|
 |
- Search
| Arch Craniofac Surg > Volume 23(4); 2022 > Article |
|
Abstract
Plastic surgery around the eyes is usually performed under local anesthesia, using a mixture of lidocaine and epinephrine. Blindness is a rare but devastating complication after the injection of local anesthesia in this region. Most cases reported to date have been caused by occlusion of the ophthalmic artery or central retinal artery. In this case report, however, we present a highly unusual case of blindness caused by corneal edema after a local anesthetic injection. A patient visited the emergency room with a laceration on the eyebrow, and local anesthesia was injected before suturing. Immediately after the injection, severe corneal edema developed, making it impossible to observe the structures in the anterior chamber in detail or check the light reflex and visual acuity of the naked eye. An antibiotic (moxifloxacin hydrochloride) and high-concentration steroid eyedrops were promptly applied. High-concentration steroids were also administered orally. On day 13 post-injury, the visual acuity of the naked eye improved to 1.0, and no recurrence of corneal lesions was observed. Although the cause of corneal edema after the local injection could not be conclusively identified, we hope that this report will help raise clinicians’ awareness of this complication and appropriate treatment methods.
Plastic surgery around the eyes is usually performed under local anesthesia using a mixture of lidocaine and epinephrine. Blindness after a local anesthesia injection is a rare but devastating complication.
