One-point versus two-point fixation in the management of zygoma complex fractures
Article information
Abstract
Background
The treatment of zygoma complex fractures is of crucial importance in the field of plastic surgery. However, surgical methods to correct zygoma complex fractures, including the number of fixation sites, differ among operators. Although several studies have compared two-point and three-point fixation, no comparative research has yet been conducted on one-point versus two-point fixation using computed tomography scans of surgical results. Therefore, the present study aimed to address this gap in the literature by comparing surgical results between one-point and two-point fixation procedures.
Methods
In this study, we randomly selected patients to undergo surgery using one of two surgical methods. We analyzed patients with unilateral zygoma complex fractures unaccompanied by other fractures according to whether they underwent one-point fixation of the zygomaticomaxillary buttress or two-point fixation of the zygomaticomaxillary buttress and the zygomaticofrontal suture. We then made measurements at three points—the zygomaticofrontal suture, inferior orbital wall, and malar height—using 3-month postoperative computed tomography images and performed statistical analyses to compare the results of the two methods.
Results
All three measurements (zygomaticofrontal suture, inferior orbital wall, and malar height) showed significant differences (p<0.05) between one-point and two-point fixation. Highly significant differences were found for the zygomaticofrontal suture and malar height parameters. The difference in the inferior wall measurements was less meaningful, even though it also reached statistical significance.
Conclusion
Using three parameters in a statistical analysis of imaging findings, this study demonstrated significant differences in treatment outcomes according to the number of fixations. The results indicate that bone alignment and continuity can be achieved to a greater extent by two-point fixation instead of one-point fixation.
INTRODUCTION
Zygoma complex fractures affect one of the most important buttresses of the face, impacting structural and aesthetic aspects of facial appearance. Therefore, their treatment is of crucial importance in trauma surgery [1,2].
In general, internal fixation of the buttress is performed using an intraoral approach, a subciliary incision, and a lateral eyebrow incision to reduce the fracture and maintain the facial contour [2,3].
Incision sites are determined according to the operator’s judgment, and this choice is therefore subjective to some extent. Zygoma complex fractures occur within the three-dimensional face structure, many aspects of which are complex and difficult to define objectively. Hence, studies have reported various results regarding the maintenance of bone stability after surgery according to differences in the number of fixations in classical surgical methods.
Although previous studies have reported that one-point fixation through the oral approach is sufficient [4,5], few studies have compared the results according to the number of fixations. Therefore, it is necessary to address this gap in the literature by comparing the surgical results of one-point and two-point fixation.
In contrast, multiple studies have compared two-point versus three-point fixation [6–8]. One study, which compared one-point and two-point fixation using X-rays, argued that two-point fixation was superior for bone stability to one-point fixation [9]. Computed tomography (CT) is considered the gold standard for diagnostic imaging and assessment of postoperative results in facial bone, the three-dimensional structure of which is relatively complex and important [10]. For this reason, we think that anatomical measurements using CT would be more accurate than comparisons using X-rays. Therefore, we compared parameters through an analysis of anatomic landmarks on CT.
METHODS
Patient selection
From March 2018 to May 2020, patients randomly underwent surgery using one of two surgical methods who had unilateral zygoma complex fractures requiring surgery into two groups. Patients with multiple facial fractures involving the nasal bone, frontal bone, or mandible were excluded. The first group comprised 22 patients who underwent one-point fixation using only an oral incision, while the second group contained 33 patients who underwent two-point fixation using an oral incision and a lateral eyebrow incision. These 55 patients underwent orbital plain computed tomography (PCT) 3 months postoperatively. Based on the PCT results, we proposed three parameters for evaluating the alignment of zygoma complex fractures and performed a statistical analysis to compare the surgical results between both groups.
The two groups of patients were randomly allocated to receive either one-point or two-point fixation. The operator, surgical method, plate shape, and surgical material were the same in all patients to control for the possible influence of these variables.
Surgical method
In the one-point fixation group, an intraoral incision was made from immediately next to the Stensen’s duct orifice to the lower part of alar cartilage, just next to the nasal septum through the patient’s lesion side. The fracture was reduced through gingivobuccal incision and fixed using a four-hole L-type plate (thickness: 1 mm), unsintered hydroxyapatite particles, poly-L-lactic composites (OSTEOTRANS MX; Takiron Co., Ltd., Tokyo, Japan), and 4-mm screws.
