Residual foreign body inflammation caused by a lumber beam penetrating the facial region: a case report
Article information
Abstract
Penetrating wounds to the face are cosmetically devastating and can be life-threatening. If the foreign body causing the penetrating wound is a piece of wood, small remnants might be left behind after the initial treatment. A 33-year-old male patient presented to the emergency center after a piece of lumber pierced his face as a passenger in a traffic accident. The patient’s vital signs were stable, and emergency surgery was performed to remove the foreign body and repair the soft tissue. No noteworthy complications were seen after open reduction and internal fixation of the facial bone fractures. Seven months after the accident, the patient underwent scar revision along with full-thickness skin grafting for post-traumatic scars. After the surgery, pus-like discharge which was not previously present was observed, and the graft did not take well. A residual foreign body, which was the cause of graft failure, was found on computed tomography and the remaining foreign body was removed through revision surgery. The patient is receiving outpatient follow-up without any complications 6 months after surgery. This case demonstrates the importance of performing a careful evaluation to avoid missing a residual foreign body, especially if it is of wooden nature.
INTRODUCTION
Penetrating wounds to the face are cosmetically devastating and life-threatening injuries that often necessitate emergent management [1,2]. X-ray, ultrasonography, and computed tomography (CT) can be used to identify remaining foreign bodies requiring removal, but some foreign bodies may be difficult to detect depending on their type or size [2,3].
In penetrating wounds, organic materials such as wood provide a more favorable environment for microorganisms to grow than metal materials, and are highly likely to cause infection and inflammation [2,4,5]. Therefore, it is important to remove the residual foreign body through a comprehensive and multidisciplinary approach in patients with penetrating wounds caused by organic materials. Through this case, we would like to emphasize the importance of detection and complete removal of residual foreign bodies from penetrating injury patients by presenting a case report of facial penetration caused by a piece of lumber.
CASE REPORT
A 33-year-old male patient was admitted to the emergency room as a passenger in a traffic accident. The accident occurred when the car he was in was hit by a truck loaded with lumber from behind, and a piece of wood penetrated the patient’s face from the right cheek to the infraorbital region (Fig. 1). The lumber that injured the patient was 5×5×100 cm. At the time of admission to the emergency room, the part that penetrated the face was still present, so it had to be shortened with a saw to shorten to 5×5×30 cm. The patient was alert and his vital signs were stable. Active bleeding from the penetrating wound was not observed.

A Photograph of the patient at the time of admission to the emergency room. A 5×5×100 cm beam of lumber pierced the face.
The initial CT scan showed comminuted fractures from the naso-orbito-ethmoid complex to the zygomaticomaxillary complex on the right side. Additionally, a wooden foreign body with low attenuation similar to air was observed (Fig. 2A and B).