Several studies have documented blindness after injection of local anesthesia in the facial area [1–7]. The most commonly reported causes of this complication are occlusion of the ophthalmic artery or central retinal artery [6,7]. In contrast, very few cases of corneal edema after a local anesthetic injection have been reported. In this paper, we report the clinical symptoms of such a case and describe the recovery process. Through this report, we hope to raise clinicians’ awareness of this complication, thereby reducing the risk of its occurrence, and share information on treatment methods.
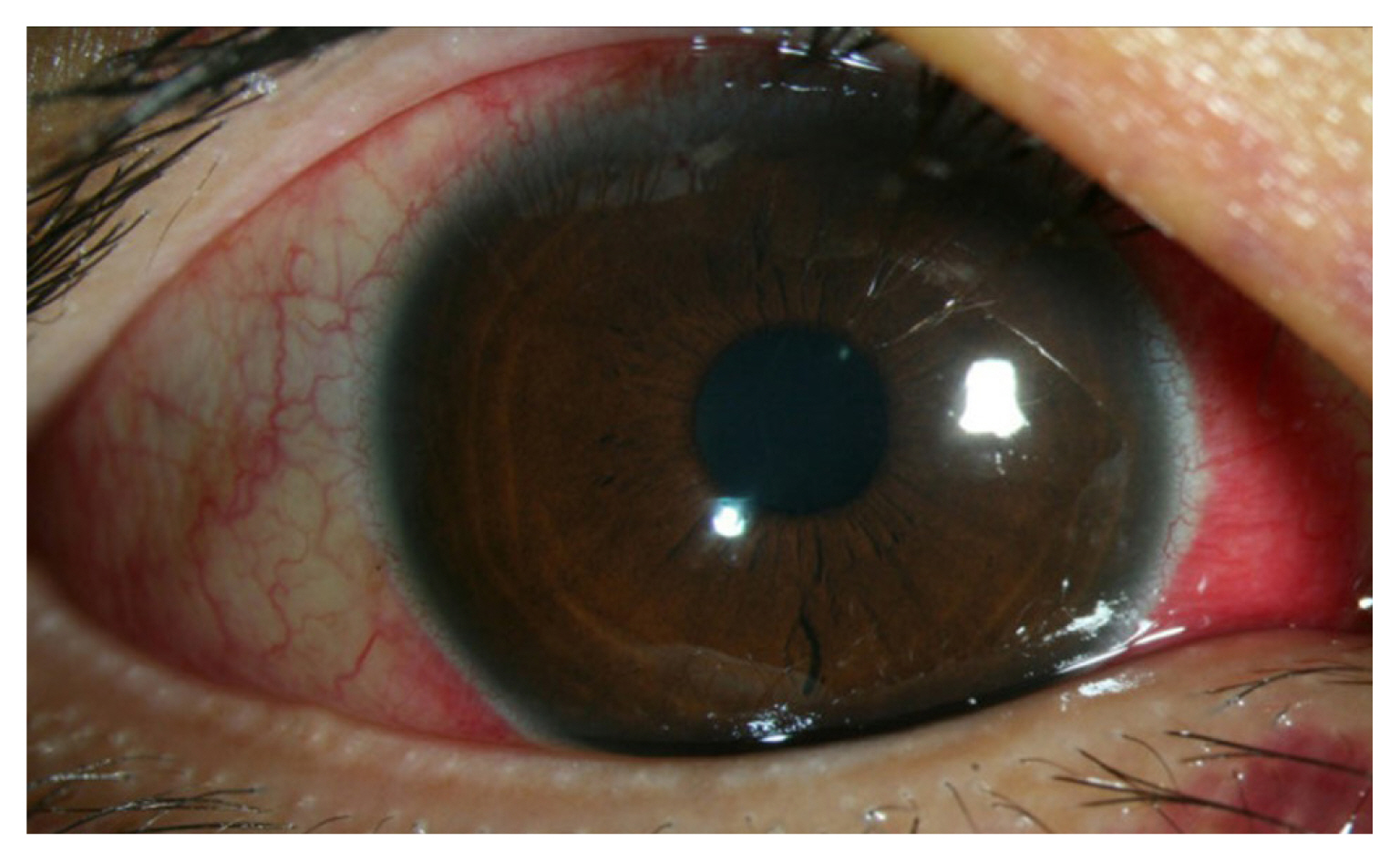
A 29-year-old man visited the emergency room with an eyebrow laceration caused by an assault (Fig. 1). The patient was alcohol-intoxicated and did not cooperate well. To suture the laceration site, a local anesthetic containing 2% lidocaine and 1:100,000 epinephrine, was injected along the circumference of the eyebrow laceration using a 30-gauge, 0.3×21 mm needle.
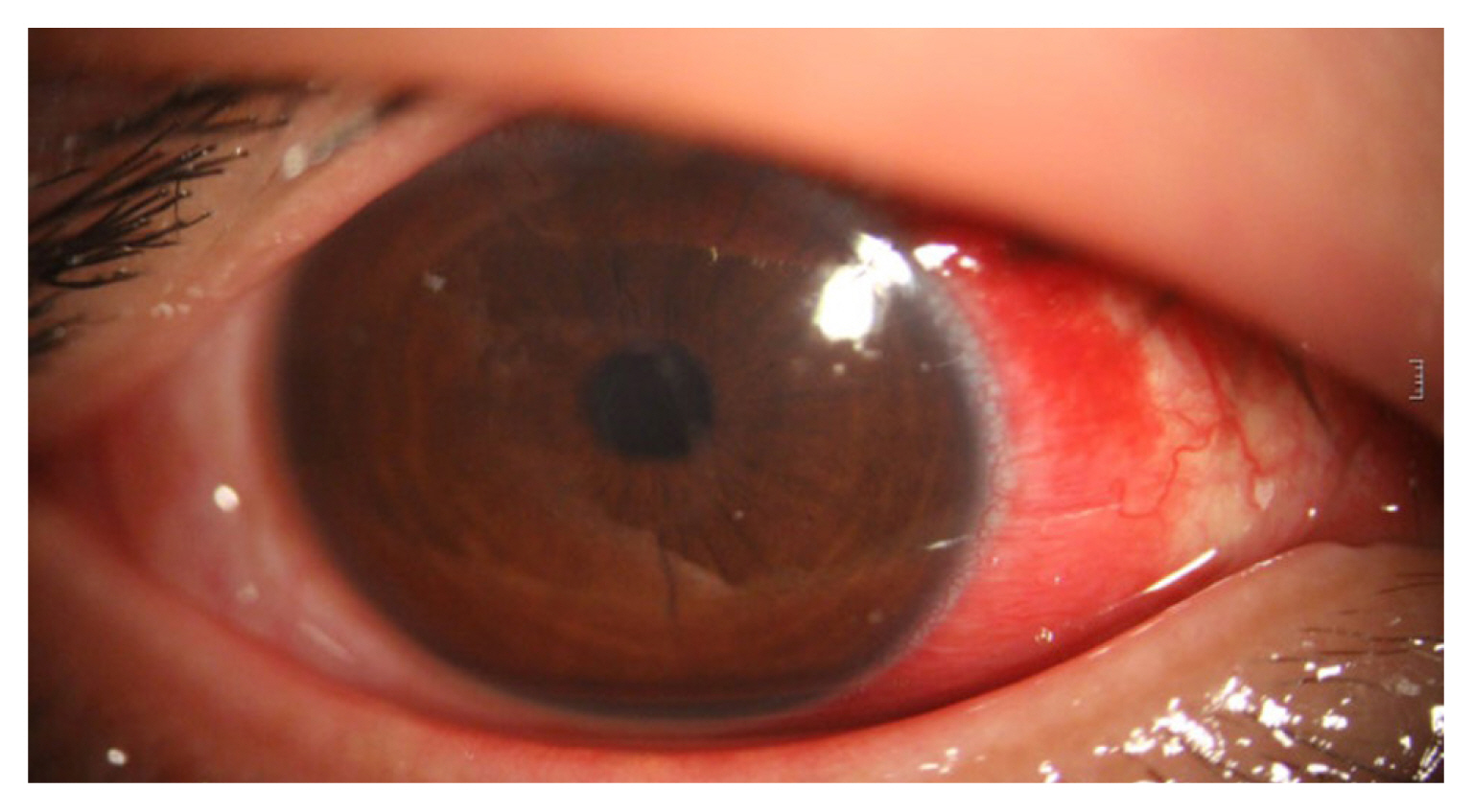
After the injection, the patient complained of pain and blurred vision. The procedure was stopped and we consulted an ophthalmologist, who observed corneal edema upon examination of the anterior segment through wide-angle safety imaging. The corneal edema was severe, to the point that it was not possible to observe the structures in the anterior chamber in detail or to check the light reflex and visual acuity of the naked eye (Fig. 2).
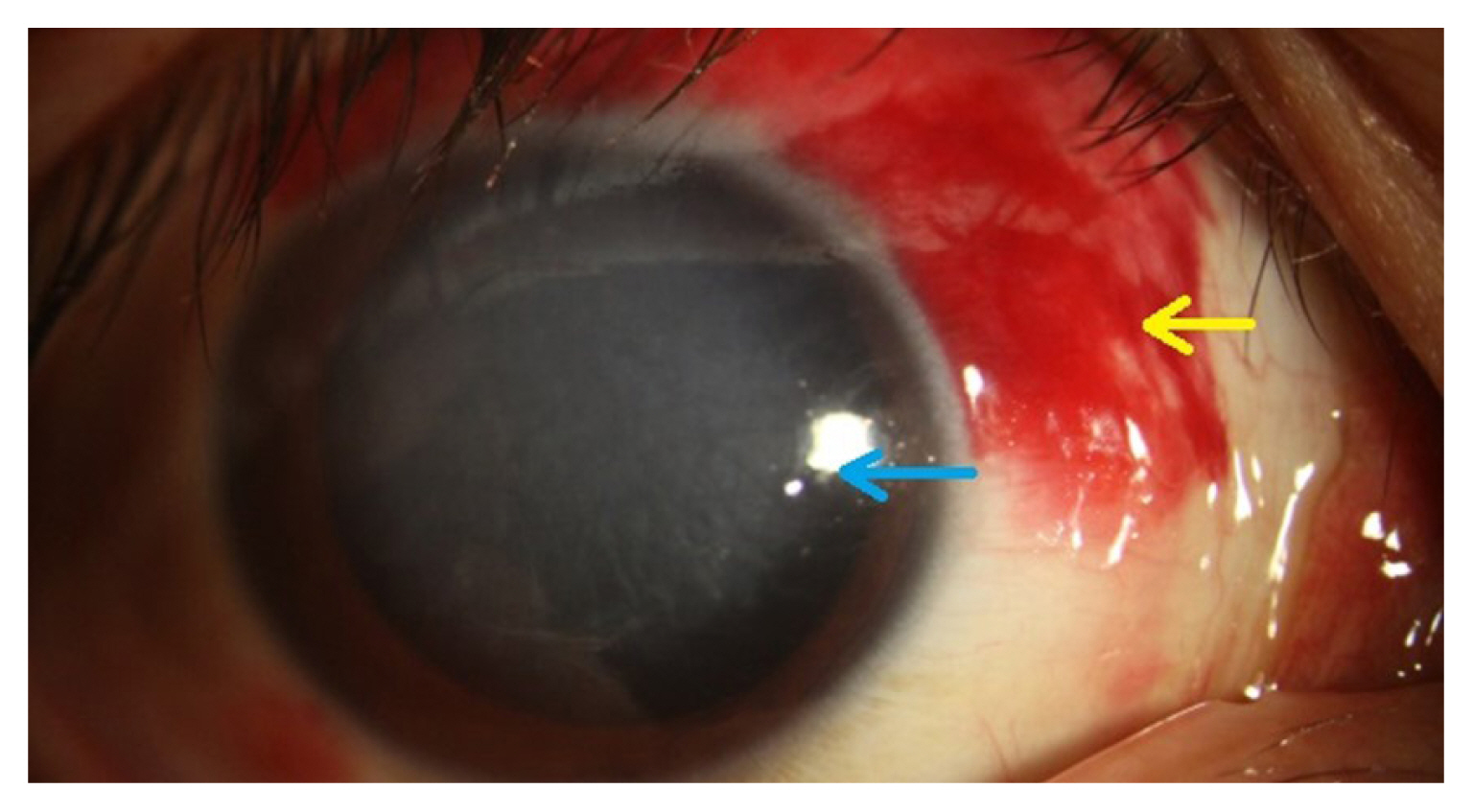
