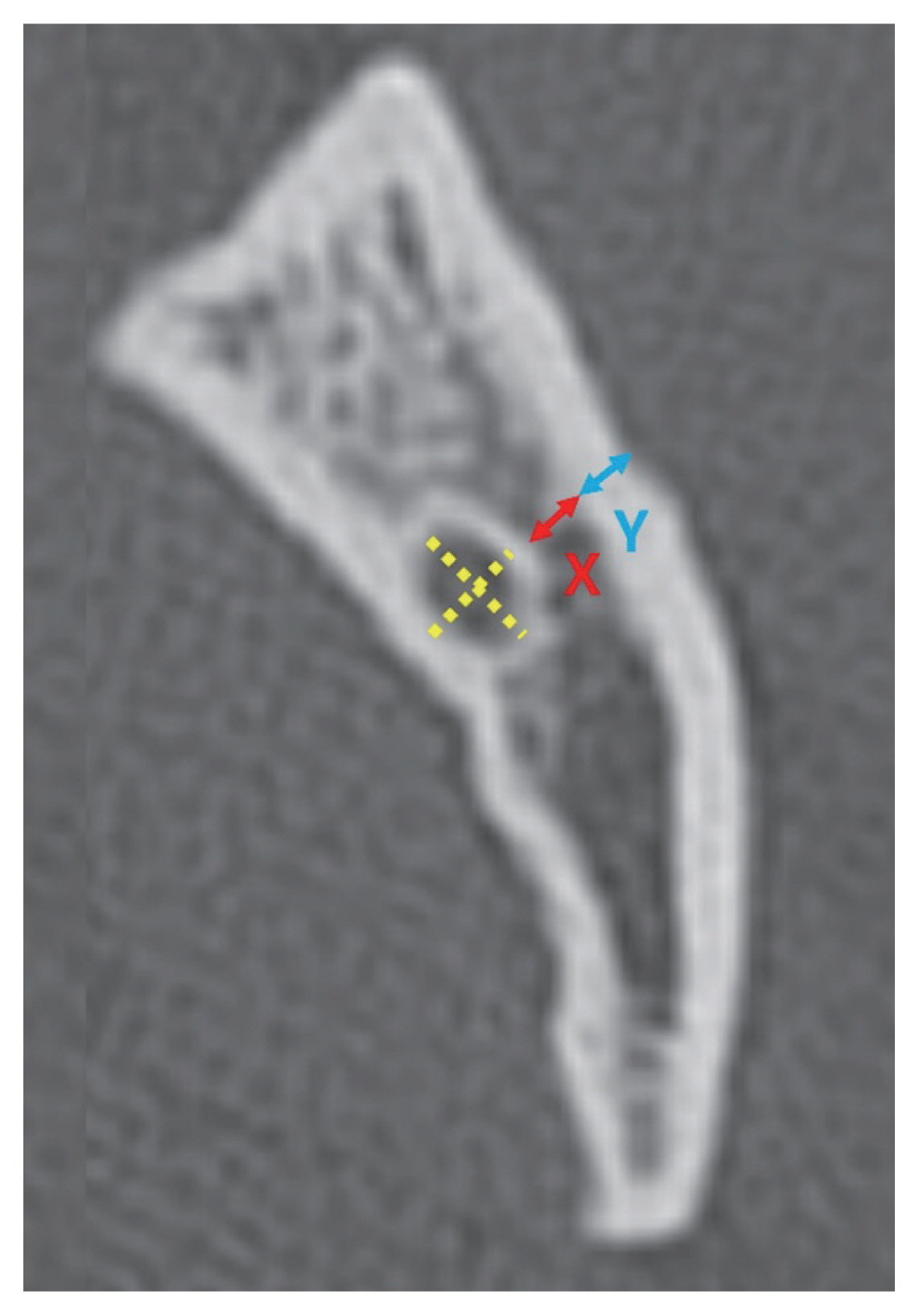
The mean age of the 230 subjects enrolled was 35.7 years (range, 20–50 years). One hundred and fifty-five subjects (67.4%) were male, while 75 subjects (32.6%) were female. There were 100 (43.5%) subjects under the age of 35 years and 130 (56.5%) subjects aged 35 years or older (Table 1). As shown in Figs. 3 and 4, the graphs revealed the changes in cortical thickness and cancellous space with age. The graph measured on the molar region showed a negative gradient with increasing age, indicating a decrease in cancellous space width and cortical thickness (Fig. 3). Conversely, the graph of the lingula region showed a positive slope indicating an increase in the width of cortical thickness and cancellous space (Fig. 4). There were significant differences in cortical thickness and cancellous space in both the lingula and molar regions between patients above and below 35 years of age (Table 2). However, significant differences between the sexes were only found in the cancellous space at the molar region and in the cortical thickness at the lingula (Table 3). In the younger age group, the cortical thickness and cancellous space were significantly greater in the molar region and smaller in the lingula region (Table 2, Figs. 3, 4). A comparison of mean values revealed that the width of the cancellous space in the molar region was greater in the male group (male, 3.77 mm±3.09 mm; female, 3.42 mm±2.67 mm), while the cortical thickness in the lingula region was greater in the female group (male, 2.45±0.36 mm; female, 2.61±0.42 mm; p<0.05). Differences in cortical thickness in the molar region and cancellous space in the lingula region with respect to sex were not statistically significant (p>0.05) (Table 3). The distance from the IAN canal to the outer cortex was calculated using the sum of the cortical thickness and the width of cancellous space, reflecting the safe distance (Fig. 5). The mean was 7.20 mm (range, 1.88–14.57 mm) (Table 4). The test for safe distance (Table 5) revealed a significant difference between participants above and below the age of 35 years, similar to the data presented in Table 2.
