INTRODUCTION
Zygomatic arch fractures are a common injury to the face, with isolated arch fractures making up 10% of all zygoma fractures and 5% of all facial bone fractures [
1]. The zygomatic arch is the lateral prominence of the cheek and plays a role in mouth opening and mastication. It also provides an origin for the masseter muscle on its lower border and protects the temporalis muscle, which is inserted onto the coronoid process of the mandible [
2].
Isolated zygomatic arch fractures are typically repaired through closed reduction, either through the temporal or intraoral approach, when they cause difficulty in mouth opening or deform the contour [
3]. However, the surgical outcomes of closed reduction for these fractures can often be poor due to the difficulty of accurately determining the location of maximal medial displacement of the fracture due to swelling around the site.
Therefore, we conducted this study to investigate tendencies in the discrepancy between the locations of the depression on the soft tissue and bone. On that basis, we sought to identify how to determine the actual location of maximal medial displacement of the fracture in the patientŌĆÖs face using a computed tomography (CT) scan convertible from a 3-dimensional (3D) bone image to a 3D soft tissue image.
METHODS
We conducted a retrospective review of a series of patients with isolated zygomatic arch fractures corresponding to type V in the Nam and Jung classification [
4] between March 2012 and February 2022. In order to evaluate whether there was a discrepancy in the gap between the most depressed location on the preauricular area (judged at the point where reduction would be done based on a photograph) and the location of maximal medial displacement of the fracture on the bone in CT images, we established a reference point (RP) for consistent measurements, and from that point, measured the transverse and vertical distances both on photographs and on the bone images of 3D CT, respectively. The values of distance measured on the photographs were corrected using the ratio of the side ear length between the photograph and the soft tissue image of 3D CT. All CT images in this study were taken from the same PACS viewer (INFINITT PACS Version 3.0.11.3 BN105; INFINITT Healthcare).
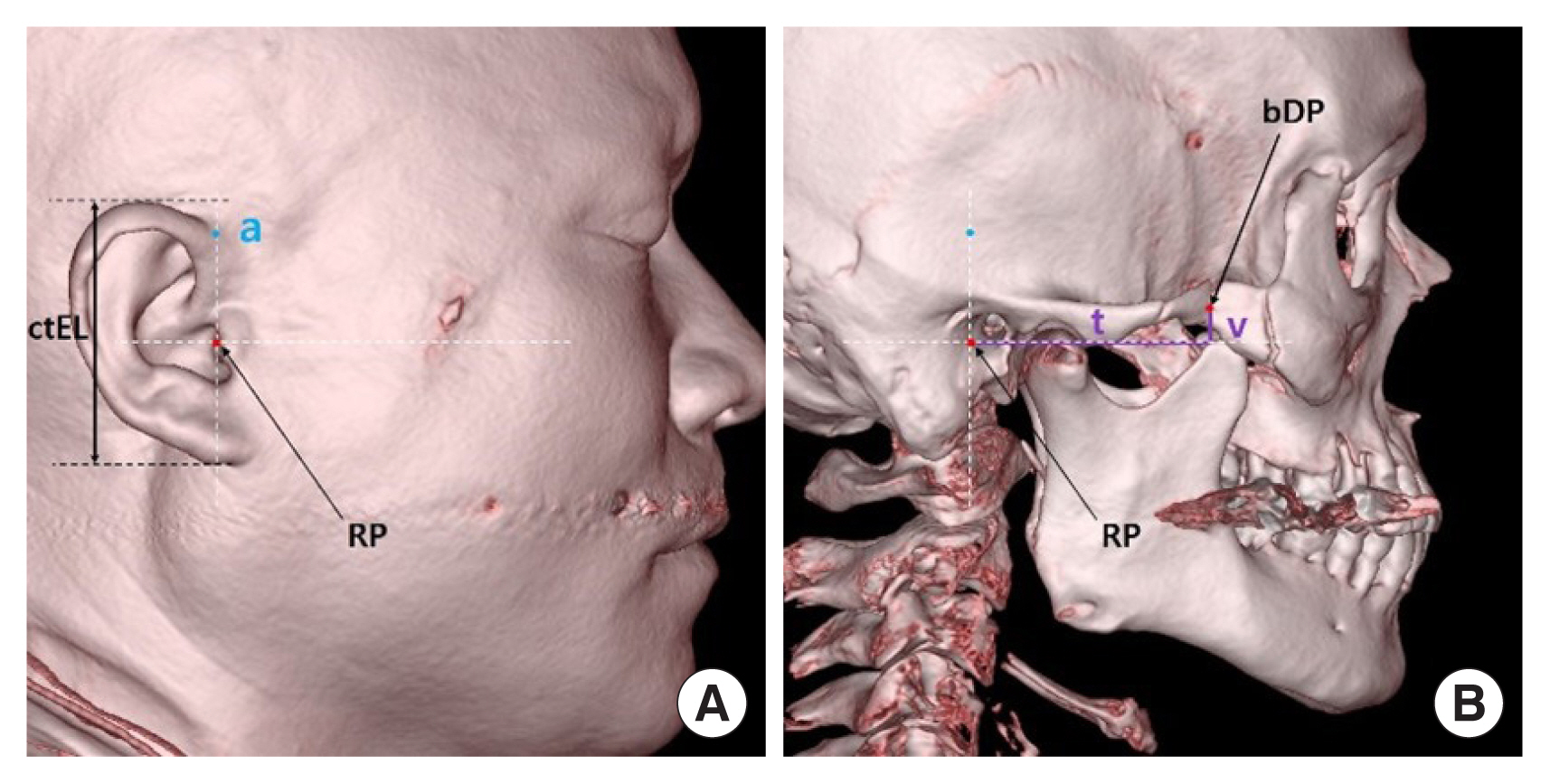
To establish the RP, we first drew a vertical line passing through the end point of the root of the ear helix in the patientŌĆÖs side-view photograph, as well as a transverse line passing through the longest horizontal axis of the external meatus opening. We then used the point where the two lines intersected as the RP for measurement. Next, we measured the ear length (pEL), the transverse distance (T), and the vertical distance (V) from the RP to the most depressed location of the soft tissue (pDP) along the preauricular area on a side-view photograph (