Moxifloxacin hydrochloride and high-concentration steroid eyedrops were applied within 1 hour after the injection of local anesthesia. In addition, high-concentration steroids were administered orally. On the day after the injury, the pupil light reflex was confirmed to be intact, and subjective visual acuity improvement began (Fig. 3).
The visual acuity of the naked eye improved to 0.32 on the 3rd day after the injury, but inflammatory findings in the anterior chamber were seen and corneal edema continued. The intraocular pressure increased due to the use of steroid eyedrops, and the steroid dose was rapidly reduced.
On the 4th day after injury, the visual acuity of the naked eye improved to 0.63, intraocular pressure was normal, and corneal edema was limited to the central area (Fig. 4). On the 10th day after the injury, the visual acuity of the naked eye was 0.63 and the corneal edema had disappeared. Closed reduction of the nasal bone fracture was performed under general anesthesia after determining that doing so would be possible considering the improved state of the patient’s eye. On the 13th day after the injury, the visual acuity of the naked eye improved to 1.0, and no recurrence of corneal lesions was observed.
In this case, the cause of corneal edema after local injection could not be conclusively identified, but several possible causes are suggested.
The first possibility relates to the epinephrine component of the local injection. Epinephrine acts peripherally on α-adrenergic receptors, resulting in the constriction of blood vessels. It is possible that corneal edema may have occurred due to ischemic damage resulting from constriction of the vessels feeding the cornea. A study documented