Bone thickness according to age groups in the molar region. The cohort was divided into 5-year-interval groups. The cancellous space and cortical thickness decrease with age.
The distance from the inferior alveolar nerve canal to the outer cortex in the molar region was also calculated (X+Y). This was the sum of the width of the cancellous space (X) and the cortical thickness (Y). The referred lines were the same as the one illustrated in Fig. 3. The purple double arrow represents the sum of two measurements.
DISCUSSION
Changes in the bone with respect to age and sex have been previously documented. Most reports examining age and sex-related differences involved long bones, such as the femur or radius, and revealed that cortical thickness decreased with advancing age [17,18]. Specifically, a significant reduction in cortical thickness was identified in female patients [17,18]. Lillie et al. [19] reported a negative correlation between the cortical thickness of the flat bones of the skull and increased age in women. Ohiomoba et al. [20] compared the alveolar cortical bone thickness in the three groups with age (12–16, 17–20, >20 years) and sexes. They observed cortical thickness significantly increased with age and found no relationship between the sexes [20]. However, few studies have investigated bone thickness changes in the mandible [11–14].
Preoperative CT scanning of patients is part of the routine workup to evaluate bony structure to plan mandibular surgery. Imaging also helps surgeons optimize the surgical procedure by avoiding nerve injury and providing adequate fixation. CT-based analyses of mandibular bone thickness have been previously reported. The trabecular bone ratio of the mandible has been calculated using micro-CT, and changes with respect to age, sex, and dentition have been analyzed [13]. A study evaluated the anatomical position of the IAN canal, localizing it and allowing accurate and safe osteotomy [12]. Studies of the cortex and cancellous space have also been conducted to elucidate the mandibular structure. Nicol et al. [21] assessed the cancellous space using cone-beam CT, and Lee et al. [22] measured cortical bone thickness and the distance from the nerve canal to the buccal cortex.
The cortex, cancellous bone, and the relationship between the two are associated with the stability of the bone structure [13,20,23]. In mandibular surgery, the hardware is commonly placed over the buccal cortex around the first to the third molar region, and osteotomy for mandibular repositioning is performed around the lingula and the buccal cortex of the mandibular body. These two regions may be clinically important to surgeons. Therefore, we selected these two locations for this study. Cortical thickness of the molar region was found to decrease with age, while that of the lingula region was found to increase. Similarly, the cancellous space in the molar region became narrower with advancing age, while that in the lingula region became wider (Table 2, Figs. 3, 4). Studies have hypothesized that cortical and cancellous bone changes show a negative gradient with aging [17–19]. However, bone thickness measurements showed a positive slope with age in the lingula region in this study. These results are comparable to those previously reported by Ohiomoba et al. [20].