Fig. 1).
Subsequently, we measured the ear length (ctEL) and pointed out the RP on the 3D soft tissue images in the same way, and after converting the soft tissue image into a bone image on the same screenshot of the CT scan, we measured the transverse distance (t) and vertical distance (v) from the RP to the actual inward portion of the fracture of the zygomatic arch (bDP) using the ruler tool on the CT imaging program (PACS version 3.0.11.3 BN105; INFINITT Healthcare) (
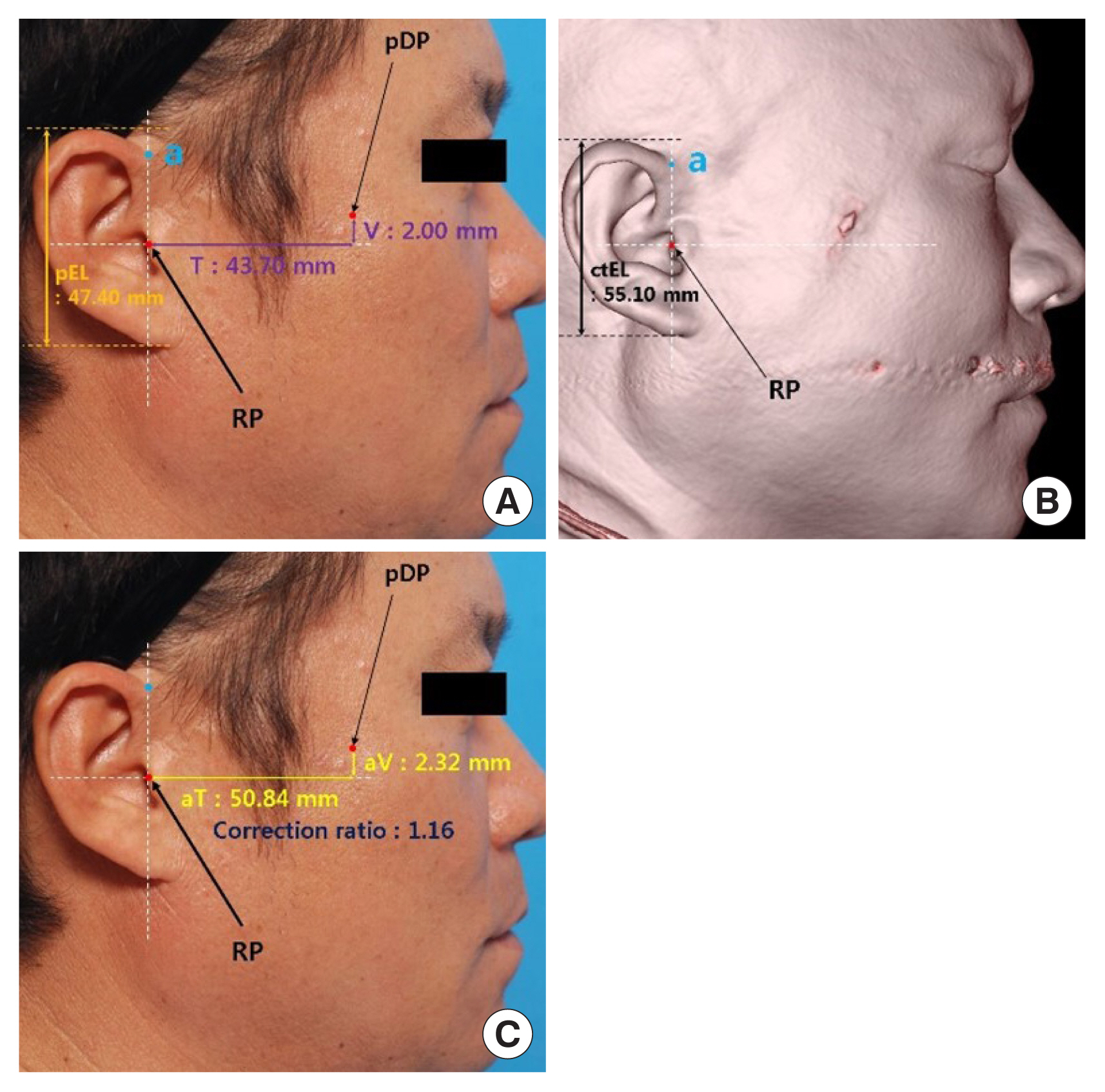
Fig. 2). The values of distance (V, T) measured from the photo were corrected into actual lengths (aT, aV) for each patient, using the ratio of the side ear length between the photo and 3D soft tissue image.
For example, if the ear length (pEL) on a photograph was 47.40 mm and the ear length (ctEL) on the 3D CT soft tissue image was 55.10 mm, the correction ratio would be 1.16. Then, if the measured values of the transverse distance (T), and the vertical distance (V) from the RP to the most depressed location of soft tissue (pDP) on the photograph were 43.70 and 2.00 mm, respectively, the actual length of T (aT) and V (aV) would be corrected to 50.84 and 2.32 mm, respectively (
Fig. 3).