In the two-point fixation group, the incision was made using the same method through the same oral approach as in the one-point fixation group, and an additional incision on the lateral eyebrow was performed considering the fracture line of the lateral orbital rim. After sufficient fracture reduction through both incisions, one-point fixation was performed on the zygomaticomaxillary (ZM) buttress using the same material as in the one-incision group, followed by another fixation along zygomaticofrontal (ZF) suture using a linear four-hole plate through the lateral eyebrow incision.
CT analysis
Using orbital PCT scans obtained 3 months after surgery, measurements were made at three points relative to the non-operated side. These measurements were used for between-group statistical comparisons of the surgical results. To ensure consistency, the measurements were all conducted in the same way.
The measurements were performed after a sufficient recovery period (3 months after surgery), during which bone remodeling and ossification of the fracture line occurred. Therefore, precise measurements were possible. This period also encompassed functional recovery (e.g., mastication, mouth opening, and vision), and swelling and ecchymosis were sufficiently reduced.
We measured the parameters at the following three locations to evaluate bone alignment and continuity after zygoma complex fracture surgery: the ZF suture, infraorbital wall, and malar height. These are traditionally used sites in three-point open reduction and internal fixation, and constitute a major buttress for achieving stability of the mid-face.
The text below presents descriptions of each measurement method used to obtain the three parameters. These methods are illustrated using an orbital PCT scan of a 36-year-old male patient who underwent surgery using one-point fixation after a right zygoma complex fracture.
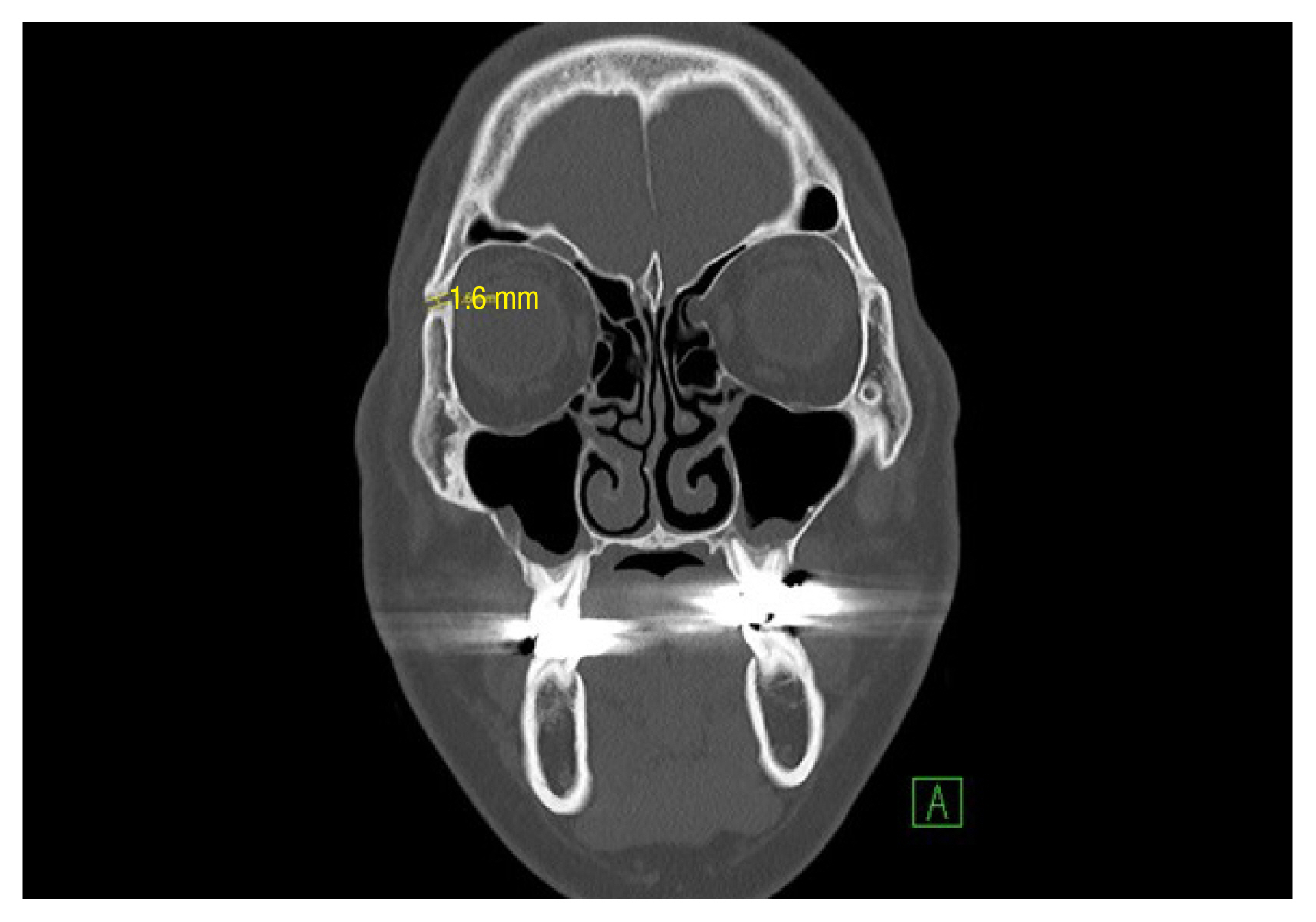
ZF suture
The bone gap in the ZF suture was measured on a coronal view of orbital PCT. First, lines were drawn along the proximal and distal areas parallel to the cross-section of the bilateral fracture line. Next, the longest vertical line connecting those two lines was drawn and the length of the ZF suture bone gap was measured (Fig. 1).
