INTRODUCTION
Facial bone fracture patients suffer various symptoms. Symptoms such as pain, tenderness, and mouth-opening limitations improve soon after open reduction. However, facial sensory changes in areas innervated by the infraorbital nerve have prolonged recovery; these sensory changes include hypoesthesia, dysesthesia, paresthesia, and anesthesia of the upper lip, cheek, lower eyelid, and ala of the nose. The incidences of these symptoms are 30% to 80% of all zygomatic fractures and 31% to 50% of orbital floor fractures [
1â
9]. Infraorbital nerve originates from the maxillary nerve, a branch of the trigeminal nerve, that runs along the inferior orbital fissure to reach the orbital cavity, and then passes through the infraorbital canal to come out of the infraorbital foramen and reaches the face [
10]. Clinically, sensory changes after a mid-facial fracture are frequent; unlike bone union ending in 3 to 4 weeks, sensory changes last for up to a year, causing inconvenience to patients [
11]. There are several studies on infraorbital nerve disturbances associated with zygomaticomaxillary and orbital floor fractures. However, only a few of them compare the incidence of sensory changes between zygomaticomaxillary and orbital floor fractures. In this study, we compared the differences in sensory changes related to basic patient characteristics such as age, sex, and injury mechanism. In addition, we compared the sensory change and recovery of infraorbital area associated with zygomaticomaxillary and orbital floor fractures.
METHODS
We reviewed the computed tomography (CT) image data of patients diagnosed of zygomaticomaxillary or orbital floor fractures in a single center between January 2016 and January 2021. The patients diagnosed of zygomaticomaxillary or orbital floor fractures who did not present for follow-up in Wonju Severance Christian Hospital, patients younger than 18 years, patients whose sensory changes could not be evaluated (e.g., loss of consciousness), and patients with open fractures with mechanical infraorbital nerve transection were excluded from this study. Zygomaticomaxillary fractures of Knight and North classification type 2 are pure zygomatic arch fractures, and they were excluded from this study because they did present with sensory changes. A total of 652 patients with 430 zygomaticomaxillary fractures and 222 orbital floor fractures were evaluated retrospectively.
The evaluated variables were as follows: age, sex, hypertension, diabetes mellitus, injury mechanism, Knight and North classification (in zygomaticomaxillary fracture cases), injury indicated for surgery (in orbital floor cases), combined injury, sensory changes, and recovery period. The injury mechanisms were categorized as follows: traffic accidents, falls, motorcycle accidents, slips, assault, sports injuries, syncope, and others. The injury mechanisms were generally classified into the high-energy (traffic accident, fall-down injury, and motorcycle accident) and low-energy (slip-down injury, assault, sports injury, syncope, and others) groups [
12]. For orbital floor fractures, the indications for surgery were as follows: (1) limitation of eye movement with muscle incarceration; (2) fracture area of >1 cm
2 or >50% of the orbital floor; and (3) >2 mm of enophthalmos [
13]. All surgery was performed within 2 weeks of injury when the better outcomes and fewer postoperative complications were expected [
14].
The sensory changes were evaluated as two-point subjective infraorbital sensory changes and divided into hyperesthesia and hypoesthesia. Sensory change evaluation was conducted every 6 months until 24 months. A permanent sensory change, by definition, did not recover within 24 months. The 24 months follow-up permitted time for neural regeneration that may exceed 6 months postinjury [
15].
The chi-square test was used to compare the groups, and p-values of <0.05 denoted statistical significance. All data were analyzed with SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
DISCUSSION
Sensory changes are frequent sequelae of zygomaticomaxillary and orbital floor fractures, which may affect the infraorbital nerve. The infraorbital nerve is often involved in trauma at the site of the infraorbital fissure, canal, or foramen, such as zygomaticomaxillary and orbital floor fractures, and can be damaged by blunt trauma or bony compression at the fracture site. Sensory changes are more frequently associated with displaced than non-displaced fractures [
16], and the duration of recovery depend on several factors, including injury mechanism and method of treatment [
17,
18]. Therefore, physical examination at the time of injury and explaining the prognosis and course to the patient is important for the treatment of zygomaticomaxillary or orbital floor fractures. The authors investigated the prevalence and recovery of sensory changes associated with zygomaticomaxillary and orbital floor fractures and differences in the frequency and severity of sensory damage associated with pure orbital floor fractures, which have relatively minor damage, compared with zygomaticomaxillary fractures.
