Seroma prevention with topical Abnobaviscum sclerotherapy following excision of giant cervical lipoma
Article information
Abstract
Background
Lipomas are common benign tumors of mesenchymal origin that are composed of mature adipocytes. Giant lipomas have a diameter ≥10 cm in one or more dimensions or weigh at least 1,000 g. The surgical excision of a giant lipoma requires extensive dissection, increasing the risk of a seroma, which can cause surgical site complications such as wound infection and necrosis. Sclerotherapy with Abnobaviscum (Viscum album extract) is a relatively new technique used to reduce malignant pleural effusion. In this study, we evaluated the effectiveness of prophylactic sclerotherapy using Abnobaviscum to decrease seroma after giant lipoma excision.
Methods
We conducted a retrospective medical record review of patients who underwent surgical excision for giant lipoma of the neck from January 2019 to December 2022. Sclerotherapy was performed on the first postoperative day in patients who consented to the procedure, and Abnobaviscum was instilled through the existing Hemovac drain. We compared the clinical course between those who underwent postoperative sclerotherapy and those who did not.
Results
Among the 30 patients who underwent giant lipoma excision, we applied sclerotherapy with Abnobaviscum to 15 patients. The average time from surgery to Hemovac removal was statistically shorter in patients who underwent sclerotherapy (p=0.004). Furthermore, seroma formation was significantly reduced in patients receiving sclerotherapy (p=0.003).
Conclusion
In patients undergoing giant lipoma excision, sclerotherapy using Abnobaviscum helps reduce postoperative seroma formation during the initial postoperative period. It can be an excellent method to reduce complications related to seroma and attenuate patients’ postoperative burden.
INTRODUCTION
Lipomas are common benign tumors composed of mature adipose tissue. They can occur in almost any region of the body, but most are found in subcutaneous tissues [1]. Lipomas are called “giant” when they are ≥10 cm in diameter in one or more dimensions or weigh ≥1,000 g. The back is the most frequent site where giant lipomas occur, followed by the neck [2]. Surgical excision is the treatment of choice for lipoma, but complications such as pain, bleeding, infection, seroma, and recurrence are common [1]. Furthermore, seroma commonly occurs when a giant lipoma is removed from the neck [3].
Seroma refers to an accumulation of serous fluid within the dead space left by an excision. Seromas can be reabsorbed spontaneously when pressure is applied at the surgical site, but sometimes require repeated aspirations. Unabsorbed seromas can cause surgical site dehiscence, infection, and necrosis. It is difficult to prevent seroma formation, and treatment is challenging. Complete surgical resection is required when a seroma becomes chronic and forms a pseudocapsule. Seromas can be reduced using several methods, including closed suction drainage, quilted or progressive-tension suturing, corticosteroid injection, aspiration, sclerotherapy, compressive dressing, and surgical resection [4–7].
Sclerotherapy has an inflammatory and subsequently sclerosing effect on serous membranes and has been used to obliterate pleural surfaces to eliminate persistent pleural effusions. There are numerous sclerosing agents including fibrin glue, doxycycline, tetracycline, OK432, bleomycin, autologous blood, and talc [8,9]. Sclerotherapy using Abnobaviscum (Viscum album or mistletoe extract) has been identified as an effective method with acceptable side effects when treating malignant pleural effusion and seromas in flap donor sites [9,10]. Furthermore, several studies have demonstrated effective prophylaxis and treatment of seromas following pressure ulcer reconstruction [11].
In this study, we investigated the efficacy of prophylactic sclerotherapy using Abnobaviscum to decrease seroma in patients undergoing giant lipoma excision.
