Abbreviations:
Rhinoplasty Outcome Examination
;
Septo-turbinoplasty Outcome Examination
.
INTRODUCTION
Reconstruction of secondary cleft lip nose deformities is challenging even for experienced craniofacial surgeons. However, there is no ŌĆ£gold standardŌĆØ operative technique, as numerous methods have been introduced in the literature. Some methods involve the use of autologous tissues, such as dermofat, cartilage, and bones, and foreign body insertion [
1,
2]. However, each method has its advantages and disadvantages in view of the long-term postoperative outcomes.
Cartilage grafts have potential problems, such as warping, resorption, visible irregularities, and donor site morbidities. First author (CKL) reported also the manuscript of ŌĆ£Total en bloc reconstruction of alar cartilage with conchal cartilageŌĆØ at 2000 [
3]. In some patients, re-operations were attempted for the correction of the unnatural and bulky nose after growth. Moreover, foreign body insertion has other potential complications such as infection, implant malposition, and extrusion. Above all, the most serious problem is an unnatural and unsatisfactory outcome; as a result, patients wander from one clinic to another for reoperation throughout life.
Our basic concept for correction is wide mobilization and remodeling of the deformed lower lateral cartilage, and the use of various suture techniques without any transplantation. These techniques enable rotation or de-rotation, lengthening or shortening, and projection or reduction of the collapsed nasal tip with sufficient redraping of the soft tissue envelop by wide undermining of soft tissue envelop.
In primary repair, a concept of non-destructive and functional repair has been introduced, which is characterized by restoring the balanced shape and position in cleft and non-cleft sides together with septo-turbinoplasty [
4]. However, secondary operative cases were another concept which had to for distorted the original anatomy and shredded the lower lateral cartilages. Therefore, more complicated procedures tried additional medial crural spanning sutures to obtain a more rigid tripod or tetrapod support of the nasal tip pyramid. Herein, we present our 15-year experience based on general principles of esthetic and functional rhinoplasty of unilateral secondary cleft lip nose deformities.
METHODS
From 2005 to 2019, 150 patients who had secondary cleft lip nose deformities were reviewed retrospectively. Nearly all patients had undergone primary surgery of the unilateral cleft lip. Some patients already had primary or secondary rhinoplasty. Regardless of the patientŌĆÖs surgical history, all patients underwent surgery following the same techniques.
Study design
Questionnaires evaluating esthetic and functional satisfaction were sent to patients through Google Forms. All responses in completed questionnaires including patient demographics, number of surgeries, and satisfactory results were extracted for analysis.
When analyzing the questionnaire responses ŌĆ£absolutely yes,ŌĆØ ŌĆ£very much,ŌĆØ and ŌĆ£more or lessŌĆØ were classified as positive, whereas ŌĆ£littleŌĆØ and ŌĆ£absolutely noŌĆØ were taken as negative answers. Statistical analysis was conducted by scoring the number of positive answers. Two-sided t-test was performed comparing mean of scores according to variable factor. A stepwise method was selected for the analysis. Statistical analyses were performed using IBM SPSS version 23 (IBM Corp., Armonk, NY, USA) software. Statistical significance was set at p<0.05.
Surgical technique
Primary operation
Under either local anesthesia with regional nerve block or general anesthesia, markings and calculations were made along the anatomical landmarks, namely, tip-defining points and width, nasion width, dorsal midline from the nasion to the imaginary tip, bi-alar width and height, nostril sill width, supra-alar crease, etc.
For open rhinoplasty, the incision was made in a marginal and stair-step transcolumellar fashion with a crescent excision of the alar web for a supposed adult nostril shape in accordance with the axis, height, width, and contour (
Fig. 1A).