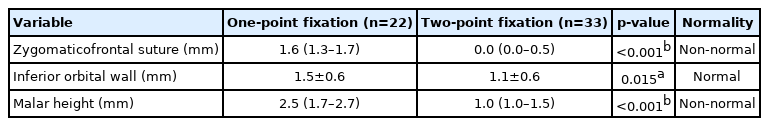
Inferior orbital wall
In order to indirectly evaluate the structural stability of the inferior orbital wall, we decided to use a landmark on the sagittal view of the orbital PCT. An imaginary line extending the infraorbital rim and the anterior border of the inferior orbital fissure was first drawn on the sagittal plane of orbital PCT. Next, a vertical straight line was drawn from this line to the deepest part of the inferior orbital area, and this line was defined as the floor depth [10,11]. The difference in floor depth between the non-operated side and the operated side was used in the statistical analysis (Fig. 2).
Measurement of the inferior orbital wall. An imaginary line extending the infraorbital rim and the anterior border of the inferior orbital fissure was first drawn on the sagittal plane of orbital PCT. Next, a vertical straight line was drawn from this line to the deepest part of the inferior orbital area, and this line was defined as the floor depth. Measurements were made on the non-operated side (A, 3.2 mm) and the operated side (B, 4.2 mm). The difference was 1 mm in this patient was 1 mm.
Since a gentle curve passing through the inferior orbital rim and floor, and then dipping and passing through the inferior orbital fissure, is an important index of structural stability of the inferior wall and floor repair, we used the floor depth as a parameter for the statistical analysis of structural stability.
Malar height