METHODS
Study design and patients
We retrospectively reviewed patients who underwent excision of giant lipomas in the neck at our hospital between 2018 and 2021. If the preoperative enhanced computed tomography result or the postoperative specimen size was ≥10 cm in one or more dimensions, or the specimen weighed ≥1,000 g, a lipoma was determined to be giant and included in the study. It was explained to all study participants that the goal of sclerotherapy was to decrease possible seroma after surgery for giant lipoma. The patients were divided into two groups. The first group consisted of patients who underwent sclerotherapy using Abnobaviscum to decrease seroma after the removal of a large lipoma. The second group consisted of patients who underwent the removal of a giant lipoma without sclerotherapy. Medical records were used to review patient information including: age, sex, body mass index (BMI), diagnoses of hypertension (HTN) or diabetes mellitus (DM), smoking status, treatment with an anticoagulant agent; location, size, weight, and duration of the lipoma; and clinical course, including the Hemovac drainage amount, time of Hemovac removal, and wound complications.
Surgical method and postoperative care
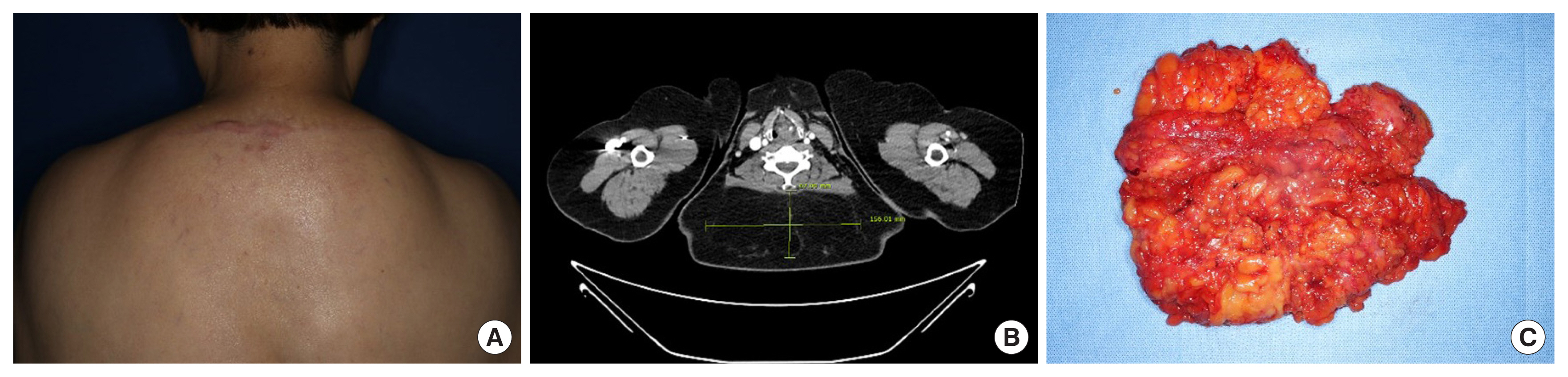
The same surgical excision method was used in all patients under general anesthesia (Fig. 1). After surgical excision, quilted or progressive-tension suturing was performed to reduce the dead space. In addition, closed suction drainage (Hemovac) was introduced to remove fluid accumulation in the operation site bed. Any fluid collection was aspirated and removed daily through the Hemovac line, and the amount was recorded. Daily compressive dressings using fluffy gauze and elastic bandage were applied, and surgical-site immobilization was recommended after surgery. All patients were hospitalized until the Hemovac was removed, and none were discharged with an inserted Hemovac.