In this study, we reviewed the CT image data of patients diagnosed with zygomaticomaxillary or orbital floor fractures. CT is considered gold standard for evaluating fracture status and postoperative outcomes [
19]. There were differences between the baseline characteristics of the orbital floor and zygomaticomaxillary fracture groups. First, orbital floor fractures occurred at younger ages than zygomaticomaxillary fractures. Second, the mechanisms underlying the injuries associated with the two categories of fractures differed. The zygomaticomaxillary fracture group had more high-energy injuries (traffic accident, fall-down injury, motorcycle accident), and the orbital floor group had more low-energy injuries (slip, assault, sports injury, and syncope). Considering these two results, the average age of occurrence for orbital floor fractures (mean 41.6 years) was significantly lower than that for the zygomaticomaxillary fractures (mean 49.9 years). Orbital floor fractures are also more frequently associated with low-energy trauma (73%), such as assault and sports injury, which are assumed to be related to physical activity. Zygomaticomaxillary fractures are more frequently associated with high-energy injuries (44%), such as traffic accidents, motorcycle accidents, and falls, than orbital floor fractures (27%). Zygomaticomaxillary fractures are also more frequently accompanied by musculoskeletal injuries (17.9%) than orbital floor fractures (11.3%). Based on these results, we could conclude that zygomaticomaxillary fractures are more frequently high-energy fractures than orbital floor fractures. These findings are similar to those of a previous study, which reported that 1,142 patients with motor vehicle accidents, work-related injuries, fall-related injuries, and maxillofacial bone fractures have a higher prevalence of combined injuries [
20].
Montovani et al. [
21] reported in their study that zygomaticomaxillary fractures (76.8%) are more frequent in men than orbital floor fractures (23.2%). They attributed this to the predominance of males in driving, drinking alcohol, and sports, which are more associated with zygomaticomaxillary fracture-related injuries. However, our study showed no gender-related differences between the two types of fractures. We supposed that facial bone fractures were more frequent during the active ages and more active males.
A comparison of the sensory changes in the two groups showed no statistically significant difference in incidence. In planning this study, we expected the zygomaticomaxillary fracture group to have a higher incidence of sensory changes and a longer duration of recovery. However, the incidence of sensory changes was not significantly different in the orbital floor and zygomaticomaxillary fracture groups (16.2% vs. 15.2%,
p= 0.773). Zygomaticomaxillary fractures were associated with a higher incidence of hypoesthesia than orbital floor fractures, but the difference was not statistically significant (13.3% vs. 11.7%,
p=0.575). Sensory recovery was more rapid and better in the orbital floor fracture group than in the zygomaticomaxillary fracture group, but the difference was not statistically significant. Oh et al. [
22] revealed that sensory recovery associated with orbital floor fractures was more rapid than that associated with zygomaticomaxillary fractures in their study of 63 patients. Homer evaluated sensory recovery after orbital floor and zygomaticomaxillary fractures in 42 patients, and they also reported that infraorbital nerve dysfunction associated with zygomaticomaxillary fractures was associated with longer sensory recovery than that associated with orbital floor fractures [
5]. However, in this study of 652 patients, we could not find significant differences in the incidence and recovery of sensory changes after orbital floor and zygomaticomaxillary fractures. From this result, we concluded that the fracture type did not have a significant impact on the incidence and recovery of sensory changes.
Hilaire et al. [
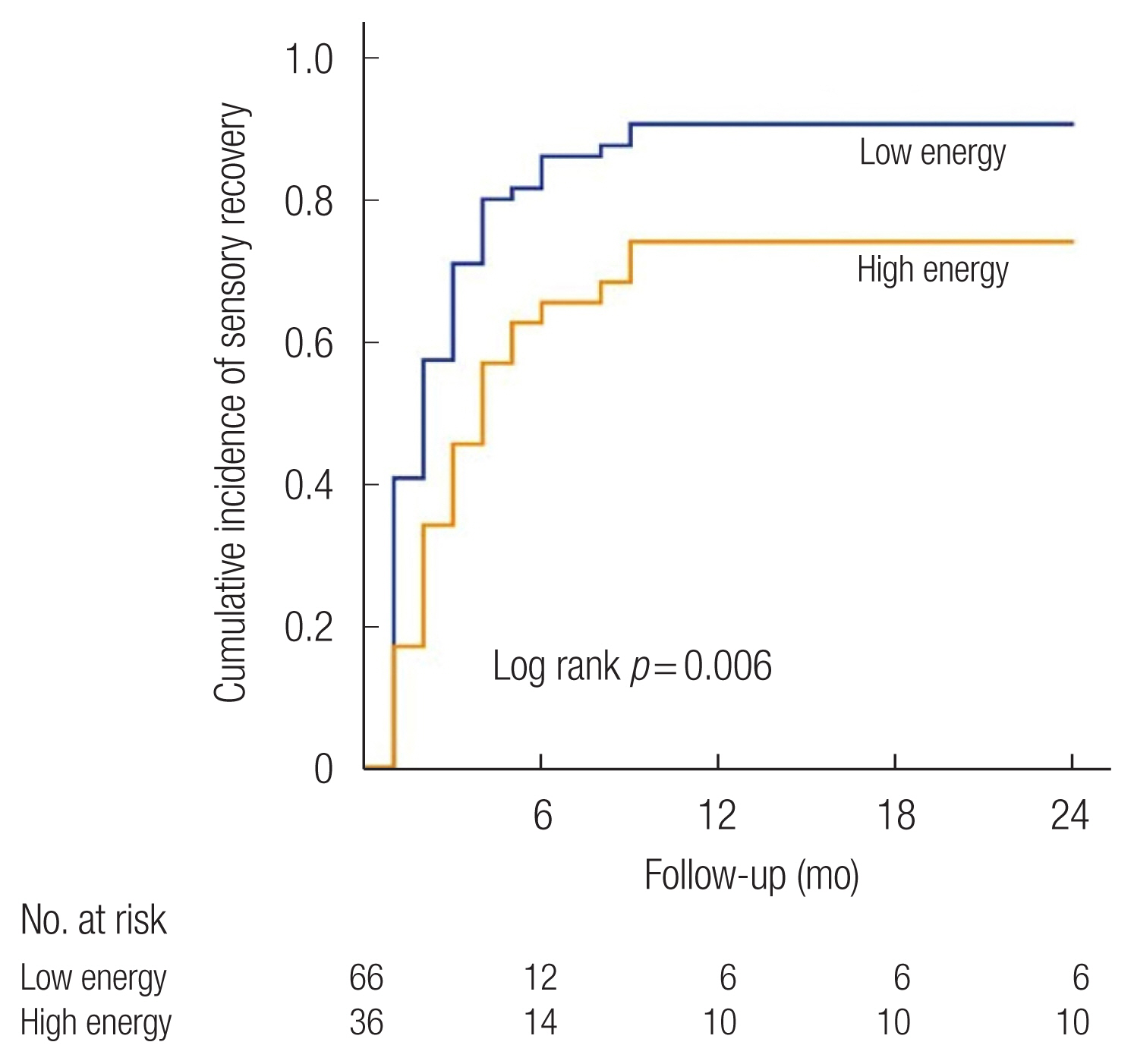