Open rhinoplasty was performed for near-total skeletonization of bony and cartilaginous structures including the deviated septum to assure symmetric soft tissue mobilization and envelope. This is one of the most important procedures for soft tissue redraping by dorsal and vestibular lining and for attaining optimal long-term results. Wide undermining was performed on the subperichondral and subperiosteal planes. The scroll area was completely released along the upper and lower lateral cartilages with the dorsum and submucoperichondrial plane on the septum. Both lower lateral cartilages were dissected free from dorsal and vestibular mucosal lining with minimal attachments of the pyriform ligament and the medial crural footplate with the depressor septi nasi muscle to maintain the original position. Moreover, the dermatocartilagenous ligament was isolated and preserved for fixation to the original position at the final procedure to prevent alar retraction postoperatively. These techniques make the lower lateral cartilage free of movement and allow shaping for any directions, such as projection or reduction, rotation or de-rotation, and tip lengthening or shortening without any restriction.
The asymmetric and deformed alar cartilage was reformed by minimal scoring incision (
Fig. 1B), and various suture techniques including medial crural spanning suture, dome spanning suture, lateral crural spanning or stealing suture, projection control suture, tip rotation suture, and cephalo-crural suture (
Fig. 1C) [
5].
Secondary operation
Because patients who underwent reoperation had undergone rhinoplasy more than once, unexpected problems may occur, such as grafting of the cartilage or implanted materials, and cutting or shredding of the alar cartilages. Foreign bodies and grafted materials were completely removed. The shredded alar cartilages were meticulously repaired to restore the original figure, and remodeling control was performed following the same procedures in addition to the control columella rigidity with two or three more medial crural spanning sutures for tripod support.
Another important procedure is the cephalo-crural suture for the tetrapod structural support, which should be a more stable and rigid structure in case of re-operation [
6].