blindness caused by anterograde migration of epinephrine and lidocaine, which induced peripheral vascular constriction and spasm, contributing to peripheral nonperfusion [7]. However, vasoconstriction and spasm usually result in partial dilatation of the pupil, and corneal edema is unlikely. Therefore, it is improbable that epinephrine was the cause of corneal edema in this case.
A second possibility is embolism. The supraorbital and supratrochlear arteries lead to the ophthalmic artery. In a previously published case, ophthalmic artery occlusion occurred after local anesthesia injection in the subcutaneous supratrochlear area [7]. Considering the location of the laceration (adjacent to the supraorbital and supratrochlear arteries), the possibility of embolism into the ophthalmic artery cannot be excluded. However, only corneal edema occurred, and no additional retinal damage was found. This is different from the findings of arterial occlusion; therefore, embolism is also an unlikely explanation.
The third possibility is that anesthesia may have been injected directly into the cornea. Local anesthesia was injected along the subcutaneous layer of the eyebrow laceration, but the patient’s degree of cooperation at that time was low. If a patient moves due to pain when anesthesia is being administered, partially penetrating the cornea is possible. The appearance of subconjunctival hemorrhage from the upper side, as shown in Fig. 2, is consistent with the possibility of penetration. Another case has been reported of temporary blindness due to the direct injection of filler into the cornea [8].