A lower incidence of nerve damage and higher reliability of fixation are achieved with diverse mandibular procedures on many occasions [3,4,6]. However, an in-depth understanding of the anatomical features is necessary to achieve these goals. IAN injuries during mandibular surgery are reported in up to 50% of cases [6]. Moreover, most mandibular fractures involve the angle and body, which are associated with vulnerability of the IAN canal [6]. Therefore, these regions are critical when manipulating the mandible during reduction or fixation procedures. In particular, the risk of IAN injury is highest during drilling and screw placement. Osteotomy between the cortex and cancellous space is also hazardous to the IAN during mandibular sagittal splitting. Therefore, cortical thickness and the space between the cortex and the canal should be carefully evaluated prior to surgery because sufficient cortical thickness contributes to bony stability and prevention of IAN damage following fixation [4,24–26]. As mentioned earlier, the vital role of cortical thickness in bone surgery has been previously demonstrated, and it can thus be considered that cortical thickness affects the surgical procedure and postoperative stability [11,14,15,19,20,27,28]. Studies have indicated the importance of assessing cortical thickness to determine the optimum anatomical location for fixation [15,27–32]. Placement of the plate and screw over the mandibular body should be performed with caution in order to avoid injury to the IAN canal that runs through the structure. Although the plate is placed inferiorly or superiorly to the canal, a safe distance must be ensured while drilling and screwing [8,33]. Our results showed that the range of cortical thickness was 1.88 to 14.57 mm, indicating the possibility of injury to the canal in some cases (Table 4). Therefore, precise localization of the IAN should precede placement of the screw, and a minimal drilling technique with adequate depth should be adopted to avoid IAN injury.
Sagittal ramus osteotomy is a major procedure in corrective jaw surgery. Sagittal splitting is indispensable for the 3-dimensional movement of the mandible to cope with diverse jaw problems [34]. Nonetheless, this procedure should be considered carefully given the risk to the IAN or the risk of unstable fixation due to suboptimal osteotomy [4,35,36]. Osteotomy starts just behind the lingula and extends to the body of the mandible, dividing the cancellous space into two parts, i.e., the buccal and lingual cortices. The mechanical force during the procedure can be transmitted to the canal or the IAN directly if the cancellous space is narrow. Our study found that canals with a very narrow space approaching 0 mm at the ligula region were observed (Fig. 6). In such circumstances, invasion or damage to the IAN is regarded as inevitable [37]. It is recommended that the risk of these complications should be established based on the CT scan, and patients should be informed of these risks before undergoing surgery.
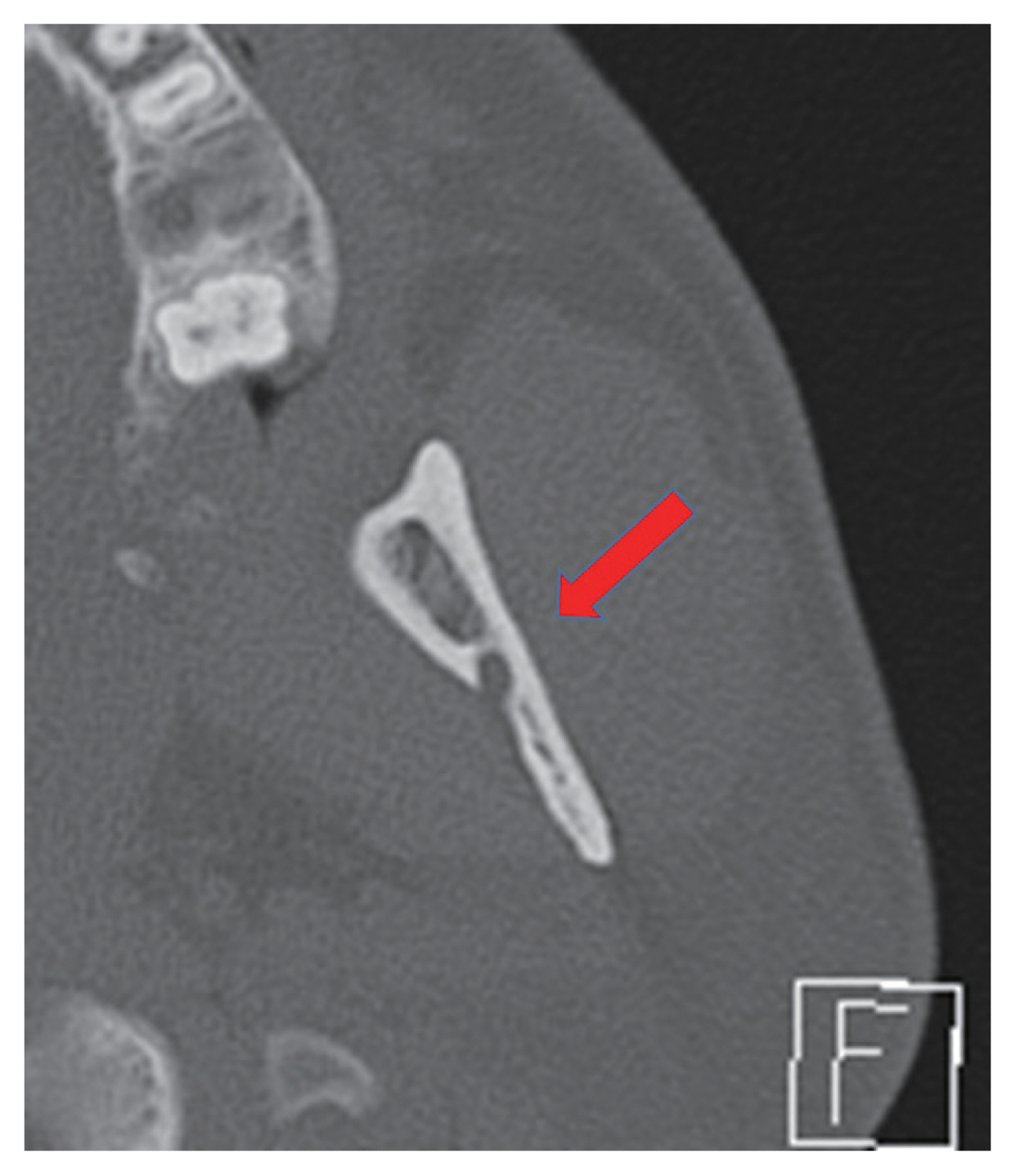
A patient with a narrow cancellous space (near zero) on the lingula aspect. In this case, the outer rim of the inferior alveolar nerve canal meets the inner border of the cortex (red arrow).