Sclerotherapy
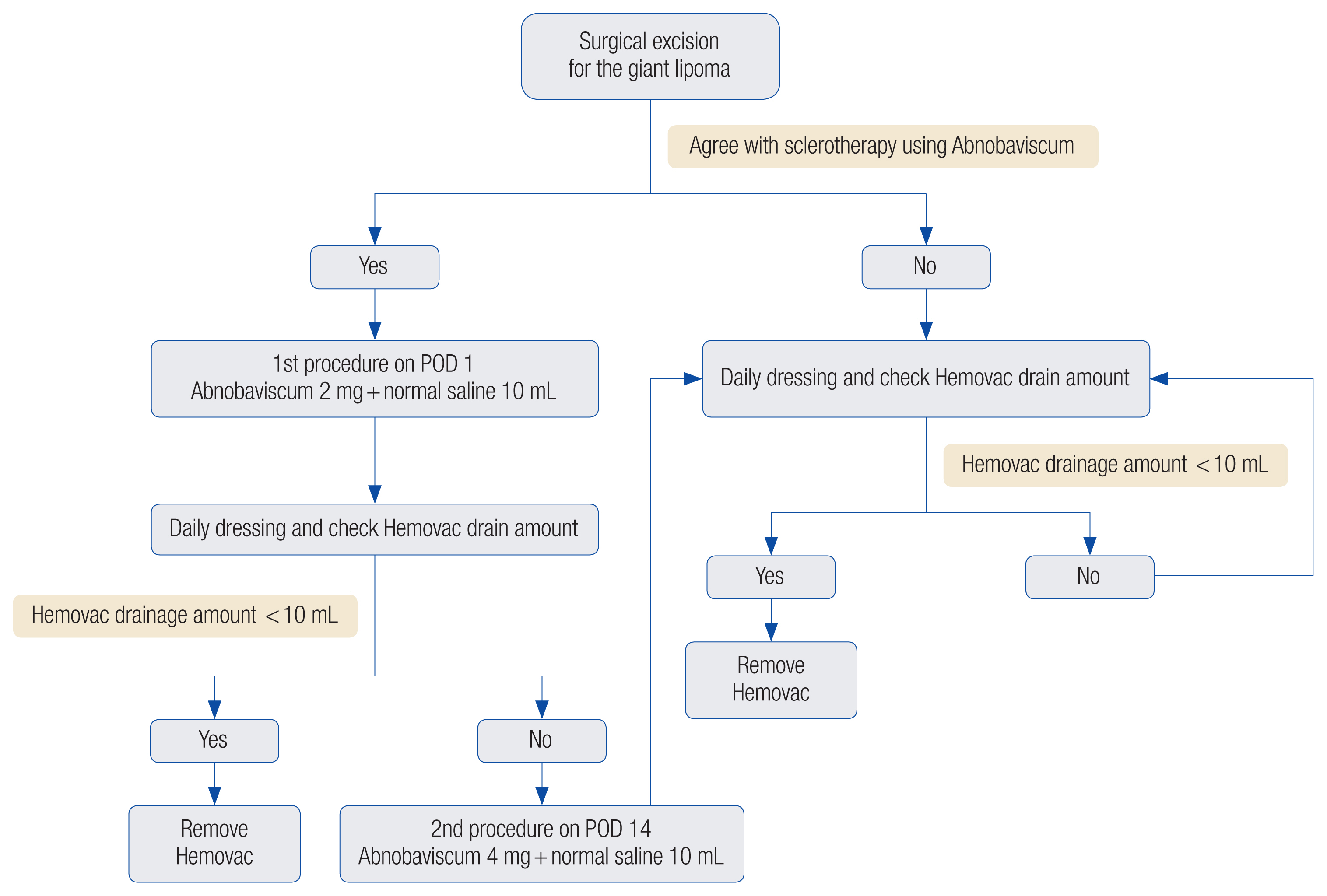
All patients who agreed to undergo sclerotherapy using Abnobaviscum (Abnoba Heilmittel GmbH) to decrease seroma were provided a thorough explanation of the procedure. Informed consent was also obtained for undergoing sclerotherapy including the efficacy and possible side effects of the Abnobaviscum agents, such as local pain, local febrile sense, and in rare cases, diarrhea and urinary frequency. The protocol of sclerotherapy using Abnobaviscum is shown in Table 1. Considering that the lipoma lesions in our study were smaller than the treatment sites of previous reports, which involved the entire pleural area of patients with malignant pleural effusion, a lower dose was used (Table 1) [10–12]. In the first procedure (postoperative day [POD] 1), 2 mg of Abnobaviscum was mixed with 10 mL of normal saline. If a second procedure was necessary (POD 14), 4 mg of Abnobaviscum was mixed with 10 mL of normal saline (Fig. 2).