Multiple reports have described blindness after local anesthesia injections. One case was caused by an injection of lidocaine as local anesthesia into the corneal stroma during plastic surgery [2]. However, the cause of corneal edema in that case was clearly direct injury of the cornea during surgery, unlike in our case. Furthermore, the patient received appropriate treatment after being transferred to a hospital with an ophthalmologist. Although it was not precisely stated, it would be expected that more time would be needed until the initial treatment. It took 4 months for the patient to recover vision, and an additional gas injection procedure was also required. Another case of ophthalmic artery occlusion occurred after local anesthesia injection into the supratrochlear area [7]. However, that case progressed to permanent visual loss, which is a substantial clinical difference from this case, in which corneal edema occurred.
We think that steroids and antibiotics played an important role in the course of this case. Steroids are effective in reducing anterior segment inflammation and, consequently, corneal edema. In particular, steroids inhibit new lymphatic vessel growth in the cornea by suppressing macrophage infiltration and pro-inflammatory cytokine expression and directly inhibiting the proliferation of lymphatic endothelial cells. In addition, antibiotics can prevent secondary infections after corneal edema. It is important to use broad-spectrum antibiotics [9]. For this reason, we immediately responded to this case by administering a combination of steroids and antibiotics.
To summarize, we immediately consulted an ophthalmologist for a patient who developed blindness due to corneal edema after an injection of local anesthesia, and obtained good results by administering appropriate treatment. In the field of plastic surgery, this is the first case to describe corneal edema after a local injection, and we hope that this report will raise clinicians’ awareness of this possible complication and disseminate knowledge regarding appropriate treatment strategies.
Notes
Ethical approval
This study was approved by the Institutional Review Board of Pusan National University Hospital (IRB No. 2205-031-115).
Patient consent
The patient provided written informed consent for the publication and the use of his images.
Author contribution
Conceptualization: Seong Hwan Bae. Data curation: Kyoung Eun Kim, Yeon Ji Jo. Formal analysis: Kyoung Eun Kim, Jae Woo Lee. Project administration: Taewoo Kang, Heeseung Park. Visualization: Heeseung Park. Writing - original draft: Jung Hyun Hong. Writing - review & editing: Jung Hyun Hong. Investigation: Jung Hyun Hong, Yeon Ji Jo. Supervision: Seong Hwan Bae, Taewoo Kang, Yeon Ji Jo. Validation: Jae Woo Lee.
Fig. 1
A 29-year-old man with an eyebrow laceration. Asterisk mark indicates the injection site of a local anesthetic.

Fig. 2
Anterior segment photography immediately after injection of local anesthesia. Corneal edema (blue arrow) and subconjunctival hemorrhage (yellow arrow) on the upper side. The light reflex and visual acuity of the naked eye could not be checked due to severe corneal edema.
REFERENCES
1. Ghosh S, Mukhopadhyay S, Mukhopadhyay S, Roy R, Dutta H. Inadvertent intracorneal injection of local anesthetic during lid surgery. Cornea 2010;29:701-2.


2. Kim BR, Park SY, Lee HK, Seo KY, Kim EK, Kim TI. a case of descemet’s membrane detachment during lidocaine injection for hordeolum incision and drainage. J Korean Ophthalmol Soc 2016;57:1790-4.


3. Bektas D, Kul N, Akyol N, Ural A, Caylan R. Temporary blindness and ophthalmoplegia due to local anesthetic infiltration of the nasal septum. Ear Nose Throat J 2012;91:E1-3.


4. Medina FM, Pierre Filho Pde T, Freitas HB, Rodrigues FK, Caldato R. Blindness after cosmetic blepharoplasty: case report. Arq Bras Oftalmol 2005;68:697-9.


5. Barodiya A, Thukral R, Agrawal SM, Rai A, Singh S. Tempo rary blindness after inferior alveolar nerve block. J Clin Diagn Res 2017;11:ZD24-5.



6. Bacsik C, Cohen A, Cutilli B, Lucyk D, Carson H, Fielding AF. Blindness secondary to injection in the nose, mouth, and face: cause and prevention. Ear Nose Throat J 1995;74:493.


7. Moon BG, Kim JG. A case of ophthalmic artery occlusion following subcutaneous injection of epinephrine mixed with lidocaine into the supratrochlear area. Korean J Ophthalmol 2017;31:277-9.




- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 3,125 View
- 87 Download
- Related articles in ACFS