Septoplasty was performed by multiple scoring incisions in a transverse or vertical fashion at the key stone area and midseptal segment for correction of high septal deviation and deviated bony septum with vomer. High deviation correction has dual effect for esthetic and functional improvement which are dorsal straightening and internal valve patency. The caudal septal deviation was corrected by cartilage scoring with the swinging-door procedure. The deviated caudal base of the nasal septum was fixed to the anterior nasal spine periosteum at the midmost position using monofilament 4-0 nylon by the figure-of-eight suture.
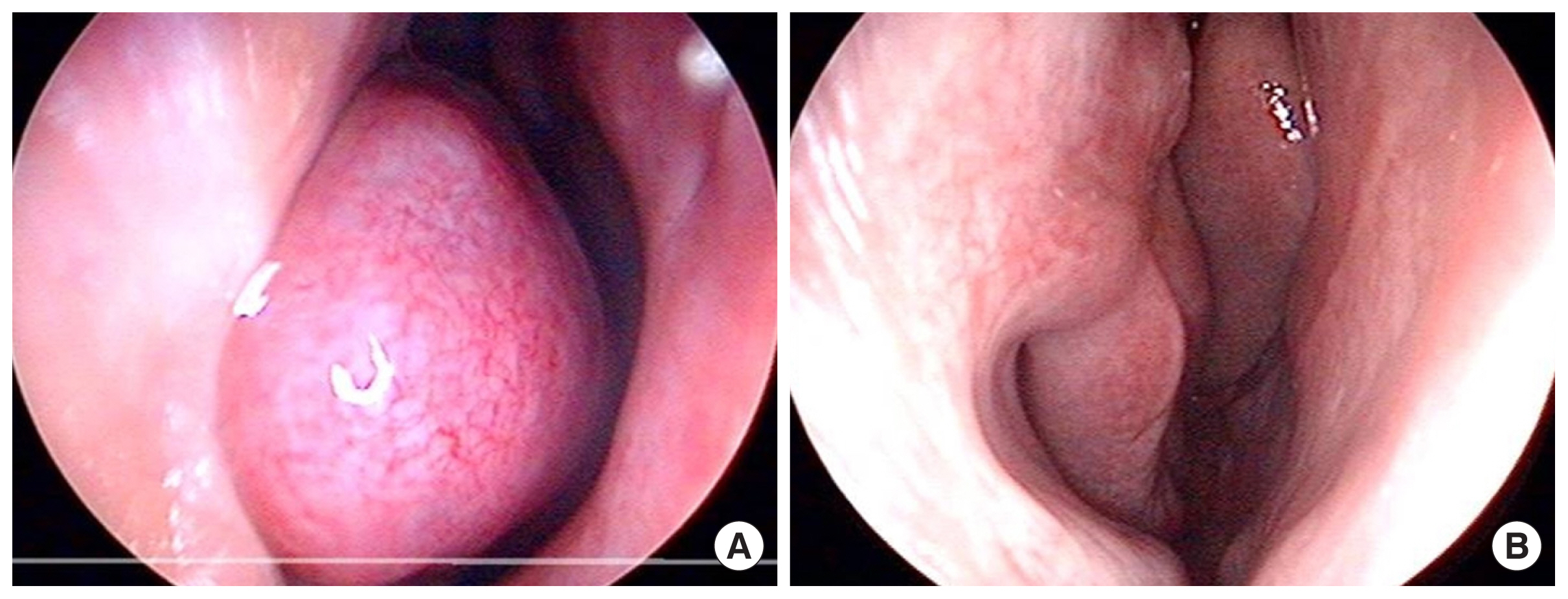
Meanwhile, the bulbous nose was debulked by trimming excessive scar tissue in the soft tissues envelope, partial de-fattening, and performing SMASectomy with special concern on vascularity. Coblator turbinoplasty (CelonLab ENT; Celon AG Medical Instruments, Germany) was performed under naso-endoscopy monitoring in case of turbinate hypertrophy. Finally, ancillary procedures for maintaining the symmetry of the nostrils and width of the nostril sill were controlled by excision and alar cinching sutures. The skin and subcutaneous layer were closed layer by layer after meticulous bleeding control. Compressive JosephŌĆÖs dressing was applied with appropriate nasal retainer, which should be kept over 4 months postoperatively to prevent nostril contraction or deformation. Nasal retainer keep the tenting effect of redraped vestibule to the remodeled lower lateral cartilage which improve the external valving action with enlarged nostril.
RESULTS
From 2005 to 2019, of the 150 patients who had secondary cleft lip nose deformities and visited our hospital for surgery, 85 (56.7%) were male and 65 (43.3%) were female, with a mean age of 30.2 years (range, 11ŌĆō63 years). Moreover, of these patients (n=150), 138 (92%) had undergone surgery, in which 30% (41/138) had surgery more than twice, and 6% (7/138) had it more than three times. Of the 138 patients who have undergone surgery, 51.2% (71 cases) used transplants, 57% (78 cases) used cartilage, fat, and AlloDerm graft, and 43% (59 cases) used silicone and Gore-Tex implant.
A questionnaire was sent to 150 patients who underwent surgery, 55 responded, and the contents of the questionnaire were analyzed. Of the respondents (n=55), 31 (56.4%) were male and 24 (43.6%) were female aged 11 to 69 years old by retrospective appraisal. No acute complications such as infection or wound dehiscence occurred (