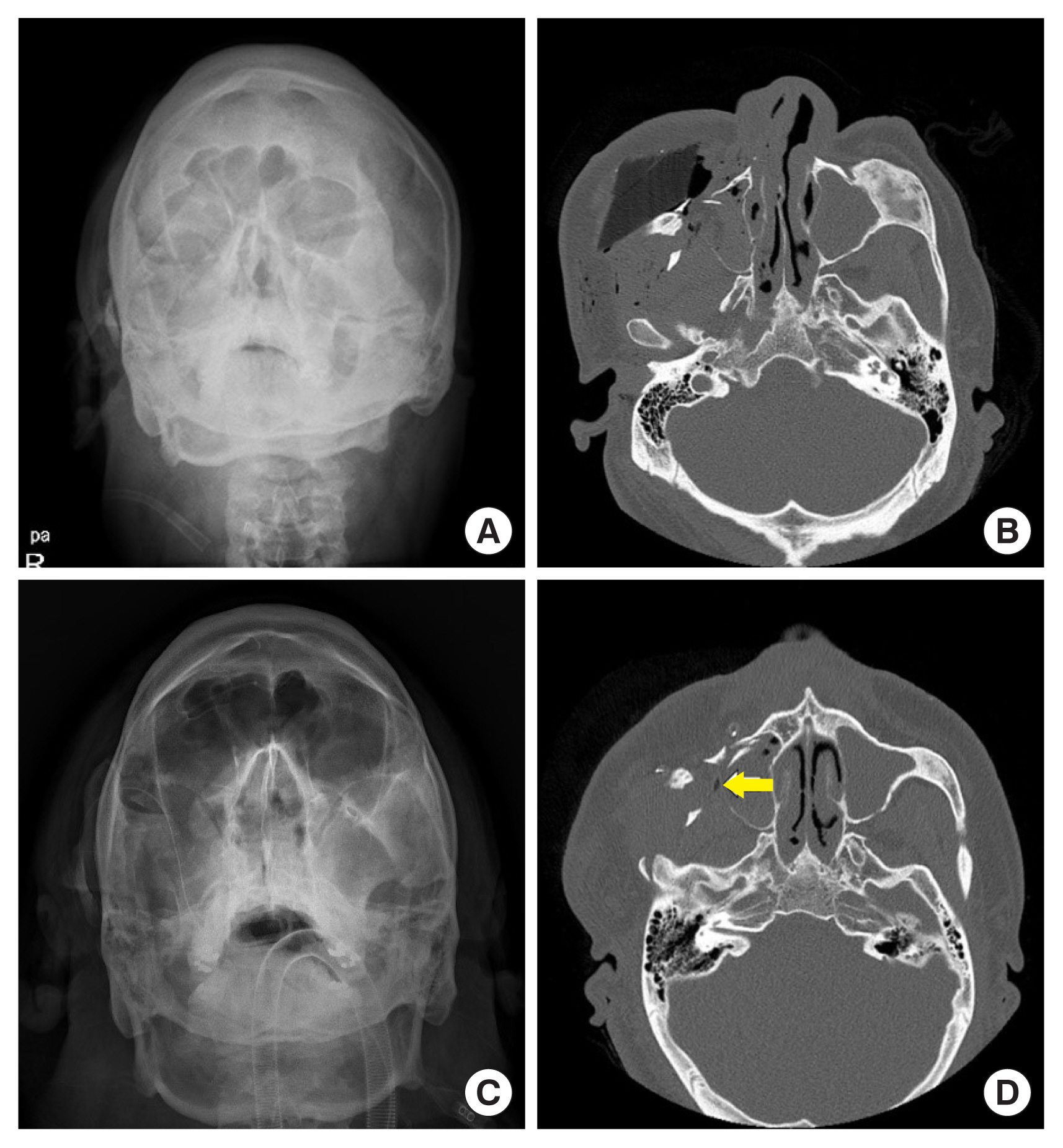
Computed tomography (CT) and simple radiography images of the patient before and after foreign body removal surgery. (A) Simple radiography image before surgery. (B) Axial CT image before the surgery. (C) Simple radiography image after surgery. (D) Axial CT image after surgery showing the residual foreign body, which was confused with an air shadow (yellow arrow).
We decided first to conduct wound exploration through emergency surgery and to remove the lumber and repair the soft tissue. After confirming that there were no signs of infection or inflammation due to a residual foreign body, we performed open reduction and internal fixation as a secondary operation.
The piece of lumber was removed during emergency surgery, along with plastic fragments presumed to be parts of eyeglass frames. Massive irrigation and bleeding control were conducted, and absence of any remaining foreign body was confirmed visually. After wound exploration the following structures were found to be injured: the buccal branch of the facial nerve, the supraorbital nerve, the supratrochlear nerve, both lacrimal canaliculi and a portion of the parotid gland. These structures were repaired primarily. For extensive lacerations extending from the forehead to the right cheek, primary closure was carried out after debridement. On the right eyelid, an artificial dermal graft (Pelnac) was placed on a 1.5×3 cm skin defect caused by avulsion. Based on the CT images taken immediately after surgery and the intraoperative findings the authors concluded that no foreign body was left (Fig. 2C and D).
After consultation with the department of infectious diseases an empirical antibiotics regimen was selected and started before the emergency surgery. Ceftriaxone (2 g) was intravenously administered every 24 hours and metronidazole (500 mg) was intravenously administered every 8 hours. This regimen was maintained for 7 days after surgery.
Ten days after surgery, normal results were obtained for C-reactive protein and blood panels including a complete blood count, coagulation test, electrolytes, liver function, and muscle enzyme tests. Surgical fixation for the facial bone fractures was carried out because there were no signs of inflammation, such as erythematous swelling, tenderness, or turbid discharge at the trauma site. Inferior orbital wall fracture was reconstructed using an absorbable mesh plate and screws, and open reduction and internal fixation were performed on the zygomaticomaxillary complex fracture using a titanium plate and screws. The nasal bone fracture was reduced in a closed manner. A skin defect of the right upper eyelid, which had been covered with a Pelnac artificial dermal graft in the previous emergency surgery, was covered with a full-thickness skin graft from the left postauricular area. The wounds healed without any complications, and the patient was discharged from the hospital.
During outpatient follow-up, an ectropion was observed due to cicatricial contracture of the right lower eyelid, and we decided to perform corrective surgery about 7 months after the trauma (Fig. 3). Scar revision was carried out for depressive scars from the forehead to the right eyebrow. After excision of the hypertrophic scar from the right lower eyelid to the cheek, a full-thickness skin graft from the left supraclavicular area was used.