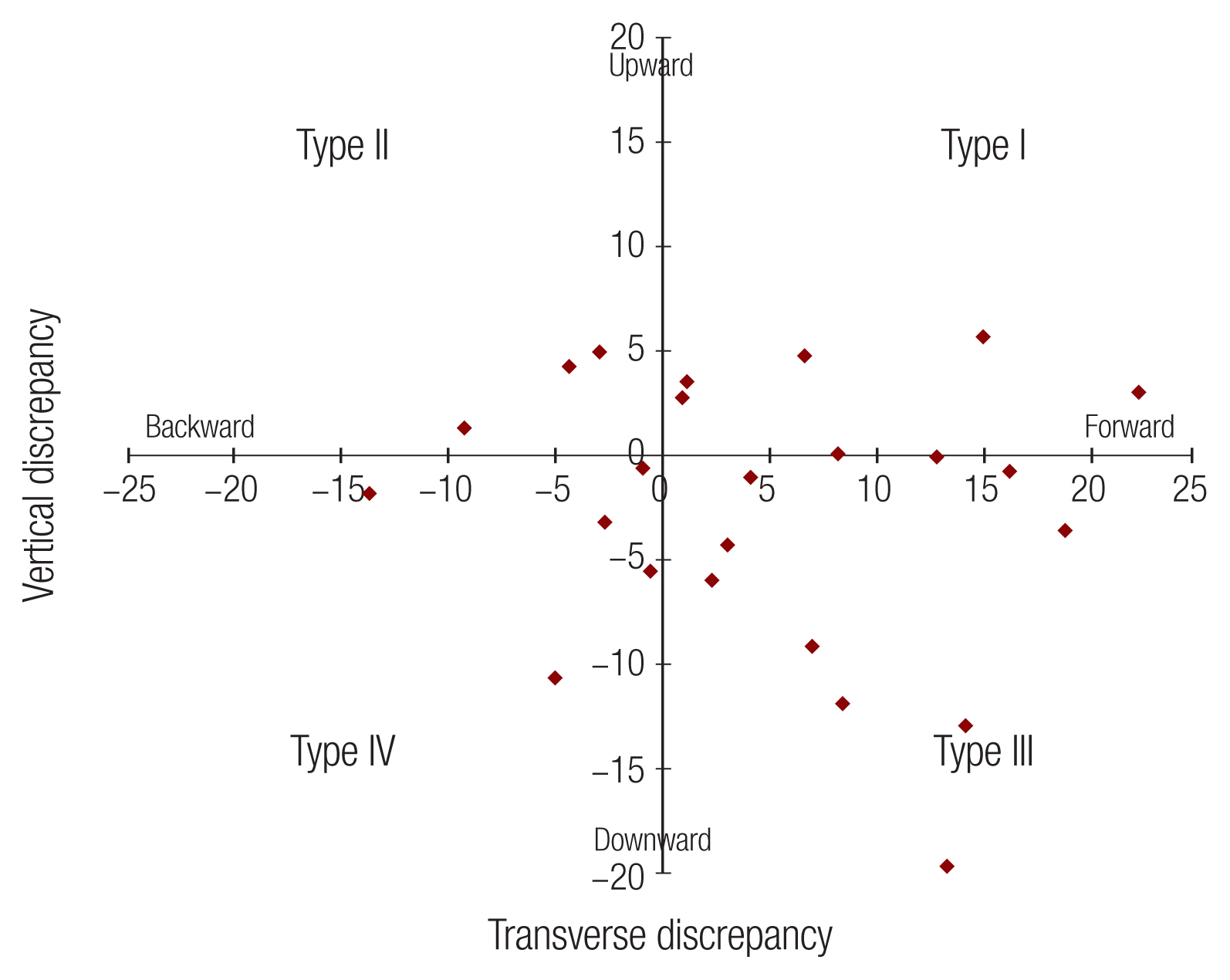
Finally, we compared the distance between the location on the lateral cheek skin (pDP) and bone (bDP) using the values of transverse distance (aT, t) and vertical distance (aV, v) from the RP. This allowed us to estimate the degree of the discrepancy (
Fig. 4).
DISCUSSION
When difficulty of mouth opening or contour deformity is present, almost all simple zygomatic arch fractures are treated with closed reduction using a Dingman elevator through the temporal (GilliesŌĆÖ technique) or intraoral (KeenŌĆÖs technique) approach, except in cases of unstable or complicated arch fractures [
3,
5,
6].
While the closed reduction method is relatively simple, it can be challenging to confirm the exact fracture location due to swelling of the soft tissue and muscles that can mask the inward portion of the fracture. This can lead to incomplete under-correction or unstable over-correction, resulting in asymmetric contour deformities or persistent functional deficits in mouth opening.
To address these issues, various methods have been introduced to confirm the exact inward fracture location and extent of reduction of the arch. Westendorff et al. [
7] introduced the use of CT-based surgical navigation to compare the real and virtual bone positions, and other authors have demonstrated that using a C-arm or a mobile Fluoroscan can increase the accuracy of closed reduction by confirming the exact inward fracture location during surgery, although the issue of radiation exposure remains [
8ŌĆō
11].
