Surgical treatment of postauricular hidradenitis suppurativa with delayed diagnosis: a case report and literature review
Article information
Abstract
Hidradenitis suppurativa (HS) is a chronic inflammatory condition that is difficult to diagnose, with a period of 10.0±9.6 years from symptom onset to diagnosis. A 32-year-old Asian man presented with bilateral postauricular abscesses that first appeared 5 years previously. Despite several incisions and drainage, the symptoms only temporarily improved and continued to recur. On physical examination, chronic scars and sinus tracts were observed around the lesion. Postauricular HS was diagnosed, and surgical treatment was performed. We performed a wide excision and reconstructed the defect using a posterior auricular artery perforator-based keystone flap. Histological examination confirmed the diagnosis of HS. The reconstruction was successful, and there was no recurrence for 2 years after surgery. HS is difficult to diagnose without specific attention. Although the postauricular region is not a typical site of HS, it can occur in this area. Therefore, if a patient presents with recurrent abscesses in the postauricular region, HS should be considered. Additionally, if HS is diagnosed in the postauricular region, wide excision with reconstruction using a posterior auricular artery perforator-based keystone flap can lead to a favorable outcome.
INTRODUCTION
Hidradenitis suppurativa (HS) is a chronic inflammatory condition that affects apocrine gland-bearing areas of the body, causing relapsing and debilitating symptoms [1–4]. Despite the prevalence of HS, its exact pathogenesis is not fully understood. Nevertheless, it is believed to be involved in follicular occlusion, immune dysregulation, and bacterial infection [1–4]. The most common presentation of HS includes the formation of painful nodules, abscesses, and sinus tracts in the axillary, groin, and anogenital regions [1–4]. However, involvement of other sites, such as the postauricular region, is atypical and rare, and can often be misdiagnosed as infected epidermal cysts or furuncles. This can make diagnosis difficult, especially since the time from symptom onset to diagnosis is typically 10.0±9.6 years [5]. In this report, we present a case of postauricular HS that was diagnosed and treated surgically after a 5-year delay in diagnosis. Our aim is to highlight the importance of the early recognition and diagnosis of HS, especially in atypical cases, to prevent unnecessary morbidity and improve patient outcomes.
CASE
A 32-year-old Asian man with no underlying medical conditions presented to our clinic with bilateral postauricular abscesses (Fig. 1). The patient reported experiencing abscesses in the bilateral postauricular area approximately 5 years previously, which were treated with I&D at a different hospital and improved. However, since then, the patient experienced multiple recurrences of abscesses, with temporary improvement after drainage, followed by relapse after a few months.

Initial photographs. A 32-year-old man with recurrent abscesses in the bilateral postauricular areas. (A) Left side. (B) Right side.
Upon initial presentation to our department, the patient had abscesses in both postauricular areas. We suspected infected epidermal cysts and performed I&D, which resulted in symptom improvement. However, 2 months later, the patient presented with an abscess near the previous lesion (Fig. 2). On physical examination, chronic scars and sinus tracts were observed around the lesion.

After incision and drainage. Postauricular chronic inflammatory lesion and scar. (A) Left side. (B) Right side.
The patient was diagnosed with Hurley stage 2 hidradenitis suppurativa of the bilateral postauricular area, and curative surgical treatment was planned. We performed a wide excision of the lesion under general anesthesia and covered the defect with a posterior auricular artery perforator-based keystone flap. We used handheld Doppler ultrasonography to identify posterior auricular artery perforators and carefully designed the keystone flap to avoid hairline deformity (Fig. 3). The surgery was uneventful, and the defect was successfully covered with the flap.