The position of the malar eminence was defined as the most protruding point of the zygomatic bone on the zygomatic complex from the axial cut covering most of the bilateral zygomatic complex region.
The extent of depression was defined as the vertical distance on PCT (axial view) between a horizontal line that passed through the anterior border of the foramen magnum, drawn from the highest malar eminence of the non-operated side, and another horizontal line drawn from the apex of the maxilla on the operated side [5,12].
The difference between these two distances was used as the parameter of malar height (Fig. 3).
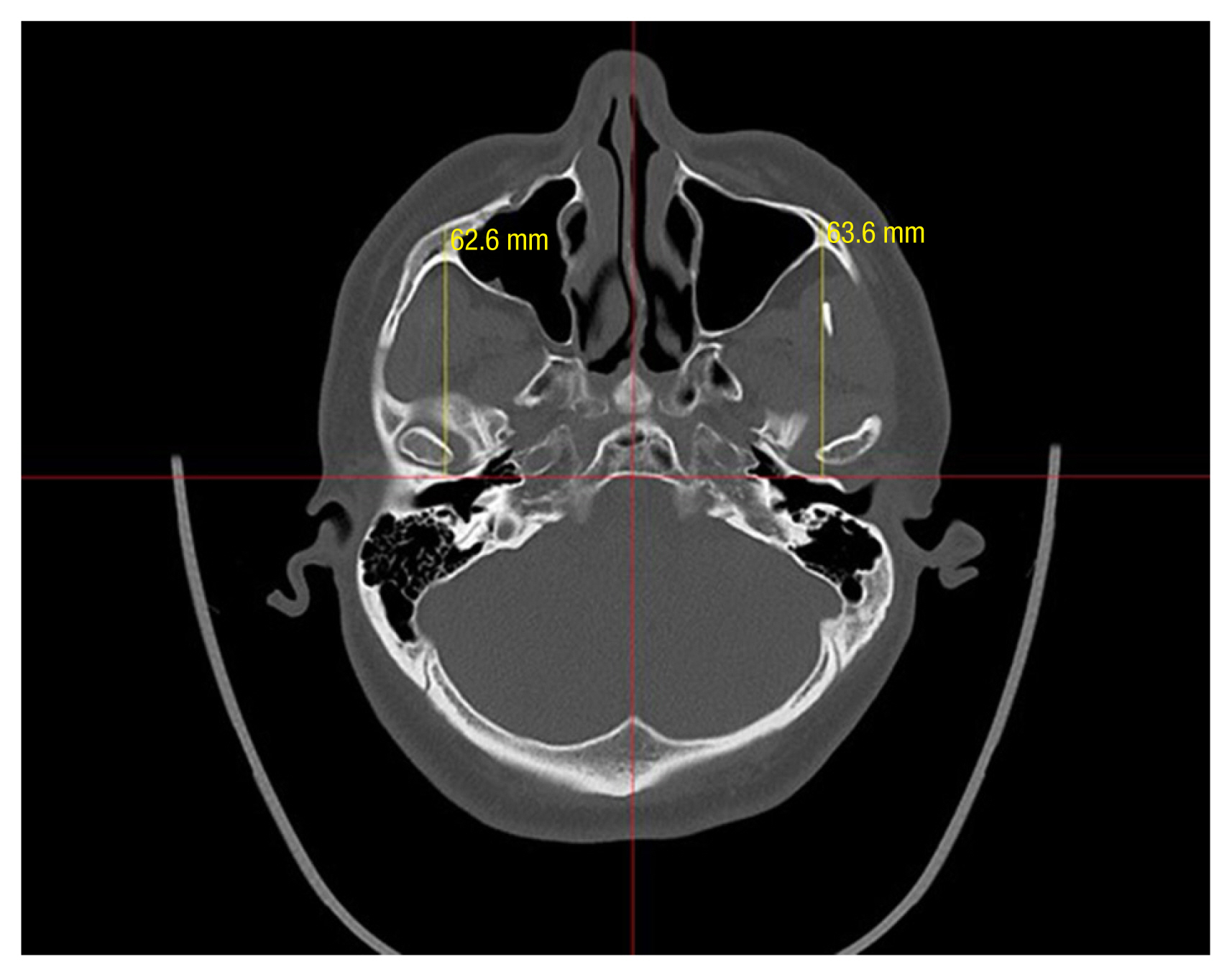
Measurement of the malar height. First, drawn horizontal line passing through the anterior edge of the foramen magnum on the coronal plane of orbital PCT. Next draw a vertical line from this line to the malar eminence on both sides. In this figure, the measurement on the non-operated side was 63.6 mm, and that on the operated side was 62.6 mm. The difference between the two distances was 1 mm in this patient.
Statistical analysis
Statistical analyses were performed under the assumption that each patient was an independent sample. As the ZF suture and malar height did not show a normal distribution of data, the Wilcoxon rank sum test (a nonparametric test method) was used. For the inferior orbital wall, which showed a normal data distribution, the independent t-test was performed. The analysis was conducted in R (version 4.0.2) [13], and the figures were produced using the ggpubr package (version 0.4.0) [14].