During removal of the tie-over dressing on the 4th day after surgery turbid discharge flowed from the underside of the graft. Even though all blood test results were normal during close observation with daily dressing, no improvement was observed. We decided to localize the abscess tract with ultrasonography and enhanced facial CT. Ultrasonography showed an abscess pocket measuring about 1×3 cm in the subcutaneous fat layer. The enhanced facial CT revealed an abscess tract and a residual foreign body in the right masticator space (Fig. 4A). During surgical exploration the residual foreign body was removed (Fig. 4B). After massive irrigation it was confirmed that no foreign body had remained. Subsequently, the patient recovered without any turbid secretion or signs of inflammation. The patient remained free of complications during 6 months of outpatient follow-up.

Photographs of the residual foreign body. (A) On an enhanced facial computed tomography image, an area of high attenuation was observed, corresponding to a residual foreign body in the right masticator space (yellow arrow). An abscess pocket of about 3 cm in size was seen (white arrowhead). (B) Residual foreign body removed.
DISCUSSION
A penetrating facial injury due to a foreign body can pose a very challenging problem and requires a comprehensive and thorough evaluation. The causes for such an injury can be iatrogenic or they can be caused by traffic accidents, gun accidents, and other traumas. When encountering a patient with a penetrating facial injury, the first step in the management is to examine the wound meticulously. The next step is to remove the foreign body, conduct sufficient debridement and repair the soft tissue. Bone fixation is necessary if a fracture is present. Infection control by using appropriate antibiotics is also a key to success [1,2,6,7]. The treatment is complemented by appropriate resuscitative management (e.g., volume replacement and securing the airway) along with an evaluation of bleeding and airway obstruction [2].
The types of foreign bodies are very diverse, such as glass, organic materials, knives, stones, and metallic materials. A wooden foreign body is more likely to break into small pieces than a metal material, and small pieces of wood may easily remain in the body and cause complications. In addition, the porosity of wood creates a favorable environment for microorganisms to grow. Foreign bodies that are not removed cause chronic inflammation and infection, which can lead to tunneling wounds or sinus tracts. Therefore, it is important to carefully examine whether remaining foreign substances are present through imaging tests before and after surgery [2,5,6].
There is no established imaging method, but various imaging techniques can be used. Simple radiography may not be of much help for this purpose due to the radiolucent nature of wood. Ultrasonography can be used to detect foreign bodies hidden in soft tissue, but its accuracy may be affected by the skill of the practitioner, the depth at which the foreign body is located, and edema of the tissue around the foreign body [2,3,5,7]. On a CT scan, wood can be seen with low attenuation, similar to air, due to its porosity in the early stages of trauma. Therefore, it is easy to confuse with emphysema. In the chronic phase, the cellulose matrix accumulates in the wooden foreign body and it can be seen with high attenuation [5,8]. Immediately after surgery, the authors thought that the foreign body had been entirely removed, but a small remnant of the foreign body was mistaken for air shadows, leading to a missed diagnosis (Fig. 2D). The residual foreign body, which was not removed at the time of the first operation, appeared as high attenuation on enhanced CT taken 7 months later due to fluid collection and inflammation of the surrounding tissues (Fig. 4A).
The authors missed the remaining foreign material, as the small wood chips showed low attenuation, similar to air, on the CT examination taken at the time of trauma. Additionally, during the follow-up period between open reduction and internal fixation surgery and scar revision surgery, the patient did not complain of any symptoms. As this case report exemplifies, in circumstances where it could be easy to interpret a foreign body as another material, such as air, close cooperation between the attending physician and a radiologist can help avoid misdiagnosis.
The patient did not develop any additional complications after the foreign body was removed by reoperation, but suffered physical, mental, and economic damage. Therefore, it is very important to establish a multidisciplinary management plan when a patient with an injury of this type first presents to the hospital.
Notes
Conflict of interest
Jun Ho Choi, Jae Ha Hwang, and Kwang Seog Kim are editorial board members of the journal but were not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Funding
None.
Ethical approval
The study was approved by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUH-EXP-2022-145).
Patient consent
The patient provided written informed consent for the publication and use of his images.
Author contributions
Conceptualization: Jun Ho Choi, Jae Ha Hwang. Project administration: Sang Seong Oh. Writing - original draft: Jae Ha Hwang. Writing - review & editing: Jae Ha Hwang. Investigation: Jun Ho Choi. Resources: Sang Seong Oh. Supervision: Kwang Seog Kim. Validation: Kwang Seog Kim, Sam Yong Lee.
Abbreviation
CT
computed tomography