On POD 1, all fluid that had drained into the closed wound drainage system (Hemovac) was removed and the amount was measured. Then, the mixture of Abnobaviscum and normal saline was injected through the Hemovac line. The clamp was locked to prevent backflow and placed higher than the Hemovac insertion site. After injection, the patient was asked to maintain prone, decubitus right, and decubitus left positions for 10 minutes each. After 30 minutes, the clamp was unlocked, and the injected fluid was removed by aspiration through the Hemovac line. For all patients, fluid buildup was removed through continuous Hemovac suction. The Hemovac was removed when the daily amount of fluid drainage was <10 mL and a physical examination found no evidence of fluctuant fluid retention.
Definition of seroma formation
Physical examinations and sonography were performed at 2 and 4 weeks postoperatively to check for the occurrence of seroma. Additionally, the presence of seroma was defined as the inability to remove the Hemovac due to continuous fluid accumulation despite complete healing of the wound at the surgical site.
Statistical analysis
Continuous variables were presented as means with standard deviation. Frequencies and percentages were calculated for categorical variables. For a comparative analysis of the two groups, the independent sample t-test and the Mann-Whitney U-test were used for continuous variables and the Fisher exact test was used for categorical variables. The Spearman correlation was used to estimate the degree of association between variables. All p-values <0.05 were considered statistically significant. Statistical analyses were performed using SPSS version 27.0 (IBM Corp.).
RESULTS
Patient demographics
The 30 patients were divided into two groups, and their demographic data were analyzed (Table 2). Group A included 15 patients who underwent sclerotherapy with Abnobaviscum after lipoma excision, and the 15 patients in group B did not receive sclerotherapy. The average age of the patients was 61.8±11.1 years in group A and 59.9±14.0 years in group B, showing no statistical difference between groups (p=0.819). In group A, there were nine men (60.0%) and six women (40.0%), and in group B there were 10 men (66.7%) and five women (33.3%); groups A and B did not show a statistically significant difference in the sex distribution (p=1.000). The BMI in group A (30.4±5.6 kg/m2) was not significantly different from the BMI in group B (28.1±4.3 kg/m2) (p=0.215). Patient histories of HTN, DM, smoking, or treatment with anticoagulant agents were also not significantly different between groups A and B.
Lipoma characteristics
The characteristics of the lipomas in the two groups were compared (Table 3). The lipoma was located in the anterior neck in two patients (13.3%) and in the posterior neck in 13 patients (86.7%) in both groups A and B, which was not a statistically significant difference (p=1.000). To compare lipoma size, the diameter at the largest dimension of each lipoma was selected and was 11.9±2.1 cm in group A and 12.3±2.1 cm in group B, showing no statistical difference (p=0.307). There was no significant difference in the weight of the lipomas between the two groups (p=0.756). The duration of illness was 8.8±6.2 days in group A, which was longer than the duration of 5.7±7.2 days in group B (p=0.020).
Comparison of the clinical course
The clinical course of the patients in the two groups was compared to evaluate the efficacy of sclerotherapy (Table 4). Quade nonparametric analysis of covariance was performed to compare the two groups with adjustment for covariates, including the duration of illness. The average postoperative Hemovac removal time was 7.8±8.3 days in group A and 13.4±5.5 days in group B—that is, on average, Hemovac removal took place 5.6 days earlier in group A (p=0.004). The ratio of Hemovac drainage amounts on POD 2 to POD 1 was 0.30±0.18 in group A and 0.88±0.55 in group B, showing a significantly greater decrease on POD 2 in group A (p=0.000). The occurrence of seroma differed significantly between the groups: two (13.3%) in group A and 10 (66.7%) in group B (p=0.003). The rate of wound complications, such as wound infection, dehiscence, and necrosis showed no difference between the groups (p= 1.000). Furthermore, there were no statistically significant correlations between the development of seroma and patient information (age, sex, BMI, HTN, DM, smoking, or anticoagulant agent use) or and lipoma characteristics (size, weight, or duration). Two of the patients who underwent sclerotherapy complained of localized heat sensations and pain, but these resolved with oral medication such as nonsteroidal anti-inflammatory drugs (NSAIDs).