RESULTS
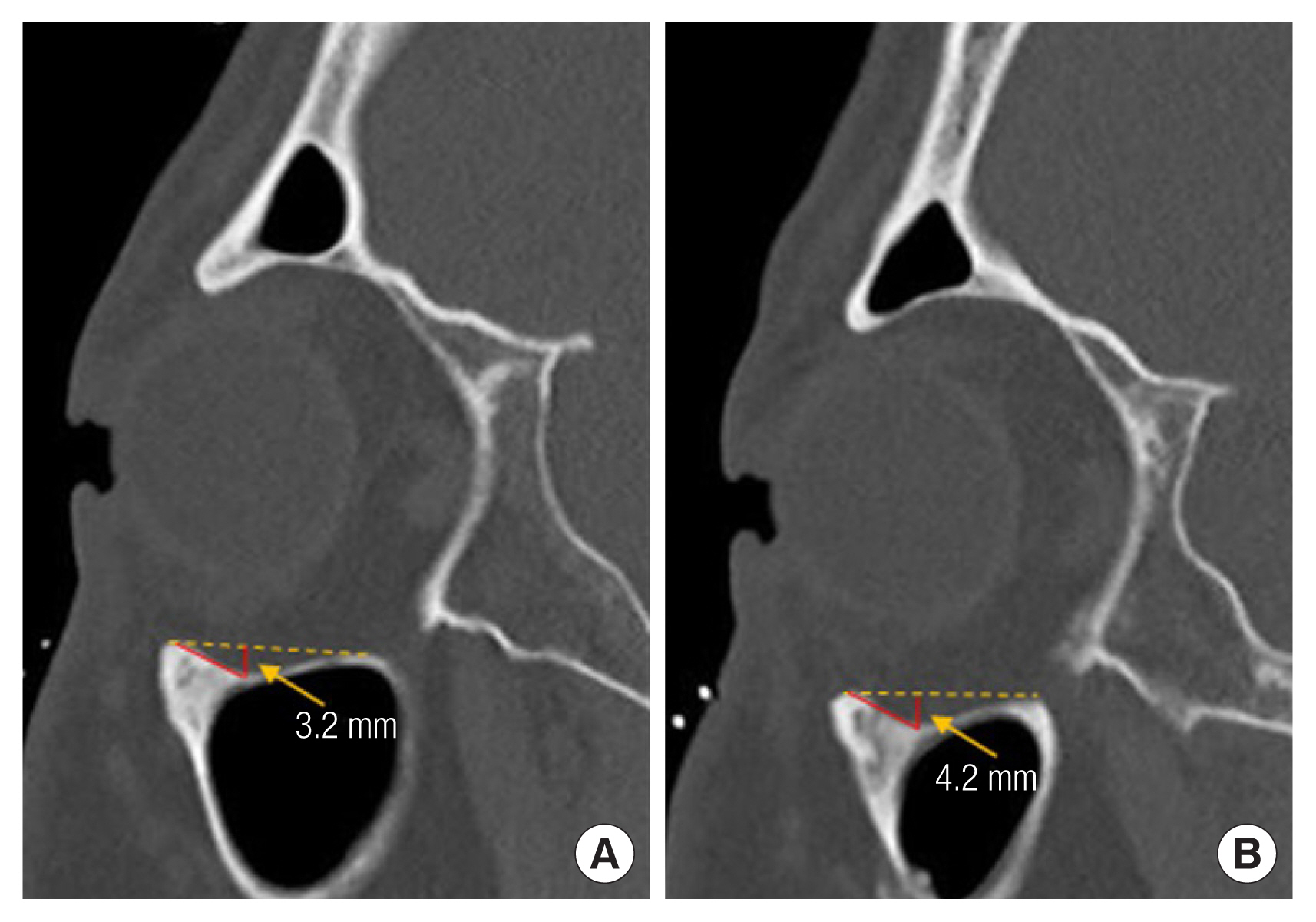
Table 1 summarizes and compares the three measurements in the one-point fixation group (n=22) and the two-point fixation group (n=33), to which patients were randomly allocated. Figs. 4–6 present a visualization of these values (maximum, minimum, median, and quartile deviation) to enable a straightforward interpretation of the distribution of the measurements and their extreme values.
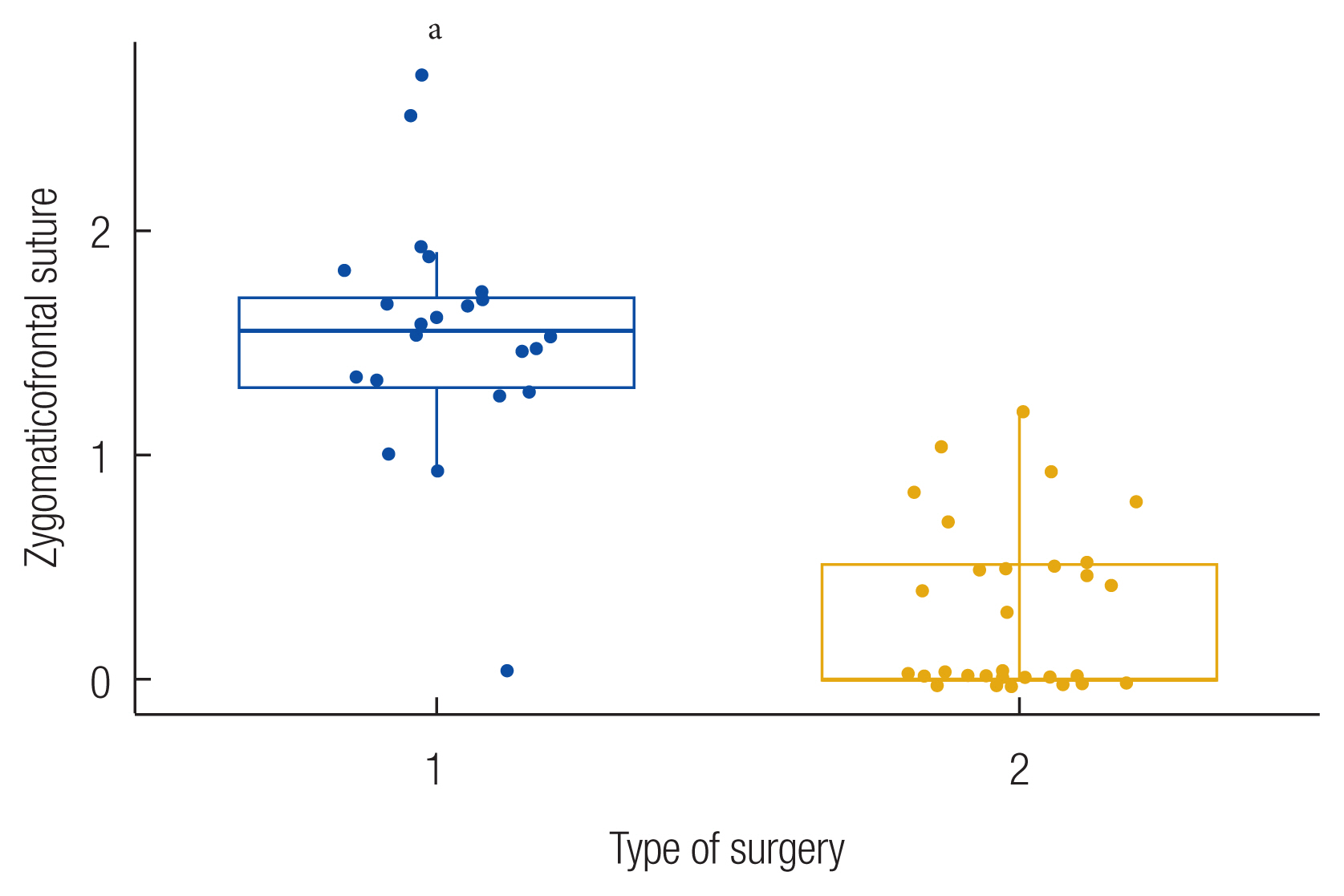
Box plot for the zygomaticofrontal suture showing that more favorable correction results were achieved with the two-point fixation method. aStatistically significant differences between the two surgical methods (p<0.001).
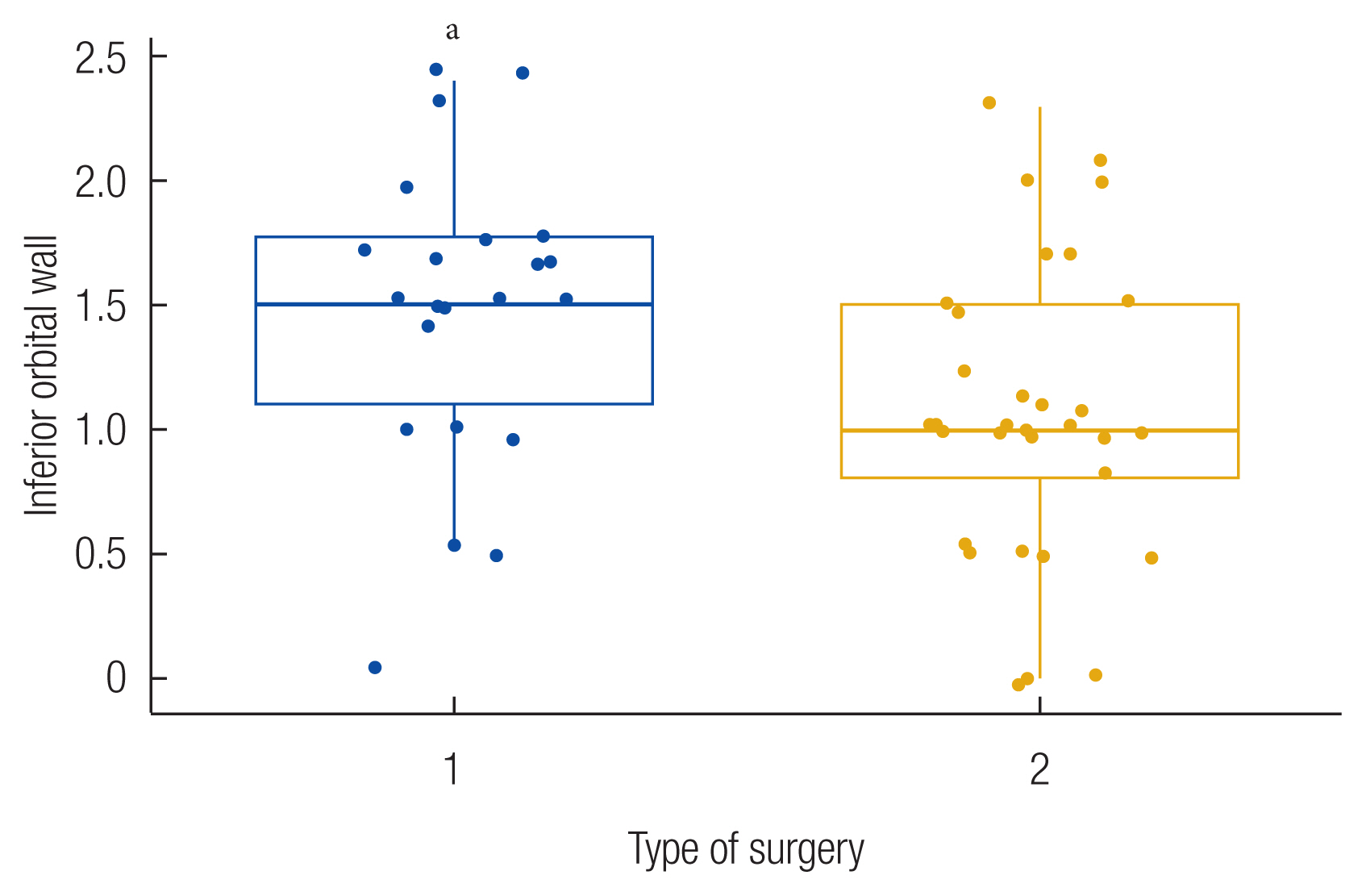
Box plot for the inferior orbital wall showing that two-point fixation led to more favorable correction results, but with relatively low statistical significance compared to the values for the ZF suture and malar height. aStatistically significant differences between the two surgical methods (p≤0.05).

Box plot for malar height showing that two-point fixation showed more favorable correction results than one-point fixation. aStatistically significant differences between the two surgical methods (p<0.001).