23] evaluated the distributions of bone fractures associated with high-energy and low-energy injuries across the upper, middle, and lower faces of 113 patients, and they found that mid-facial fractures were most prevalent. Other types of fractures such as LeFort and multiple facial fractures, were also found to be similar. In our study, the incidence of sensory changes was not significantly different in the low- and high-energy injury groups. However, permanent sensory changes were more incident in the high-energy injury group and the difference was significant (1.5% vs. 4.0%,
p=0.043).
As a result, this study indicated that there was no significant difference in the incidence of sensory changes and subsequent permanent sensory change in the patients with zygomaticomaxillary and orbital floor fractures. When the injury mechanism was considered, the prevalence of permanent sensory change increased in the high-energy injury group, which means that the intensity of damage can predict permanent sensory damage rather than the location of damage to the infraorbital nerve. Based on these results, we concluded that the mechanism of injury was associated with the incidence and prognosis of sensory changes than the classification of fractures, such as zygomaticomaxillary and orbital floor fractures. In addition, the risk of permanent sensory changes should be assessed based on the mechanisms of the fractures.
We evaluated the sensory changes based on the Knight and North classification in the zygomaticomaxillary fracture group because the classification is based on the rotation of the zygoma body. We supposed that nerve injury could change in the direction of rotation of the zygoma body with distraction or compression injury. However, this study showed no differences between sensory disturbance and recovery related to the classification. Oh et al. [
22] assumed in their study that the Knight and North classification was only based on the direction of rotation, it was not an indicator of the severity of a fracture, and it could not affect the sensory change incidence and recovery. We expected differences in the sensory disturbance depending on the direction of the rotation of the zygoma; however, based on our study results, we concluded that this classification had no significant effect on the incidence and recovery of infraorbital nerve disturbance.
For orbital floor fractures, injuries with indications for surgery were associated with a higher incidence of sensory changes and permanent sensory changes than those without indications of surgery. This is probably because more extensive fractures were associated with worse damage to the nerve. For patients with injuries with indications for surgery, it is necessary to assess for sensory changes before surgery and educate patients on prognosis.
In this study, the incidence of permanent sensory changes was similar to that reported in a previous study [
24]. Of the 652 patients in this study, 16 (2.45%) had sensory changes 24 months after the injury. All the patients who did not have sensory recovery until 12 months after trauma showed sensory disturbance within 24 months after injury. Based on this, we cautiously concluded that the patients who did not have recovery of the sensory changes until 12 months after trauma could not be expected to recover.
This study has several limitations. The study was retrospective in nature. In addition, evaluation of sensory change was subjective.
The strengths of this study are as follows. It was a comparative study with a larger sample than previous studies. In addition, the study compared the sensory changes based on age, sex, injury mechanism, and the type of fractures.
There was no significant difference in the incidence of sensory changes in patients with zygomaticomaxillary and orbital floor fractures. The orbital floor group demonstrated a shorter sensory recovery period and a lower incidence of permanent sensory changes than the zygomaticomaxillary fracture group, but there was no statistically significant difference. Therefore, in case of orbital floor fracture the risk of permanent sensory impairment should be considered, especially for cases with indications for surgery. Furthermore, since the mechanism of a fracture, rather than the type (orbital floor fracture and zygomaticomaxillary fracture), affects sensory changes and their prognosis, clinicians should pay attention to the risk of permanent sensory impairment associated with high-energy injuries.