DISCUSSION
Lipomas are common benign mesenchymal tumors, primarily found in soft tissues and composed of adipose tissue. They can occur subcutaneously in any fat-containing region of the body. The neck and trunk are the most common locations of lipomas [13–15]. Surgical excision is the treatment of choice for large lipomas, but complications such as pain, bleeding, infection, hematoma, seroma, scarring, and recurrence can occur. Seromas are not unusual following surgery for soft tissue tumors, and giant lipomas have a high probability of seroma formation due to the extensive dissection required to remove them [2,3].
Seromas are serous fluid collections, a common complication of surgical procedures that create an anatomical dead space. They are absorbed naturally in most cases, but if not, sequelae such as surgical wound infection, dehiscence, and necrosis may occur. Various methods exist to decrease seroma, including repeated aspiration, closed suction drainage, quilted or progressive-tension suturing, corticosteroid injection, immobilization, sclerotherapy, compression using a garment or dressing, and surgical resection. Seroma formation is difficult to prevent, but once it occurs, a seroma is also difficult to treat [4–7]. If not properly treated, fibrous pseudocapsules develop surrounding the seroma, leading to a chronic encapsulated condition. Seroma pseudocapsules consist of fibrous tissue composed of the eosinophilic hyaline degeneration of collagen and the products of inflammatory and lymphocytic infiltration. In these cases, complete surgical capsulectomy is required [4,16]. According to Nichter et al. [8], even if a seroma is eventually treated using time-honored methods, the extended use of a drainage catheter, increased risk of infection, prolonged hospitalization, and frustration for patients and surgeons are unavoidable.
Sclerotherapy creates a fibrotic change when an irritating material is injected into the seroma, causing adherence of the inner serous surfaces and removal of dead space. This inflammatory reaction exerts a subsequent sclerosing effect on the serous membranes. Sclerotherapy has been used to obliterate visceral and parietal pleural surfaces and eliminate persistent pleural effusions. There are numerous chemical sclerosing agents, including fibrin glue, doxycycline, tetracycline, OK432, bleomycin, autologous blood, and talc [8,9]. Currently, Abnobaviscum, a Viscum album (European mistletoe) extract, is widely used in sclerotherapy. Several studies have shown that it has advantageous therapeutic effects and few adverse effects compared to other sclerosing agents [9]. It has been used for malignant pleural effusion, the treatment of surgical flap donor-site seroma, and seroma treatment and prevention after pressure ulcer reconstruction. Abnobaviscum degrades ribosomal RNA, blocks protein synthesis, and induces cell death, leading to an antitumor effect. It also promotes the synthesis of macrophage colony-stimulating factors and removes dead space through an immune response that increases interferon, interleukin, tumor necrosis factor, and natural killer cell concentrations. Sclerotherapy using Abnobaviscum has been reported to cause mild adverse effects, such as a local sensation of heat, local pain, and in rare cases, diarrhea and urinary frequency; these adverse effects tend to resolve rapidly [9–11]. Considering this, we performed sclerotherapy using Abnobaviscum to decrease seroma formation, which was highly likely to occur after the removal of a giant lipoma.
Our study found a significant difference in patients’ clinical courses depending on whether sclerotherapy was used. Specifically, we compared the clinical course of two groups of patients undergoing giant lipoma excision in the neck, followed by the removal of serous fluid using a Hemovac drainage system. Postoperative Hemovac treatment was maintained for an average of 7.8±8.3 days in group A and 13.4±5.5 days in group B, and then the Hemovac was removed. The time interval was significantly shorter in group A (p=0.004). Seroma formation occurred in significantly fewer patients in group A than in group B (13.3% vs. 66.7%, p=0.003). Using sclerotherapy with Abnobaviscum decreased complications caused by seroma and shortened the treatment period, thereby reducing the hospitalization period and burden for patients and accelerating their return to daily life. In addition, to evaluate the immediate effect of sclerotherapy, the Hemovac drainage amount on POD 2 (the day after sclerotherapy) was compared with the Hemovac drainage amount on POD 1. The ratio of the drainage amount on POD 2 compared to POD 1 was 0.30±0.18 in group A and 0.88±0.55 in group B (p=0.000). Therefore, we confirmed that fluid accumulation in the dead space was significantly reduced immediately after sclerotherapy. Although localized heat and pain occurred in two out of 15 patients who underwent sclerotherapy, these symptoms resolved without recurrence after a one-time dose of an oral medication such as NSAIDs. There were no other adverse effects such as diarrhea or urinary frequency.