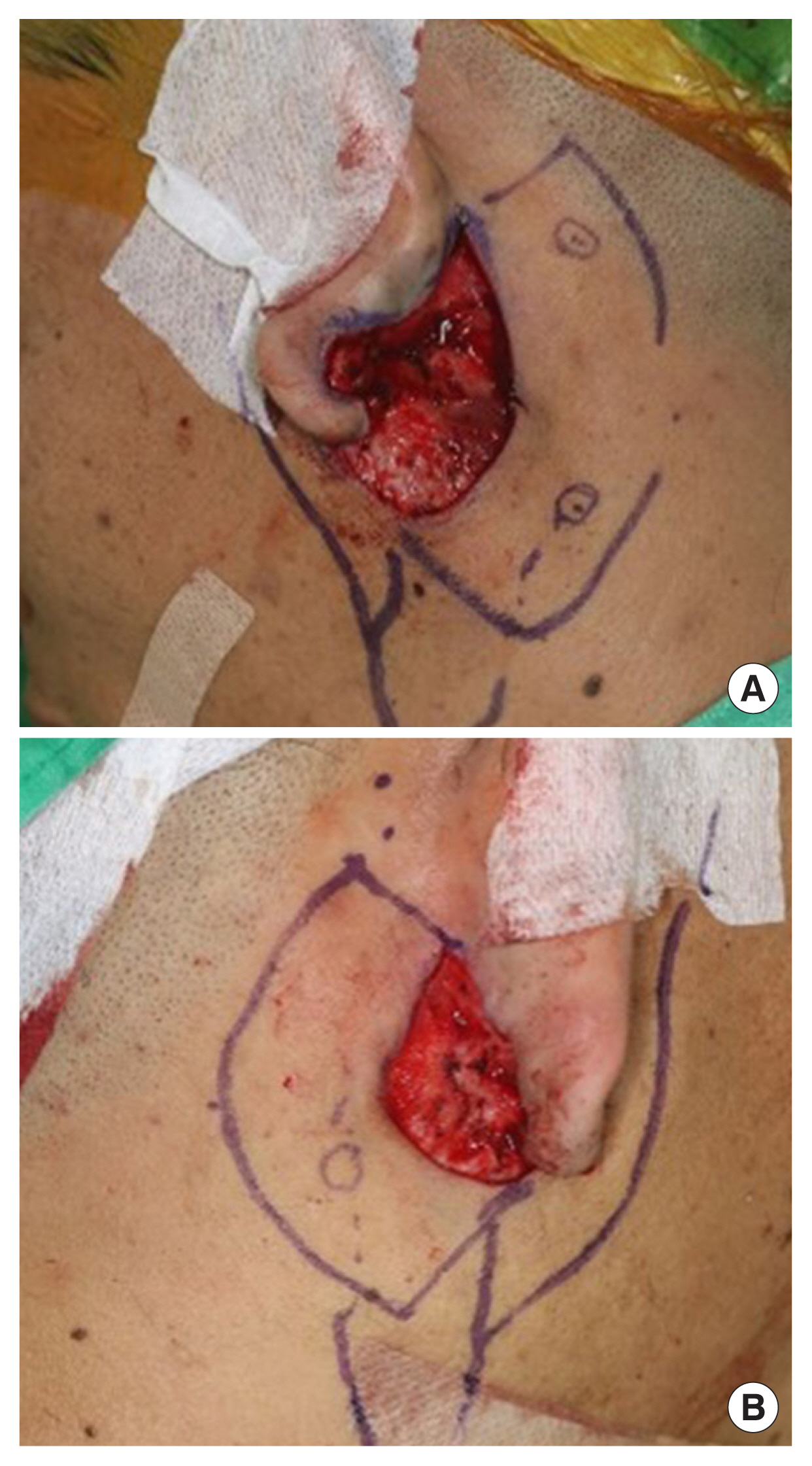
Intraoperative photographs. Wide excision was performed and defect was covered with a posterior auricular artery perforator-based keystone flap. (A) Left postauricular area. (B) Right postauricular area.
Histological examination of the excised lesions revealed chronic inflammation and dilated hair follicles with degenerated keratin. Based on the histological results and clinical symptoms, the diagnosis of HS was confirmed. There were no wound complications after surgery, and the patient did not experience recurrence for 2 years (Fig. 4). Additionally, the cosmetic outcome was good, with no disturbance of the hairline.
LITERATURE REVIEW
HS is a chronic inflammatory disease that affects the folliculopilosebaceous unit [2]. It primarily affects areas with abundant apocrine glands, such as the axilla, groin, and anogenital region [1–4,6]. The common factor among these regions is the occurrence of skin folds, which are known to be associated with the development of HS. Folding of the skin contributes to the obstruction of the follicular opening, which can lead to the development of HS [2–4,6]. The postauricular region can also be considered a susceptible site for HS from this perspective, although it is not commonly recognized as a typical location for HS.
The symptoms of HS may include painful and inflamed nodules, abscesses, and sinus tracts in the affected areas [1–4,6]. The affected skin may also appear red, be tender to the touch, have a foul odor, and discharge pus or blood [1,3,4]. The Hurley staging system is commonly used to classify the severity of the disease, with stage I indicating single or multiple abscesses without sinus tracts or scarring, stage II indicating recurrent abscesses with sinus tracts and scarring, and stage III indicating diffuse involvement with multiple interconnected sinus tracts and abscesses [2,6].
HS is more common in women than in men and typically develops after puberty. It affects about 1% to 4% of the population, with a higher prevalence in individuals with a family history of the disease, obesity, smoking, and metabolic syndrome [2,4,6]. Approximately 75% of all HS patients have obesity. Loss of 15% of body weight can result in complete remission in approximately 50% of patients, and symptoms improve in 20% of patients [7]. It is known that the incidence of HS is 1.5 to 3 times higher in patients with type 2 diabetes or polycystic ovarian syndrome [2].
The pathogenesis of HS is not yet fully understood; however, it is hypothesized to involve dysregulated immune responses to bacterial antigens in genetically predisposed individuals, resulting in perifollicular inflammation [2–4,6]. This is accompanied by hyperkeratinization of the follicular epithelium, leading to the formation of a keratin plug that obstructs the follicular opening [2,6]. As a result of this obstruction, the follicle dilates and eventually ruptures, leading to the release of intrafollicular debris into the surrounding dermis and propagating an inflammatory response [2,6]. As inflammation progresses, ruptured follicles may become interconnected, resulting in the development of sinus tracts or fistulas and the persistence of chronic inflammation [2–4,6]. Therefore, HS exhibits histological features such as follicular plugging, perifollicular lymphocytic inflammation, and the formation of deep dermal sinus tracts lined by granulation tissue due to the interconnected ruptured follicles and chronic inflammation.
