INTRODUCTION
Mandibular fractures account for 40% to 62% of facial bone fractures, and over 50% of mandibular fractures involve multiple breaks [
1]. Mandibular fractures are typically classified based on the location of the fracture, the condition of the teeth surrounding the fracture line, and the direction of the fracture line. The anatomical location of the fracture is often used for classification purposes. Generally, the condyle and body regions are the most common sites for mandibular fractures, although variations may occur depending on the specific report. The diagnosis is usually made through a combination of a clinical evaluation and imaging tests. Given the diverse severity and patterns of fractures, patients may not always present clear symptoms, making imaging tests essential for an accurate diagnosis. Historically, panoramic imaging has been viewed as the gold standard for diagnosing mandibular fractures, providing excellent diagnostic results [
2]. Computed tomography (CT) has recently been acknowledged as the preferred diagnostic tool due to its high accuracy [
3]. However, despite the increasing availability of CT scans for suspected mandibular fractures at well-equipped medical facilities, obtaining CT scans remains a significant challenge in many countries, especially in developing nations. This is due to factors such as the high costs of CT equipment and the financial burden on patients [
4,
5].
This study focused on mandibular split (greenstick) fractures, which represent an unusual fracture pattern limited to the lingual cortex of the mandible. To date, only two case reports have been published worldwide [
6,
7], and there is a lack of other specialized studies or reports in this area. Therefore, the aim of this report was to enhance cliniciansŌĆÖ understanding of mandibular split fractures, improve diagnostic accuracy, and contribute to future research.