This study had some limitations. The statistical analysis comparing the Hemovac removal time between the two groups used a nonparametric statistical method because the sample size of this study was small. For this reason, the dispersion of data within each group (i.e., standard deviation) was not very meaningful. To address this problem, it is necessary to conduct a more reliable analysis in a larger group. According to Sanchez et al. [17], giant lipoma is defined as a lesion that is at least 10 cm in diameter in one dimension or weighs a minimum of 1,000 g. All patients in this study had lipomas larger than 10 cm in diameter, but none of the lipomas exceeded 1,000 g in weight. According to Aho et al. [18], the correlations between seroma formation and risk factors such as DM, obesity, HTN, and smoking are still unclear due to inconsistent study results. In our study, there were no statistically significant correlations between seroma formation and various patient demographics (age, sex, BMI, HTN, DM, smoking, and anticoagulant agent use) or the duration of lipoma. Specifically, the lipoma characteristics, including the weight of lipoma and the diameter of the largest dimension, which could represent the size of the mass, showed no statistically significant correlations with seroma formation. Otherwise, the patient who had the most prolonged Hemovac duration belonged to group A, which received sclerotherapy with Abnobaviscum. A 61-year-old woman underwent elliptical excision for a non-capsulated giant lipoma measuring 10.8×3.9×5.6 cm in the subcutaneous layer of the posterior neck. She underwent sclerotherapy on POD 1. The Hemovac drain amount decreased from 120 mL on POD 1 to 30 mL on POD 2. However, due to continued fluid accumulation, a second injection of Abnobaviscum was instilled on POD 14, increasing the dose to 4 mg. Nonetheless, serous discharge continued. Therefore, the Hemovac line was exchanged on POD 30 and the Hemovac could be removed 4 days later on POD 34. No seroma findings were noted in a follow-up performed 1 month later (Fig. 3). In addition, our study was a retrospective study based on medical records and lacked long-term imaging follow-up. A large prospective double-blind study should be conducted to confirm our findings.

(A) Preoperative sonography of a 61-year-old woman who underwent excision of a posterior neck lipoma. (B) Postoperative sonography after Hemovac removal. (C) Clinical course of Hemovac drainage amounts.
In conclusion, sclerotherapy using Abnobaviscum in the initial postoperative period in patients who have undergone giant lipoma excision in the neck can accelerate Hemovac drain removal and decrease seroma formation. Thus, it can reduce the risk of seroma-related complications such as surgical site infection, dehiscence, and necrosis and attenuate the burden for patients and surgeons by shortening the treatment period. Although the prevention and treatment of seroma are still challenging, sclerotherapy using Abnobaviscum can be an excellent prophylactic technique to decrease seroma after surgical procedures with a high possibility of seroma formation.
Notes
Conflict of interest
Jae Ha Hwang and Kwang Seog Kim are editorial board members of the journal but were not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Funding
None.
Ethical approval
The study was approved by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUH-2023-018) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and use of their images.
Author contributions
Conceptualization: Jae Ha Hwang. Data curation: Jun Ho Choi, Seung Yeon Choi. Formal analysis: Kwang Seog Kim, Sam Yong Lee. Investigation: Jun Ho Choi, Seung Yeon Choi. Methodology: Kwang Seog Kim, Sam Yong Lee. Project administration: Jae Ha Hwang. Writing - original draft: Jae Ha Hwang, Jun Ho Choi, Seung Yeon Choi. Writing - review and editing: Jae Ha Hwang.
Abbreviations
BMI
body mass index
DM
diabetes mellitus
HTN
hypertension
NSAIDs
nonsteroidal anti-inflammatory drugs
POD
postoperative day