Table 1).
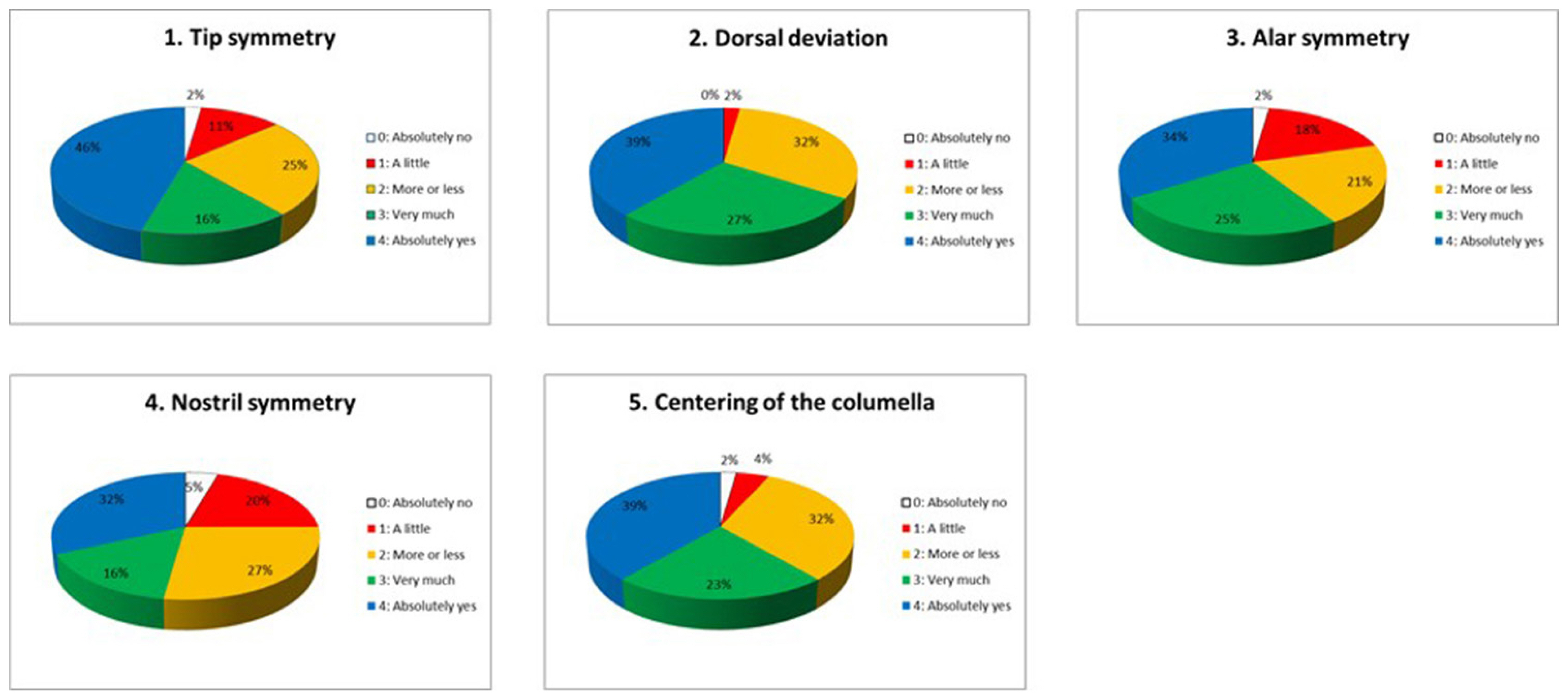
Surgical outcomes were evaluated with a questionnaire, which was divided into five categories each for esthetic and functional analyses (
Tables 2,
3). The satisfaction rate of each item was drawn in a pie chart.
As regards esthetics, the satisfaction rate ranged from 75 % to 98% (
Fig. 2). The worst satisfaction rate was based on the nostril symmetry at the wormŌĆÖs eye posture. This is the most significant complaint of patients with unilateral secondary cleft lip nose deformity. In the functional analysis, the satisfaction rate ranged from 78% to 98% (
Fig. 3). An unexpected and remarkable result was noted, i.e., improvement in smelling in approximately 81% of cases (very much, 42.5%; absolutely yes, 37.5%). It was one of the most positive sign reported by the patients regarding functional restoration with nasal breathing. A two-sided
t-test showed no significant differences (
p<0.05) in the functional results with septoplasty surgery (
Table 4).
The incisional scar was barely noticeable. Acute and chronic complications such as wound infection or wound dehiscence were rare. The overall satisfaction rate was relatively high in terms of functional and aesthetic results of the operation including shape and symmetry of the nose with long-term observation.
We present a case that was 17-year-old and underwent primary lip repair around age of 3 months, and had a nasal deformity, asymmetric nostril, and nasal obstruction. The patient underwent open rhinoplasty and septo-turbinoplasty described in the text for improvement of esthetic aspect and function rehabilitation. After 12 months of surgery, the patient showed satisfactory improvement both in external appearance and function (
Figs. 4,
5).
Herein, we present another impressive case on the life of a plastic surgeon, which we had over the 10-year cleft journey with the patient from teen age to early 30s. She did not know where and when she underwent primary repair for the cleft lip and palate. She was not concerned with the subsequent corrective surgery for cosmetic and functional growth. She had undergone six operations and had a 10-year orthodontic therapy with us. We talked several times not to dissuade her from total reconstruction. Finally, she expressed satisfaction of her external appearance and has a happy married (
Fig. 6).