This study included a total of six patients. Their clinical features, the distribution and direction of the fracture line, and the diagnostic accuracy of split fractures using CT and panoramic imaging were examined and compared.
METHODS
In this study, we conducted a retrospective review of medical records for six patients who visited our hospital between January 2020 and June 2023 and were diagnosed with mandibular split fractures. They were chosen from patients who initially presented with a mandibular fracture and had visited either the plastic and reconstructive surgery department or the emergency room. From patientsŌĆÖ records, we collected information on age, sex, symptoms, mechanism of trauma, the location of the fracture line as observed on CT and panoramic images, number of fractures, impact site, presence of concomitant injuries, and treatment status (surgical or non-surgical). Additionally, we estimated the frequency of mandibular split fractures by comparing the number of these patients to the total number of patients diagnosed with mandibular fractures during the same study period.
RESULTS
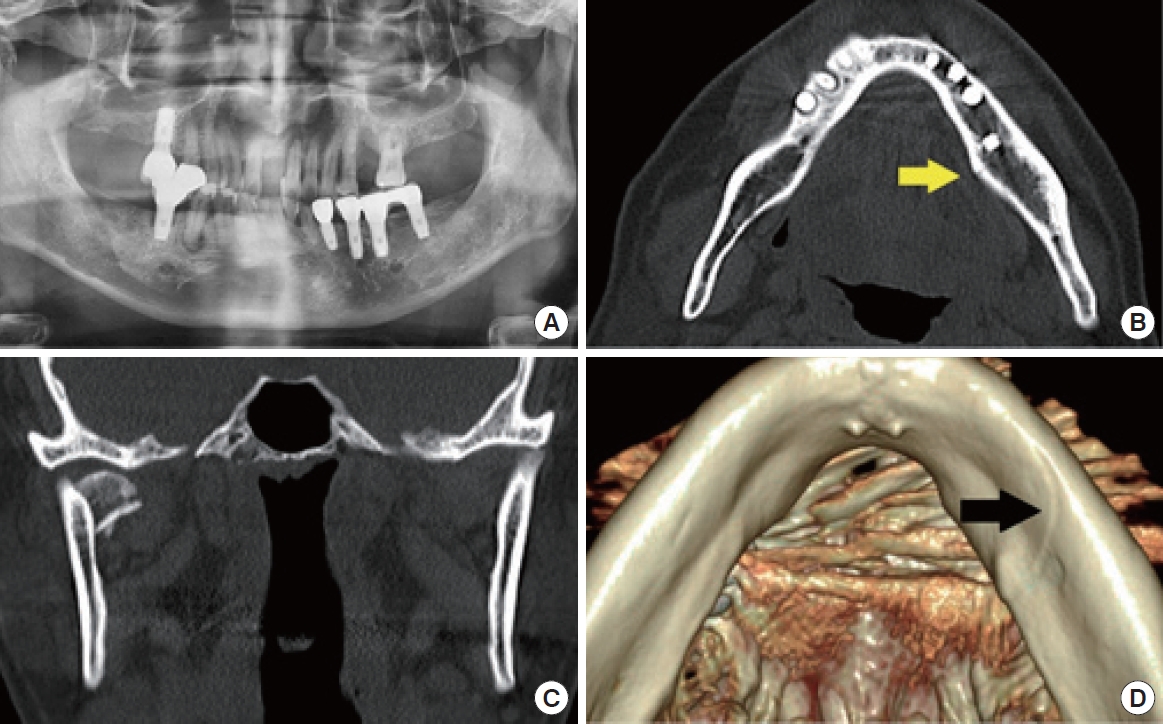
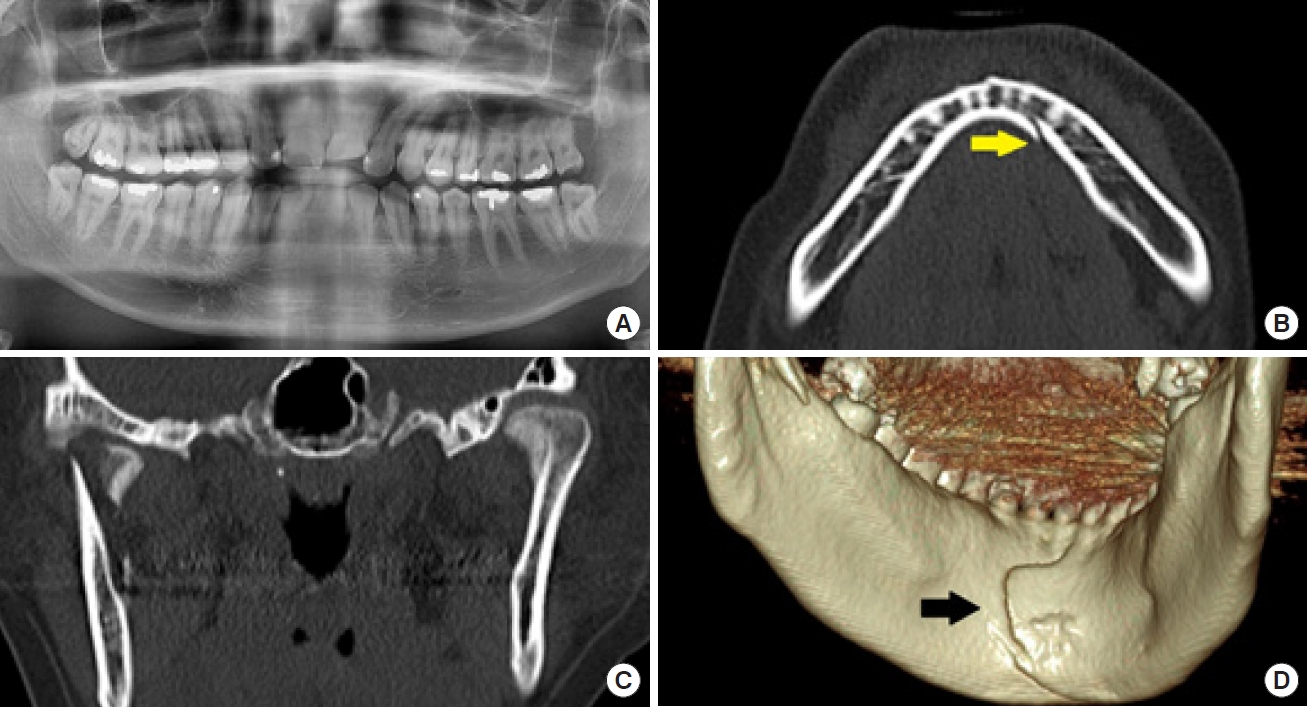
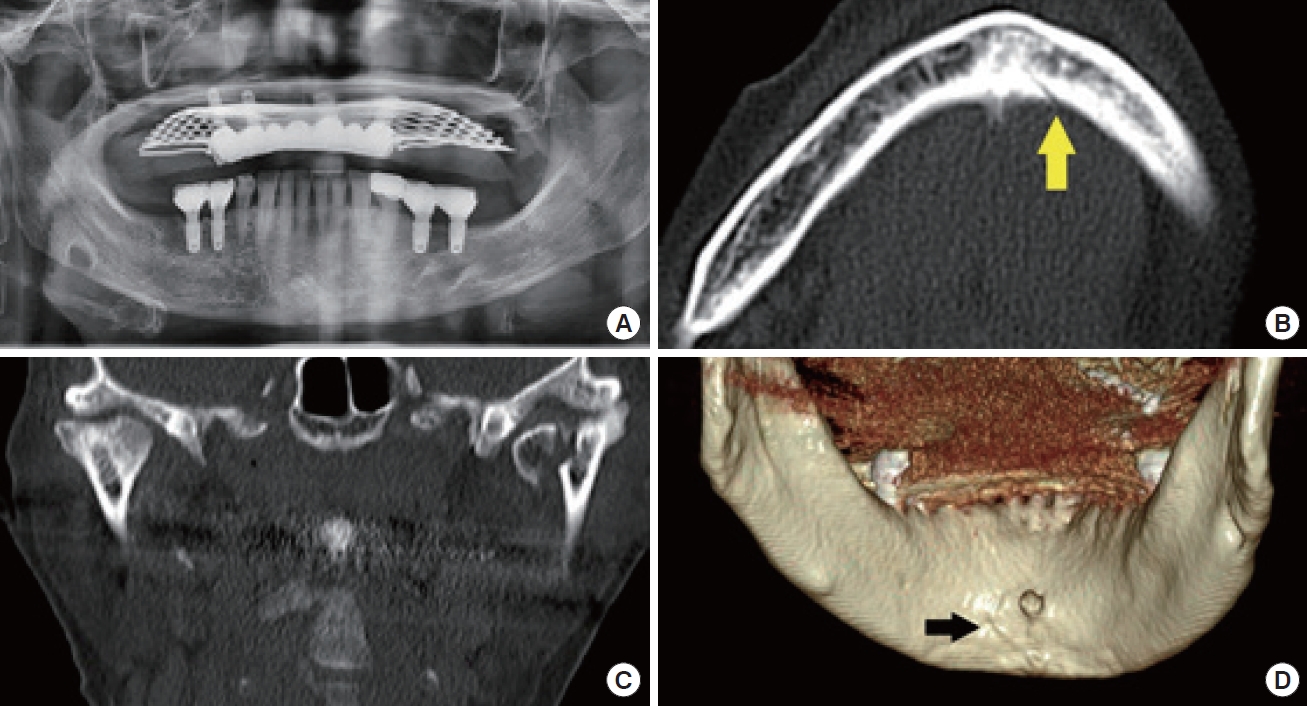
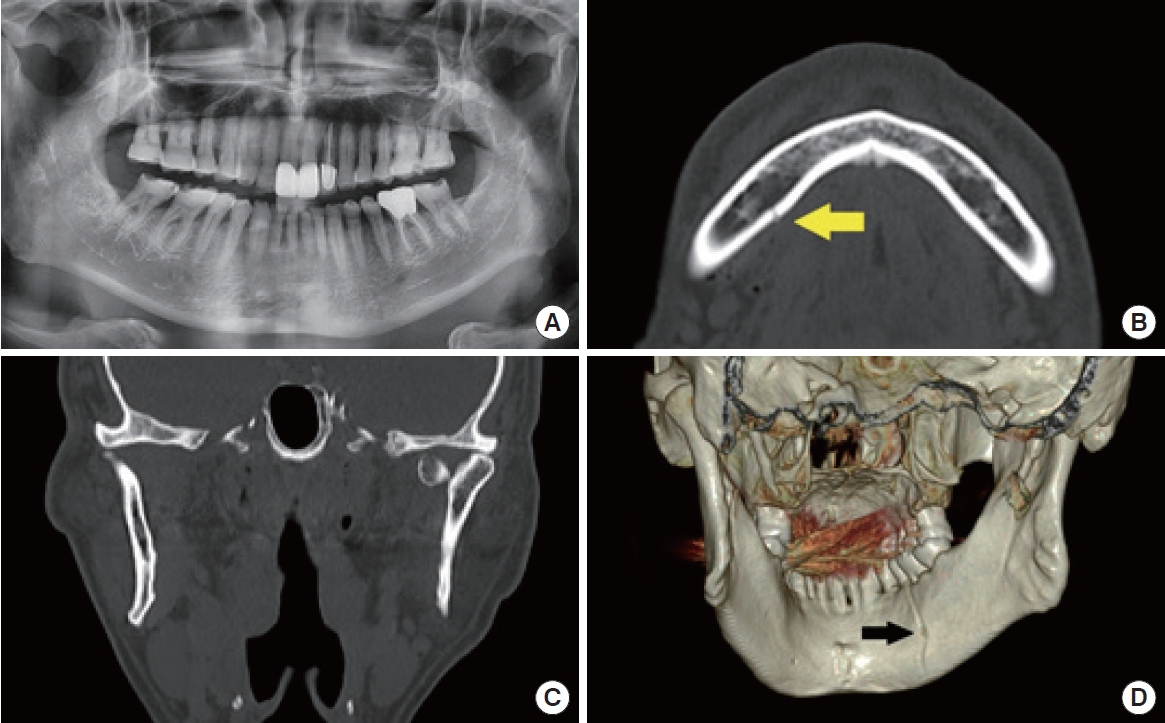
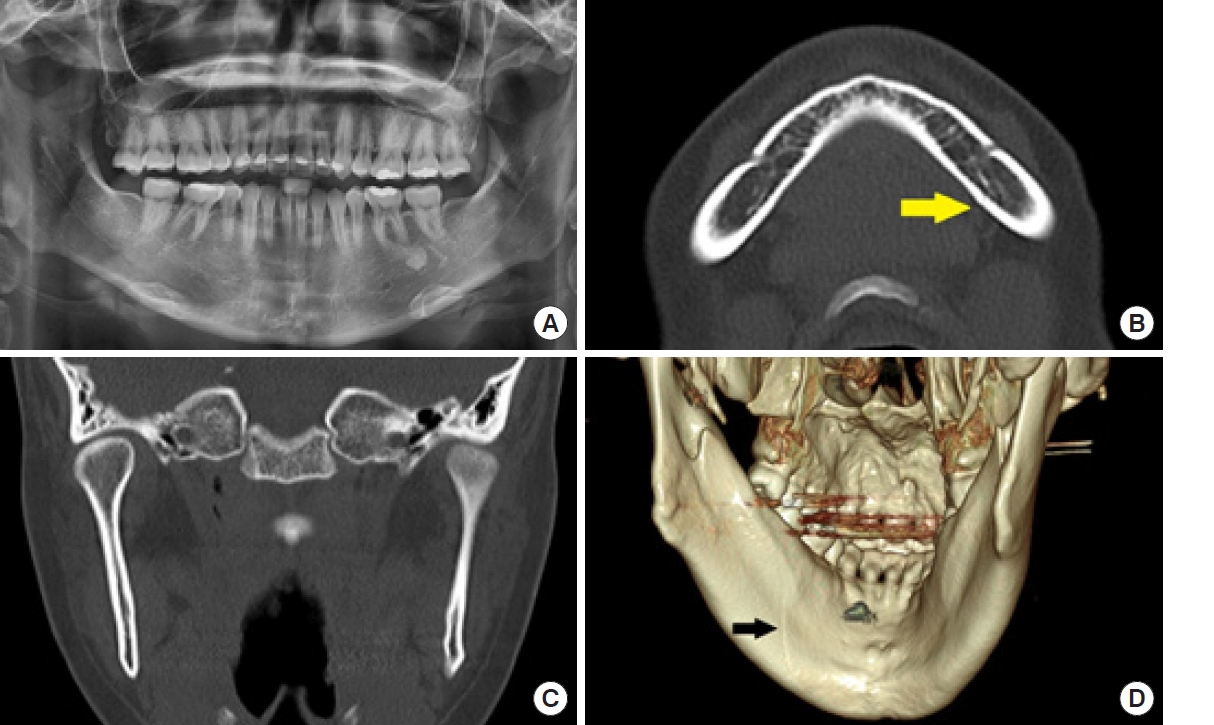
In all six patients diagnosed with mandibular split fractures, the fracture line was not readily apparent on panoramic radiography, but was definitively confirmed using CT scans and three-dimensional (3D) reconstructed images (
Figs. 1-
5). The ages of the patients varied widely, ranging from 20 to 71 years (20, 25, 28, 60, 69, and 71), with a mean age of 49.8 years. The sex distribution was equal among the patients, with three men (50%) and three women (50%). The majority of the patients (4/6, 66.7%), sustained their injuries from slip-and-fall incidents. The remaining two patients (33.3%) were injured in collisions with another vehicle while riding a motorcycle.