The median ZF suture bone gap measurement in the one-point fixation group was 1.6 mm, while the first quartile (25th percentile) was 1.3 mm and the third quartile (75th percentile) was 1.7 mm. In the two-point fixation group, the median value was 0 mm, the first quartile was 0 mm, and the third quartile was 0.5 mm (Table 1). A box plot (Fig. 4) indicates that the bone gap of the ZF suture was noticeably and significantly narrower in the two-point fixation group (p<0.001).
The mean inferior orbital wall measurements were 1.5±0.6 mm in the one-point fixation group and 1.1±0.6 mm in the two-point fixation group (Table 1). The two-point fixation group showed a significantly smaller difference in floor depth between the operated side and the non-operated side (p= 0.015). As shown in Fig. 5, these measurements had a wider distribution than the other parameters (Figs. 4, 6) and the level of statistical significance was also lower.
The median value for the malar height was 2.5 mm in the one-point fixation group (first quartile: 1.7 mm and third quartile: 2.7 mm). The median value in the two-point fixation group was 1.0 mm (first quartile: 1.0 mm and third quartile: 1.5 mm). As depicted in the box plot (Fig. 6), the two-point fixation group showed a significant difference in malar height between the operated side and non-operated side compared to the one-point fixation group (p<0.001).
Summarizing these results, the two-point fixation method including a ZF suture showed better surgical results in terms of these three measurements than the one-point fixation method, which involved fixation only on the ZM buttress. Therefore, bone alignment and continuity were achieved more precisely and better maintained using two-point fixation than using one-point fixation.
DISCUSSION
The treatment of zygoma complex fractures, which have a complex three-dimensional mechanical structure, is challenging. In order to obtain satisfactory surgical results, both aesthetically and functionally, fixation should be performed with an appropriate approach and accurate reduction. Traditionally, zygoma complex surgery with a three-point incision approach and a three-point fixation has been preferred [6], but a study reported that one-point or two-point fixation could achieve stability similar to that obtained using three-point fixation [15].