DISCUSSION
The secondary cleft nose deformity has long been debated for the optimal timing of the procedure and the corrective technique [
7]. The lower lateral cartilage deformities including buckling, caudal tipping of the lateral crus, and short, contralateral rotation of the medial crura with septal deviation. Common nasal deformities include dorsal deviation, tip deflection, decrease in projection, alar buckling, and deviation of the columella and septum. Another causes are skeletal deficiency and the absence of nostril sill colliculus at the cleft side [
8].
There are need remodeling, reshaping and refining of nasal framework, soft tissue envelops and supporting structure. But there is rarely obtainable about an improvement absolutely perfection for esthetic and functional aspects.
Numerous methods were introduced for the repair of deformities, such as the two V-flaps [
9], reverse U-flap [
10], composite graft [
11ŌĆō
13], full-thickness skin graft [
14], V-Y composite flap [
15], and double composite tissue Z-plasty [
16]. More often, rib cartilage, conchal cartilage, and silicone implants are commonly used.
The goal of reconstruction should be to achieve acceptable cosmetic and functional results.
As early as 1984, McComb [
17] suggested that the lower lateral cartilages of the cleft side had near-normal size and strength, but merely deformed, displaced, and tethered by soft tissues. He also demonstrated that symmetric nostrils could be achieved with release and repositioning.
We would make an additional remark that it has sufficient strong rigidity, so cartilage remodeling is possible without any extra-support.
As development of autologous and non-autologous implants, including cartilage graft and silicone implants, some surgeons tend to rely on grafts rather than on restoring the normal shape and position of the lower lateral cartilage.
Authors apply three distinct opinions about the cartilage remodeling concept. First, the total size and stiffness of lower lateral cartilage is similar to the non-cleft side, except for deformation after puberty. Second, corrective effects cannot gain to pileup the graft materials or foreign bodies on the breaking tripod of the nasal tip. This will make only a bulbous nose without subtle contour of the nasal tip, alar fold, and nostril, as well as esthetic balance. Third, near-total mobilization, remodeling of both the lower lateral cartilage, and several suture techniques can allow rotation or de-rotation, lengthening or shortening, and projection or reduction for the collapsed nasal tip with sufficient redraping soft tissue envelop.
These are our basic concepts for corrective method without any transplantation. With this technique, one can restore near-normal and balanced nasal tripod, which maintains the symmetry of the nasal tip-defining points, shape of the nostrils, and alar contour without using cartilage grafts or foreign bodies. No single operation can completely fix all types of complex deformities in secondary cleft lip/nose deformity. Surgeons must know about various methods and apply the techniques in patient-tailored manner.
Lastly, we would like to mention our 40-year cleft journey with our patients. The doctor has to persuade the patient and the families for repeated timely operation to reach the final destination from birth to adulthood through sincerity, affection, and patience.
Many operative techniques are employed by different plastic surgeons for the repair of secondary cleft lip/nose deformities. However, the gold standard technique for primary or secondary repair has not been established. Most of them have been debated based on their advantages and disadvantages; thus no uniform operative method or satisfactory postoperative results were preferred by the patients and surgeons.
Herein, the presented technique is a fixed and constant maneuver in primary or secondary cases. However, the technique is laborious and time-consuming for meticulous cartilage isolation without cartilage damage and mucosal tearing.
This study has a couple of limitations. First, there was an insufficient long-term follow-up case. Second, statistical analyses could not be performed due to the small number of responses and showing at postoperatively. Third, we are very sorry for the lack of the photogrammetry or anthoropometry.
Despite these limitations, we analyzed the appropriateness of the surgical treatment for the patients. Therefore, this study makes a valuable contribution for the secondary cleft noses deformity patients that require reconstructive surgery. We would like to continue of follow-up and data collection forwardly. Based on our results, we strongly recommend the suture fixation technique for cleft lip/nose correction.