The locations of the split fractures were as follows: symphysis in one patient (16.7%), symphysis to parasymphysis in two patients (33.3%), parasymphysis in one patient (16.7%), and parasymphysis to the body in two patients (33.3%). The fracture pattern observed was vertical in three patients (50%), oblique in two patients (33.3%), and omega in one patient (16.7%) (
Figs. 1-
5). Of the six patients, four (66.7%) presented with condylar head fractures, with one of these patients (16.7%) having fractures in both condylar heads. In two patients (33.3%), split fractures were the only type of fracture present.
All six patients presented with facial lacerations. Three patients (50%) had lacerations confined to the chin, while two patients (33.3%) had multiple lacerations on both the chin and lips. The remaining patient (16.7%) had multiple lacerations on the chin, lips, and philtrum. In five cases (83.3%), the lacerations were deep enough to expose bone, whereas the remaining case involved a subcutaneous laceration. Regarding the location of the lacerations on the mandible, five patients (83.3%) had lacerations on the lower middle part of the jaw, and one patient (16.7%) had a laceration slightly to the left of the center in the anterior region. Two of the six patients (33.3%) also had tooth damage, including fractured molars. None of the six patients had lacerations in the oral cavity, bruises, or hematomas.
Based on patient reports and clinical observations, we determined whether occlusion was normal or abnormal. We observed malocclusion in three patients (50%) who had condylar head fractures. The other three patients (50%), including one with a left intracapsular condylar head fracture, exhibited normal occlusion. All six patients reported pain and tenderness in the temporomandibular joint (TMJ) following their injuries, and they had a limited mouth opening range of 2 to 3 cm. In the two patients (33.3%) with isolated split fractures, TMJ pain subsided after 7 to 10 days, and they regained near-normal mouth opening. Tenderness on the lingual side, which was suspected to be associated with the split fractures, persisted for approximately 2 weeks in most patients.
Of the six patients, two (33.3%) who were involved in motorcycle accidents had significant concomitant injuries. These patients required treatment from the departments of neurosurgery, trauma surgery, and thoracic surgery.
Four patients (66.7%) underwent intermaxillary fixation (IMF) and rubber traction using IMF screws, followed by early exercise after a 2-week period. Two patients (33.3%) were treated conservatively, which included dietary restrictions, for a duration of 4 weeks. Following a treatment period of 4 to 5 weeks, all six patients achieved normal occlusion. However, a slight deviation in mouth opening was observed in one patient who had a right condylar head fracture (
Table 1).
All six patients underwent CT and panoramic imaging simultaneously at the time of injury, and we compared and analyzed the findings from both modalities. CT scans successfully diagnosed split fractures in all patients, providing clear visualization on axial and coronal views, with even greater clarity on 3D images. However, panoramic images failed to reveal any fracture lines in four of the patients. In the remaining two patients, a potential fracture line was detected, but its visibility was not clear.
During the study period, our hospital diagnosed a total of 108 patients with mandibular fractures. Of these cases, 5.6% were identified as split fractures.
DISCUSSION
Mandibular fractures are significant in the field of plastic surgery, accounting for 40% to 62% of facial bone fractures [
1]. Since the mandible is the only mobile bone in the face due to the presence of the TMJ, it requires accurate diagnosis and treatment to ensure normal daily functioning without complications, such as malocclusion or restrictions in mouth opening.
This study aimed to enhance our understanding of mandibular split (greenstick) fractures in adults, which are poorly understood at present, by reviewing the clinical characteristics and imaging findings of patients diagnosed with this distinctive fracture pattern. To the best of our knowledge, only two cases of mandibular split fractures in adults have been reported worldwide. Sever et al. [
6] reported a case of a 26-year-old woman who experienced a split fracture of the mandible after an epileptic seizure, and Ersan and Ilguy [
7] reported a case of a 33-year-old woman who had a split fracture due to a fall. This is the first study to analyze multiple cases.
Approximately half of all mandibular fractures involve multiple breaks, with double fractures being the most prevalent. When force is applied to the chin, the resulting kinetic energy travels along the mandibular arch, causing a direct fracture at the point of impact and an indirect fracture at a weaker point on the opposite side [
1]. Therefore, after confirming a mandibular fracture, it is important to carefully assess whether there are fractures in other parts of the mandible. In this study, of the six cases of split fractures, four (or 66.7%) presented with double and triple fractures, including both condylar heads. The remaining two cases (33.3%) had only split fractures.