While conducting research, we observed that an insufficient safe distance was relatively common with increasing age (Table 5). An insufficient safe distance hampers the adequacy of mandibular procedures and leads to unfavorable outcomes and complications. Nevertheless, some patients over 35 years of age with a mean distance <7 mm may be vulnerable to nerve damage (Table 5). Therefore, information on the higher risks of complications should be provided to these patients as part of the informed consent process [38].
This study has a few limitations. Previous studies related to bony changes with age have used diverse methodologies to show the difference or the trend of the change [17–20]. However, here, we studied whether there was a statistically significant difference between the groups based on a threshold age of 35 years because this was the median age in the cohort, and when dividing the groups based on this age threshold, there was limited between-group deviation. Accordingly, we considered that the reliability of the statistical results could be increased by using the same parametric statistical method. However, using an age threshold of 35 years is supported by limited evidence, which comprises a limitation of this study. In addition, since this was a retrospective study, confounding factors that potentially affect mandibular structure such as dental conditions, oral health, medical conditions, and even the effects of contraceptives in women were not considered in the study. Especially, the absence of data regarding the calcium level, menopause, or osteoporosis constitutes a study limitation. Furthermore, the thickness of each CT section was 2 mm, which may have introduced errors in the precise localization of the landmarks.
Many published studies have already revealed that thinning of the cortex is an age-dependent process in most bony structures of the human body [11,14,15,19,20,27,28]. Overall, these findings indicate that a careful approach is required, particularly in treating older patients with a potentially higher risk of complications. Interestingly, the significant difference between the sexes was only revealed in the cancellous space of the molar region and the cortical thickness of the lingula region (Table 3). In conclusion, age-related bony changes are predictable, and CT scanning to identify the relevant findings is crucial. An understanding of the structural changes is necessary to ensure effectiveness of related surgical procedure.
Abbreviations
CT
computed tomography
IAN
inferior alveolar nerve
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
This study was approved by the Institutional Review Board of Kangdong Sacred Heart Hospital (IRB No. 2021-09-001). Informed consent was waived because of the retrospective nature of the study.
Author contribution
Conceptualization: Soyeon Jung. Data curation: Soyeon Jung, Yongjoon Chang. Formal analysis: Soyeon Jung, Chul Hoon Chung, Yongjoon Chang. Methodology: Soyeon Jung. Project administration: Soyeon Jung. Writing - original draft: Soyeon Jung, Hyunjong Yun, Kuylhee Kim, Yongjoon Chang. Writing - review & editing: Soyeon Jung, Chul Hoon Chung, Kuylhee Kim, Yongjoon Chang. Investigation: Soyeon Jung, Hyunjong Yun, Chul Hoon Chung. Supervision: Chul Hoon Chung, Kuylhee Kim, Yongjoon Chang.