One study reported that aesthetic and functional requirements could be achieved with one-point fixation on the ZF suture [16]. Other studies showed that satisfactory surgical results could be obtained using one-point fixation through the oral approach [4,5]. Nonetheless, the number of plates required for adequate fixation remains a matter of debate.
A previous study used X-ray scans to compare surgical results between one-point and two-point fixation in zygoma complex fractures, with measurements performed at the same fixation positions as in our study. That study argued that two-point fixation showed superior results for bone stability [9]. Since CT is considered the gold standard for evaluating postoperative results and making anatomical measurements of facial bone fractures, which have a complex three-dimensional structure [10], CT is more appropriate to evaluate whether adequate postoperative results have been achieved in facial bone.
In our study, the results of two surgical methods (one-point and two-point fixation) for unilateral zygoma complex fractures were quantified using postoperative PCT.
Although other studies using PCT reported that one-point fixation was sufficient [4,5], these studies did not compare the surgical results with those using the two-point fixation method. Through a comparison of these two surgical methods via statistical analyses and visualization, this study demonstrated that there were significant differences in the treatment results.
Meanwhile, two-point fixation has disadvantages in terms of a longer operating time and implant palpability [9]. The higher number of fixations may also be a disadvantage due to aesthetically unfavorable scars. Nonetheless, since research on surgical methods for scar reduction continues to be conducted [17], we think that it would be more appropriate to choose the surgical method with a focus on appropriate reduction and maintenance of bone stability.
The occurrence of complications according to different numbers of fixation points should also be considered. One study reported that decreases in malar height and vertical dystopia occurred more frequently in cases with fewer fixation points [18]. Another study argued that three-point fixation was more stable in terms of malar height and mouth opening than two-point fixation due to the weaker influence of masticatory forces during the healing phase [6]. In contrast, there are complications that occur less frequently with fewer fixation points. Studies have reported that postoperative facial and neurological complications were less common in patients who underwent two-point fixation than three-point fixation [7]. and that scar formation occurred more frequently in two-point fixation than one-point fixation [9].
A possible explanation for why the statistical correlation of the inferior orbital wall in this study was lower than that of the other two factors might be the fact that fixation was not performed directly on the infraorbital wall through a subciliary incision. If fixation had been performed on the infraorbital wall, it is expected that higher correlation results would have been obtained.
A limitation of the bone gap measurements in this study is that we did not consider differences in individual patients due to facial asymmetry. However, parameters were measured accurately and precisely, and statistically significant results were derived from these two groups with a relatively large number of samples. Therefore, we think that the results are meaningful despite the fact that asymmetry was not considered.
Nonetheless, this study demonstrated that making two incisions and fixations enables more precise correction to a statistically significant degree. Therefore, we hope that this study will help to construct an objective, data-driven basis for determining the incision site for open reduction and internal fixation of zygoma complex fractures, which to date has depended on operators’ subjective judgment.
Contrary to a previous study arguing that more extensive incisions did not have a significant impact on surgical outcomes, stating that aesthetic and functional requirements could be achieved only with one-point fixation on the ZF suture [16], we identified statistically significant differences. Specifically, two-point fixation showed better surgical results than one-point fixation based on accurate and precise measurements.
In this study, we compared the surgical results of one-point fixation and two-point fixation methods for the fixation of the ZF suture and ZM buttress. If similar studies are conducted in the future. For example, fixing the inferior orbital rim and ZM buttress may be compared with only fixation in ZM buttress. If such research will accumulate, it would facilitate more stable and aesthetic surgery and be helpful for operators in choosing the surgical method that is most suitable for each case. Furthermore, it will be possible to create objective, statistically supported criteria for the evaluation of postoperative results.
Abbreviations
CT
computed tomography
PCT
plain computed tomography
ZF
zygomaticofrontal
ZM
zygomaticomaxillary
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Gyeongsang National University Hospital (IRB No. GNUH 2021-11-010) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Author contribution
Conceptualization: Nam Gyun Kim. Data curation: Gi Cheol Do, Nam Gyun Kim. Formal analysis: Kyung Suk Lee, Gi Cheol Do. Methodology: Jun Sik Kim. Project administration: Kyung Suk Lee, Jun Sik Kim, Nam Gyun Kim. Visualization: Gi Cheol Do. Writing - original draft: Gi Cheol Do. Writing - review & editing: Jae Bong Shin. Investigation: Jae Bong Shin, Min Hyung Kim. Resources: Min Hyung Kim. Software: Gi Cheol Do. Supervision: Kyung Suk Lee, Jun Sik Kim, Nam Gyun Kim.