Mandibular fractures tend to occur more frequently in men, primarily due to interpersonal violence. Conversely, in women, these fractures are often the result of traffic accidents or falls [
3]. However, in this study, the male-to-female ratio was equal, with falls being the predominant cause of fractures. Taking into account the two previously documented cases, split fractures seem to be more prevalent in women, with slip-down incidents being the primary cause. This suggests a possible correlation between the relatively less intense impact on the mandible and the incidence of split fractures. The thickness of the mandibular cortex decreases after the age of 35 years [
8]. Yet, in this study, there appeared to be a minimal correlation between cortical thickness and split fractures, as patients in their 20s and those in their 60s and 70s exhibited similar fracture patterns.
All six cases involved chin lacerations, and in five of these cases (83.3%), the bone was exposed, yet the fracture line was not visible to the naked eye. The location and pattern of the lacerations, combined with physical examination findings of abrasions and swelling, indicated that the impact occurred around the jawŌĆÖs midline. In considering the primary impact site on the mandible, it was proposed that one patient (16.7%) experienced an impact from the middle anterior direction of the mandible, two patients (33.3%) from the inferior direction, and three patients (50%) from a direction between the anterior and inferior. Furthermore, if a deep laceration is present in the middle of the jaw and there is persistent tenderness on the lingual side, a split fracture should be suspected. It can be inferred that when a specific impact is applied from the anterior or inferior direction of the chin, split fractures may occur, and additional impact may result in condyle fractures. The correlation between the characteristics of the impact and fractures requires further research.
In four patients (66.7%), we performed a closed reduction, taking care to avoid exacerbating the fracture. We achieved IMF using IMF screws. Post-surgery, we corrected occlusion with a rubber band and initiated early exercise 2 weeks later. IMF screws have several benefits, including a shorter operation time, simpler procedure, and minimal discomfort for the patient during outpatient removal. Research has shown that IMF screws provide stability and malocclusion rates comparable to traditional arch bars [
9]. There are also reports of using N-2-butyl cyanoacrylate adhesive to correct pediatric zygomatic split fractures [
10]. Given the split interval, this adhesive could be a viable treatment option.
Until the early 2000s, panoramic imaging was considered the gold standard for diagnosing mandibular fractures. It had a diagnosis rate of 86% and was relatively inexpensive, making it a practical choice for tooth-related evaluations [
3,
11]. However, it is not advisable to perform CT scans indiscriminately due to the associated medical costs, radiation exposure, and the potential for artifacts caused by intraoral fillings [
2]. Despite these drawbacks, CT scans offer the advantage of viewing the mandible in axial, coronal, and sagittal views, and the ability to generate 3D composite images from these views. With a nearly 100% diagnostic rate, CT scans are a valuable tool in diagnosing mandibular fractures [
11,
12]. They are particularly useful in determining the location and direction of the fracture line, the degree and direction of displacement, as well as the degree of depression and rotation. This information is vital for both diagnosis and treatment planning. As a result, CT scans have become the preferred diagnostic tool in recent years [
3,
13]. In this study, CT and 3D composite images were crucial for diagnosing split fractures. CT scans clearly displayed split fractures on the posterior surface of the mandible in both axial and coronal views, while these fractures were not easily visible on panoramic images. If only condylar head fractures are diagnosed and surgical treatment is performed, there is a risk that force may be transmitted to the split fracture site during surgery, potentially exacerbating the split fracture. It is therefore important to consider the presence of split fractures and carefully plan the surgical approach to avoid worsening the fracture. Consequently, it is essential to perform CT scans, especially in cases of split fractures. Among these, 3D reconstruction images provide the most definitive diagnostic information. However, despite these trends, there are still situations where the use of CT for diagnosis is difficult due to disparities in medical environments. According to Prasad et al. [
4], only 15% of patients presenting with head and neck trauma in developing countries were able to undergo CT scans. Similarly, Ogunmuyiwa et al. [
5] highlighted the economic challenges of obtaining CT scans for facial fractures in developing nations. Nevertheless, this study revealed limitations in diagnosing mandibular fractures, particularly split fractures, through panoramic images. Even in regions with limited medical resources, it is recommended to utilize CT scans for cases with suspected mandibular fractures to improve diagnostic accuracy.
During the study period, six (5.6%) of the 108 patients diagnosed with mandibular fractures were found to have split fractures. Given the rarity of this fracture pattern, this frequency seems relatively high. This suggests that split fractures may have been previously overlooked or misinterpreted as artifacts resulting from dental fillings. It is important to observe mandibular fractures more closely in order to improve diagnostic accuracy. We anticipate further case studies and research to deepen our understanding of split fractures.