Other reports have shown that ultrasound is useful for diagnosing and managing zygomatic arch fractures, with a sensitivity of 88.2% and specificity of 100% in accurately assessing inward fracture sites of the arch [
12], and have reported successful results for the closed reduction of zygomatic arch fractures using ultrasound and needle marking [
13]. Therefore, as many authors have previously pointed out, it is important to not only assess the exact inward fracture location, but also to aim for precise reduction in order to achieve successful outcomes with anatomic reduction through closed reduction in even simple zygomatic arch fractures.
In general, closed reduction for simple zygomatic arch fractures is achieved by applying the opposite force of the injury vector to the indented area of the lateral cheek that is believed to be inwardly fractured, based on palpation and visual inspection. If the surgical result is poor despite appropriate reduction, it is possible that the vector of reduction was misrepresented or the wrong portion was reduced, rather than the actually depressed portion of the bone. However, due to the varying swelling of the soft tissue and muscles in each patient, it can be difficult to detect the exact location of reduction around the fracture site with visual inspection alone.
Meanwhile, Nam and Jung analyzed the main classification criteria for isolated zygomatic arch fractures (injury vector, V-shaped fracture, coronoid collision) from five previous studies, and presented a modified classification into six types by subdividing zygomatic arch fractures. In this study, in order to target fractures with an apparently clearer indentation portion on the lateral cheek skin, only patients with isolated zygomatic arch fractures corresponding to type V (i.e., a V-shaped fracture with depression of the middle portion and bone displacement with fracture lines or greenstick fractures due to injury, with the force vector directed toward the middle portion with or without coronoid impingement) in the Nam and Jung classification were included.
To detect the real inward fracture site of the zygomatic arch on the skin of the lateral cheek, we evaluated the agreement between the location of depression on the lateral cheek judged to be reduced and the actual inward location of the bone in the real fracture site using the soft tissue images on the 3D reconstruction format and the 3D bone images, which were converted on the same screen image of the CT scans. We compared these with the distance and location on photographs as described above. While it is easier to measure the distance using soft tissue images on the 3D reconstruction and bone images on CT scans taken immediately after the trauma, the measurement of the distance on the lateral cheek was made using patientsŌĆÖ photographs taken 1 day before the operation to minimize error caused by swelling.
Since, as found in this study, the transverse and vertical distances between the soft tissue and the bone depression differed in all cases, and these differences showed four types (forward and upward, backward and upward, forward and downward, and backward and downward), it is necessary to more accurately detect the location of the actual inward portion of the fracture of zygomatic arch fractures, even though the most common pattern of discrepancy was directed forward and downward, albeit without a meaningful tendency.
Therefore, to help accurately position the Dingman elevator in the actual inward fracture location, an RP in the 3D soft image was determined, and that image was converted to a 3D bone image to check the distance (t and v) from the same RP to the most inwardly depressed fracture location. We suggest that better surgical results could be achieved by inserting a Dingman elevator at the point identified by feeling with oneŌĆÖs fingertips to identify the most depressed location, taking the same RP on the patientŌĆÖs face, and marking a point at the location of the t and v distance.
A limitation of this study is that the identification of the most depressed portion visually on the photographs and the location of the innermost displaced fracture on the 3D reconstructed bone images is subjective. To minimize this error, three plastic surgeons independently marked the most depressed portion both on the photographs and CT images, and the mean values of distance from the RP were used in this study.
Another limitation is that each patient had a different angle in their profile picture, making it difficult to align the 3D CT image evenly when positioning it in the side view. Therefore, for each case, the 3D soft tissue image of the CT scan was aligned to be on the same profile plane as the side-view photographs. The RP was then set on the side soft tissue images in the same way as it did on the side-view photographs.
This study showed tendencies in the discrepancies between the locations of the depressions on the soft tissue and bone. Applying the transverse and vertical distances measured from a bone image of the CT scan onto a patientŌĆÖs face at the indicated RP will be helpful for predicting the reduction location. Nonetheless, this study has limitations, and it will be necessary to conduct further research with a larger sample size and more accurate and consistent measurements methods between the soft tissue images of 3D CT and photography, including even alignment of different angles, the correction of size differences, and the determination of a constant RP.