The diagnosis of HS can be challenging and requires a combination of clinical history and physical examination [2,3,5]. While a tissue biopsy can confirm the diagnosis, HS can often be diagnosed without the need for biopsy due to the clear visual appearance of the condition. Early diagnosis can be achieved through a thorough patient history and physical examination. Delayed diagnosis can result in a poorer quality of life for patients and larger lesions that are more difficult to treat [5]. Therefore, it is crucial to have a high level of suspicion and make an early diagnosis. Previous studies have shown that an average of 10.0±9.4 years elapse from symptom onset to diagnosis [5]. Furthermore, HS is diagnosed by dermatologists in approximately 80% of cases, whereas the diagnosis by surgeons is less than 10% [5]. The low diagnosis rate by surgeons despite many patients presenting with recurrent abscesses suggests a lack of awareness of HS among surgeons. Showing an interest in the patient and making an early diagnosis can greatly improve their quality of life and prognosis.
Effective management of HS requires both medical and surgical treatment. Various drugs are used for medical treatment, depending on the symptoms and severity. These include systemic antibiotics, hormone therapy, steroids, and biological treatment. Antibiotic therapy typically involves the administration of tetracyclines, clindamycin, or rifampicin, which may be adjusted based on culture data. In severe cases of Hurley stages 2 and 3, intravenous ertapenem is used in combination [2,3, 6,8]. Hormone therapy may involve the use of oral contraceptives, which can improve symptoms in Hurley stage 1 patients [2,6]. Steroids can be administered by intralesional injection or orally [2,6]. Biologics, such as adalimumab or infliximab, are often used and both suppress tumor necrosis factor-α [2,6]. However, relying only on drug therapy requires continuous treatment to maintain remission, and discontinuing medication can result in relapse. In addition, long-term drug therapy can cause serious adverse effects. If the lesions are too large for wide excision and coverage, drug therapy should be considered. However, if lesions are small, early surgical intervention is crucial for successful treatment.
Surgical treatment of HS includes I&D, surgical unroofing, or wide excision [2,8]. Performing only I&D is known to result in almost 100% recurrence; therefore, relying only on I&D is not recommended [9]. In Hurley stage 1, surgical unroofing can be attempted. Using a 5- to 7-mm punch biopsy instrument or carbon dioxide laser, the roof of the chronic sinus tract is debrided, and the defect is treated with secondary intention [2]. However, complete removal of the roof of the deep interconnecting sinus tract is difficult, leading to a risk of recurrence [2].
For complete treatment, all the affected skin must be removed and replaced with healthy skin [2,10]. Therefore, the treatment of choice for HS involves wide excision followed by reconstruction using skin grafting or skin flap surgery using healthy tissue. Partial-thickness skin can be harvested from excised HS lesions for grafting [2]. This is known as the reused skin graft technique since the folliculopilosebaceous unit that causes HS is not included in partial-thickness skin, avoiding additional donor site injury [2].
DISCUSSION
The patient in this case had recurrent abscesses for 5 years. He underwent multiple I&D procedures for a long time. However, due to the frequent recurrence, he was experiencing a great deal of hardship and exhaustion. He was unable to continue his job while receiving treatment, so he quit and started his own business. Showing an interest in the patient and making an early diagnosis can greatly improve their quality of life and prognosis.
In this case, we considered cosmetic factors when reconstructing the defect to ensure stable coverage without affecting the hairline. Therefore, we used a keystone flap based on a posterior auricular artery perforator for reconstruction [11,12]. The keystone flap is easy to perform and is suitable for reconstructing large areas while preserving the hairline [13,14]. Additionally, we maintained a skin bridge on the greater arc of the keystone flap, known as the Sydney melanoma unit modification [15]. This maintains the flap’s stability and improves its survival. However, even if the skin bridge is not maintained, if posterior auricular artery perforator is well secured, it is expected to have no effect on flap survival.
HS can be difficult to diagnose without specific attention. Although the postauricular region is not a typical site of HS, it can occur in this area. Therefore, if a patient presents with recurrent abscess in the postauricular region, HS should be considered. Additionally, if HS is diagnosed in the postauricular region, wide excision with reconstruction using a posterior auricular artery perforator-based keystone flap can lead to a favorable outcome.
Abbreviations
HS
hidradenitis suppurativa
I&D
incisions and drainage
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The report was approved by the Institutional Review Board of Dongguk University Hospital (IRB No. 110757-202207-HR-06-02).
Patient consent
The patient provided written informed consent for the publication and use of his images.
Author contributions
Conceptualization: Inho Kang. Data curation: Inho Kang, Joon Ho Lee. Formal analysis: Inho Kang. Supervision: Joon Ho Lee, Gyu Yong Jung. Writing - original draft: Inho Kang. Writing - review & editing: Inho Kang, Gyu Yong Jung, Min Jun Yong, Yujin Ahn, Joon Ho Lee.
Funding
None.

